Back to 2024 Abstracts
A MULTICENTER INTERNATIONAL STUDY ON PATIENTS WITH T3 AND T4 CATEGORY OF GALLBLADDER CANCER: FINDING THE RIGHT BALANCE OF SURGICAL TREATMENT
Ariana M. Chirban
*1,2, Maria B. Rivera
3, Eduardo A. Vega
21University of California San Diego, La Jolla, CA; 2St. Elizabeth's Medical Center, Boston, MA; 3Clinica Alemana - Universidad del Desarrollo, Santiago, Chile
Background: Gallbladder Cancer (GBC) remains a challenging malignancy, with surgical resection as the sole curative option. However, optimal surgical treatment, as well as utilization of chemo- and radiotherapy for tumor category: T3 and T4, remains an area of continued debate.
Methods: An international cross-sectional retrospective study was performed on data collected from seven countries and 17 institutions between 1997-2020 regarding patients operated for GBC. Kaplan-Meier curves and Cox regression analyses were used to determine factors impacting overall survival (OS).
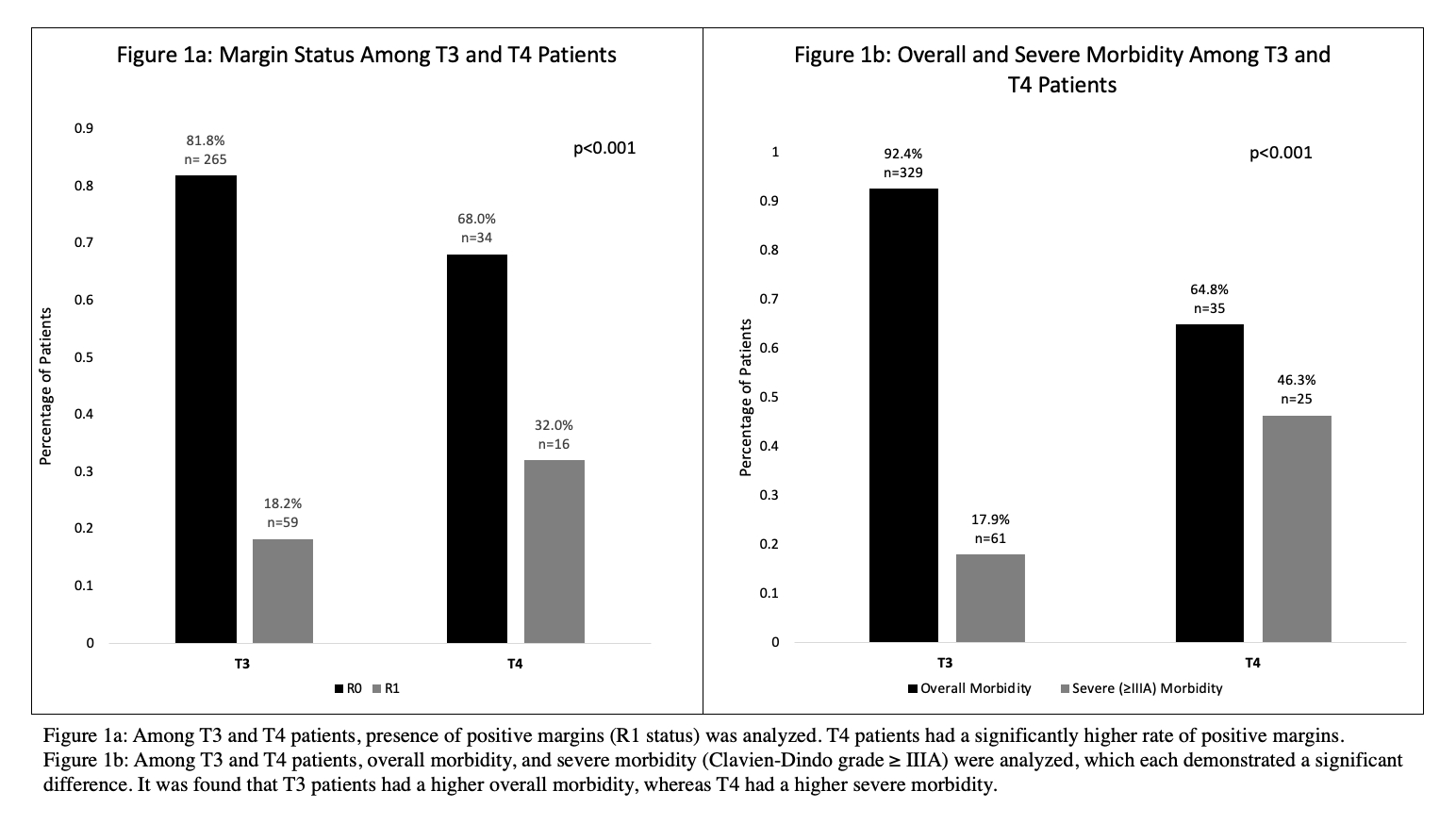
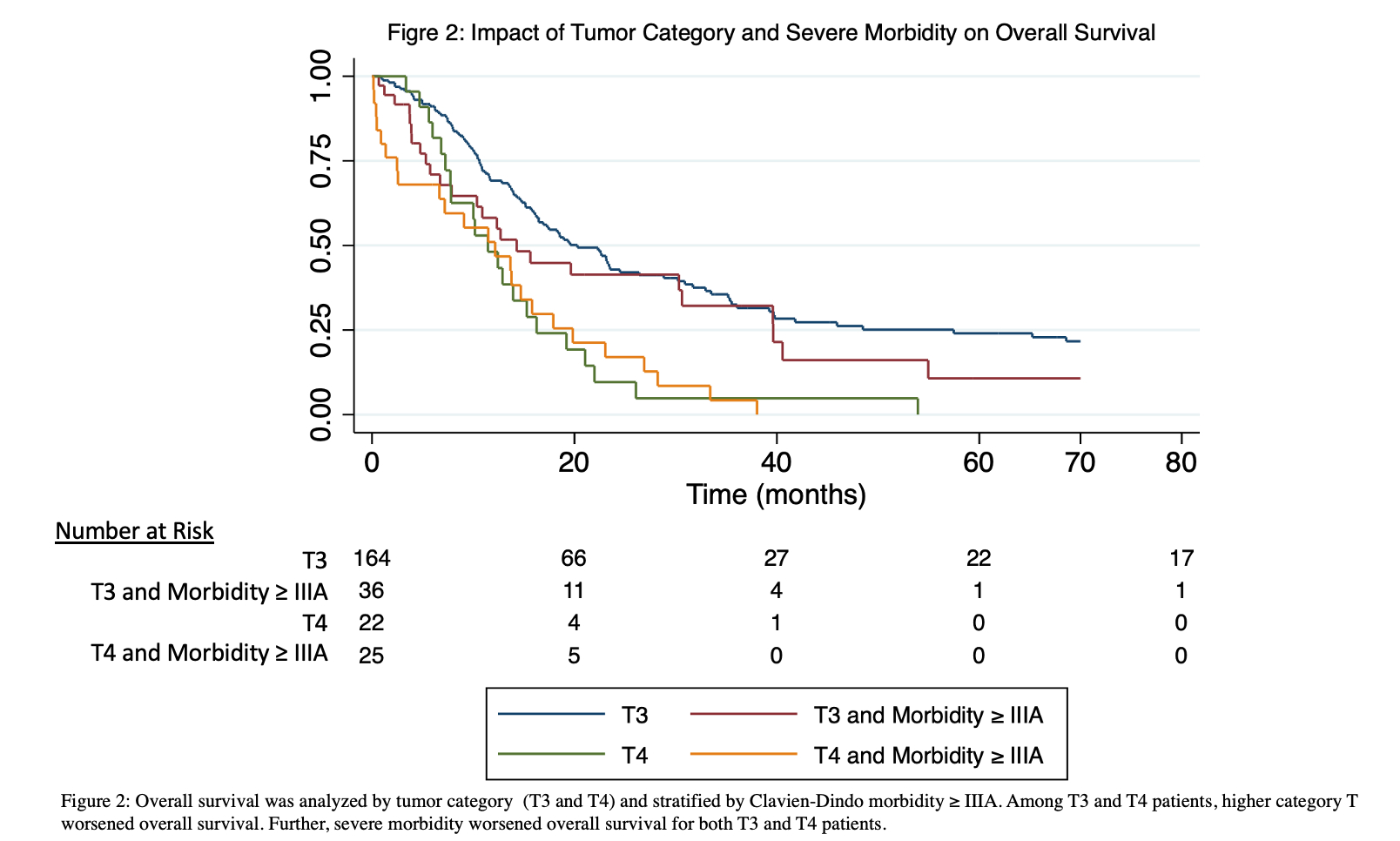
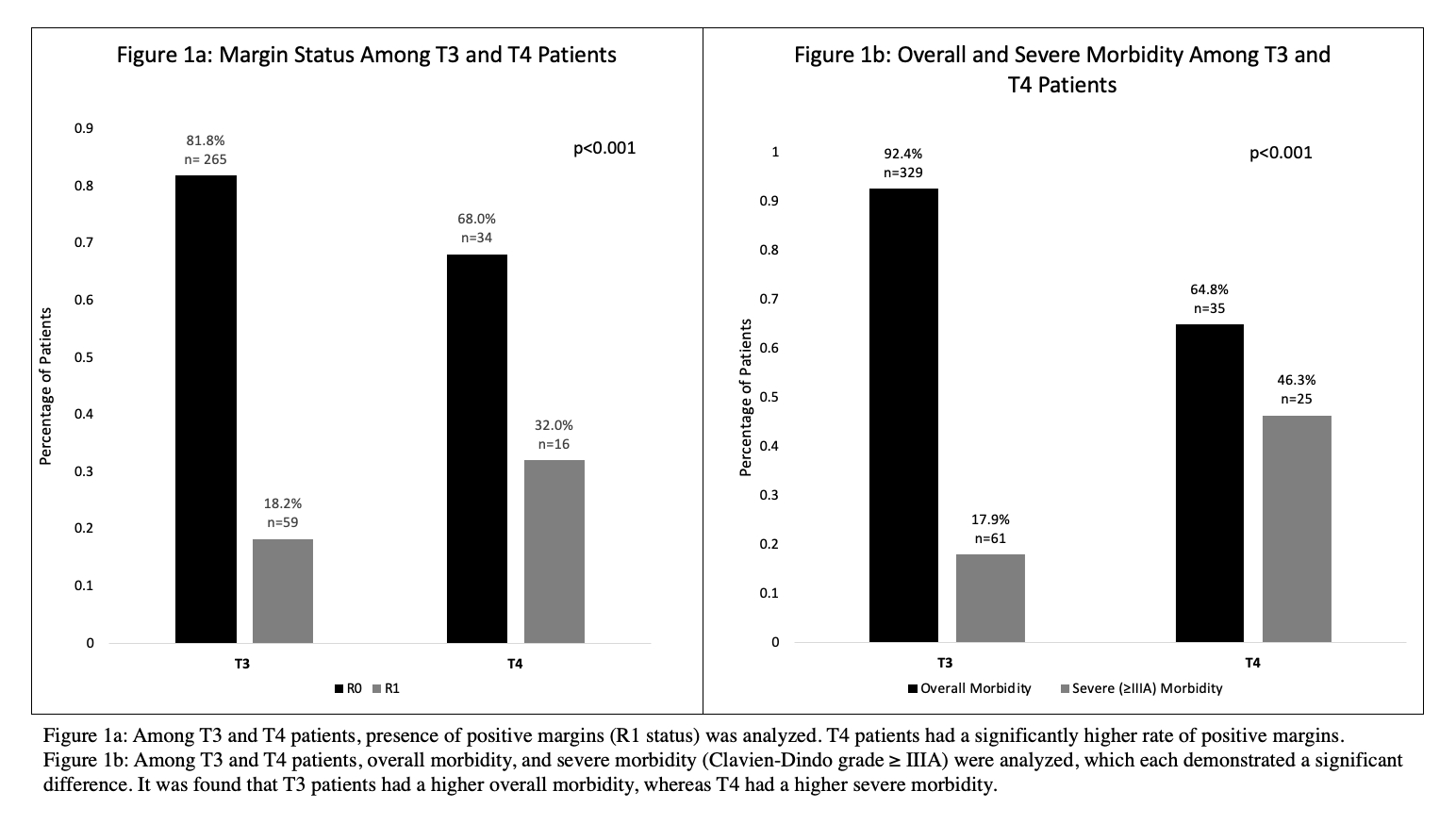
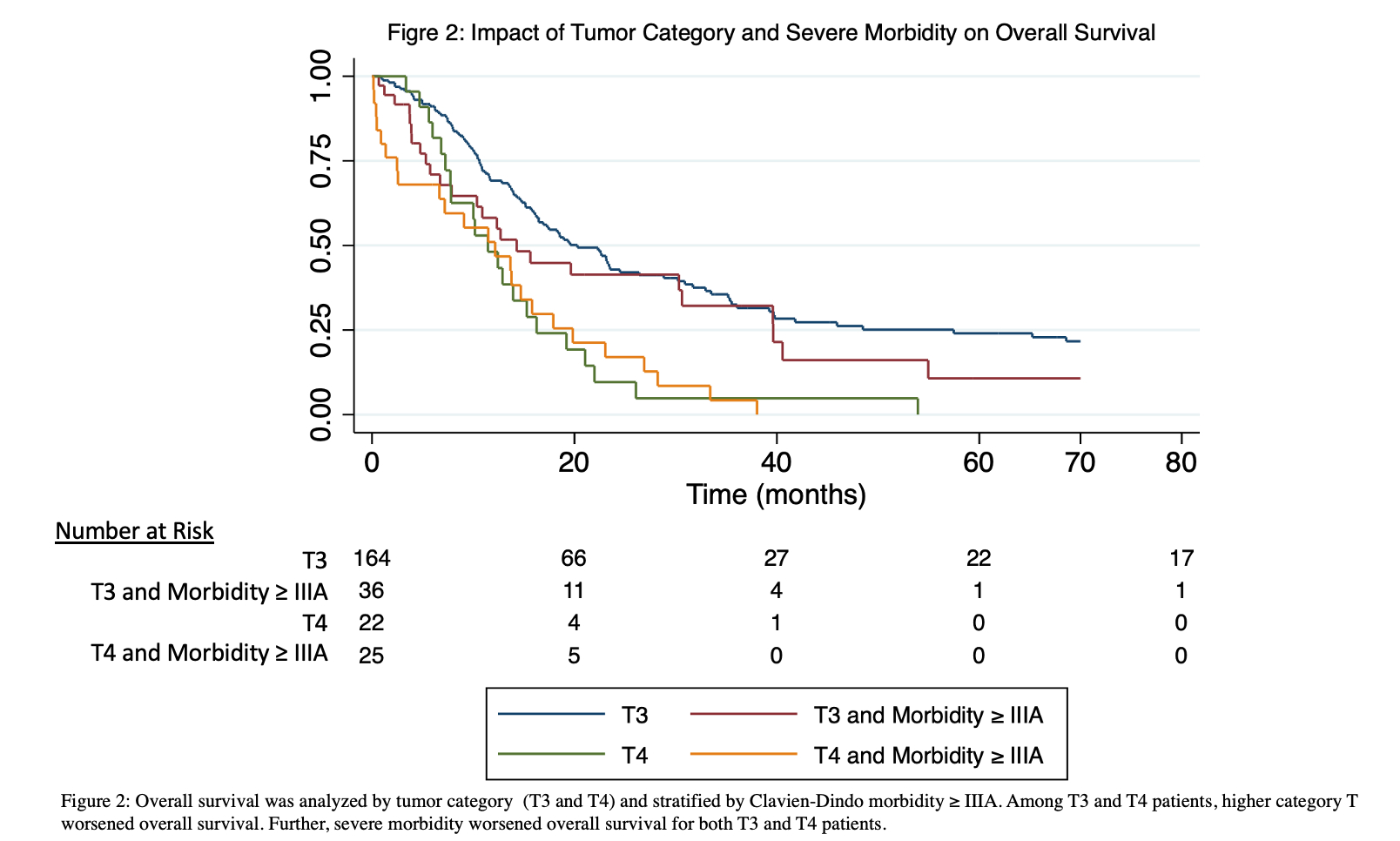
Results: Of 1075 patients, 649 (60.4%) were T1/T2 category, 372 (34.6%) were T3, and 54 (5.0%) were T4. When comparing T categories, there was a significant difference in R1 status (p<0.001): 18.2% among T3 patients and 32.0% among T4 patients (Fig. 1a). T4 patients had the highest rate of recurrence at 78.8% (p<0.001) vs 63.7% for T3 patients. Overall morbidity was highest among T3 patients, however, T4 patients experienced more severe (grade≥ IIIa) morbidity (p<0.001) (Fig. 1b). Furthermore, T4 patients had the longest length of hospital stay (LOS), p<0.001, of 