Back to 2024 Abstracts
PROGNOSTIC FACTORS FOR SURGICAL RESECTION OF MULTIFOCAL INTRAHEPATIC CHOLANGIOCARCINOMA IN THE CHEMOTHERAPY ERA
Anish J. Jain
*, Harufumi Maki, Antony Haddad, Elena Panettieri, Ching-Wei D. Tzeng, Yun Shin Chun, Madhulika Eluri, Shubham Pant, Sunyoung S. Lee, Z. Ian Hu, Kanwal Raghav, Milind Javle, Jean-Nicolas Vauthey, Hop S. Tran Cao, Timothy E. Newhook
Surgical Oncology, The University of Texas MD Anderson Cancer Center, Houston, TX
Background:Prognosis after hepatectomy for multifocal intrahepatic cholangiocarcinoma (iCCA) is worse than for unifocal iCCA with reported post-operative survival of under 2 years. As a result, multifocality must be carefully considered prior to resection. We sought to characterize factors associated with oncologic outcomes following resection for patients with multifocal iCCA compared to unifocal iCCA.
Methods: Prospectively maintained database were queried for patients who underwent curative-intent hepatectomy for iCCa from 1/2003 to 12/2022. Clinicopathological factors and survival were compared in patients with unifocal and multifocal ICCA.
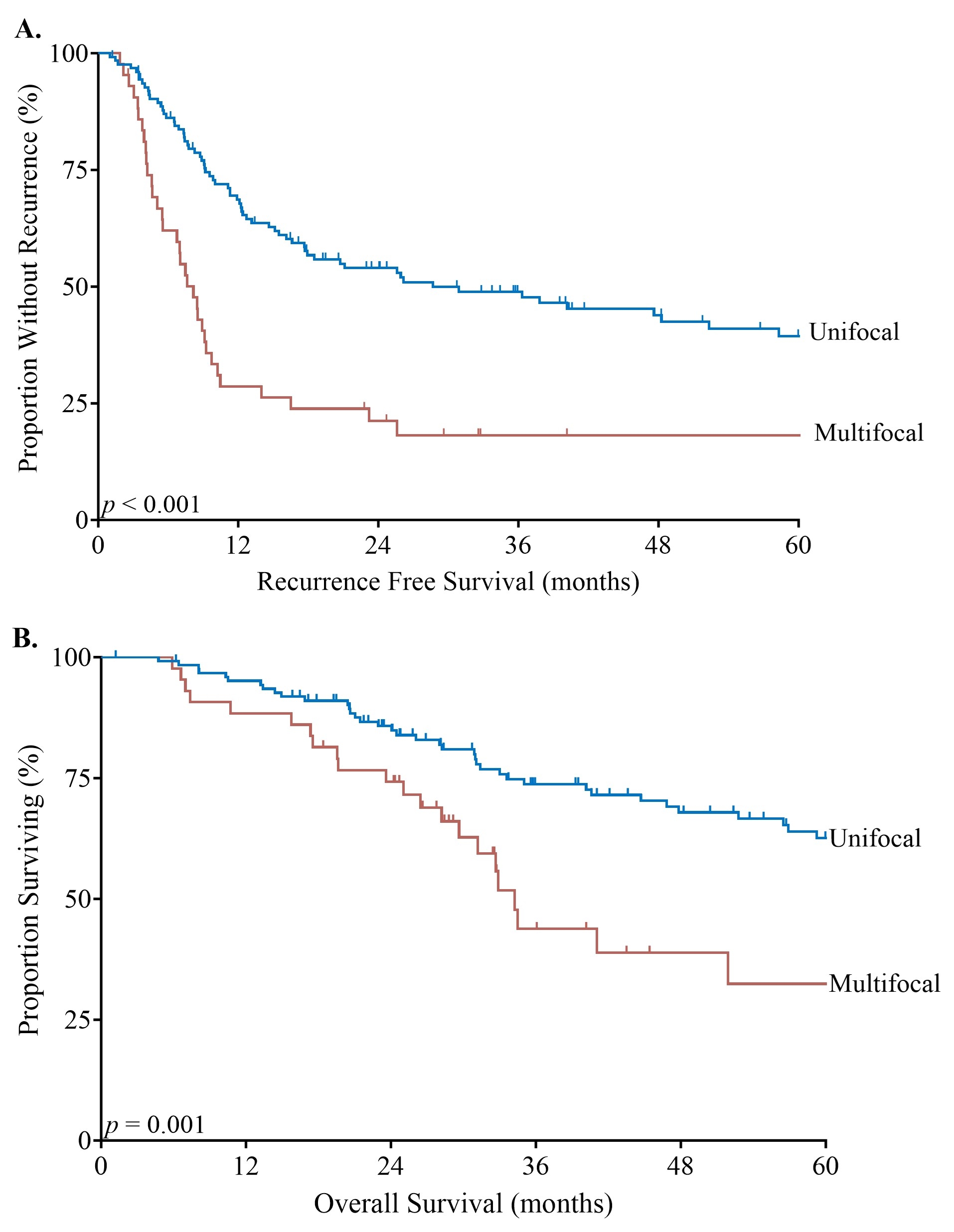
Results:Among 168 patients, 43 (26%) patients had multifocal iCCA and 125 (74%) unifocal iCCA. Patients with multifocal iCCA more frequently received preoperative (70% vs 41%, p=0.049) and postoperative chemotherapy (81% vs. 59%, p=0.009). Patients in both cohorts underwent major hepatectomy, vascular resection, extrahepatic bile duct resection, and lymphadenectomy at similar rates. Lymph node metastasis (N1) was more frequent in patients with multifocal iCCA (40% vs. 14%, p<0.001). Additionally, patients with multifocal iCCA had larger tumors (median 6.5 vs. 5.3 cm; p=0.034) and the median number of tumors for patients with multifocal iCCA was 2 (range: 2-12). Recurrence free survival (RFS) was significantly worse for multifocal compared unifocal (