24 days (SD 33.5) vs 7 days (SD 11.9) among T3 patients. For T3 patients, univariable analysis demonstrated that R1 status, overall morbidity, and LOS worsened overall survival (OS) (p<0.02) (Figure 2). Preoperative chemotherapy (p=0.02), and post-operative chemotherapy (p=0.02) and radiotherapy (p=0.05) improved OS. For both T3 and T4 patients, common bile duct, hepatic artery (HA) and/or portal vein (PV) resection provided no significant improvement in OS (p≥0.2). In the multivariable analysis, two variables negatively impacted OS for T3 patients: number of days in the hospital (HR=1.02, 95% CI [1.01-1.03), p<0.001) and R1 status (HR=1.81, 95% CI [1.34-2.45], p<0.001).
Conclusions: This study revealed critical insights into the treatment landscape for GBC. Notably, R1 status significantly differed between T3 and T4 patients, emphasizing challenges posed by advanced disease. It was found that extended surgical interventions have limited impact on survival. Such findings suggest that T3 and T4 patients receive extended surgeries that may not provide benefit and may worsen outcomes due to increased morbidity. While there appears to be advantages of utilizing chemotherapy and adjuvant radiotherapy among T3 patients when analyzed in isolation, multivariable analysis demonstrated no benefit. The multivariable analysis highlighted the negative impact of surgical complications, such as LOS, and R1 status on T3 patients' OS. These findings underscore the delicate balance required in surgical treatments for T3 and T4 GBC, advocating for a nuanced approach tailored to individual patient characteristics to optimize outcomes while minimizing morbidity.
Back to 2024 Abstracts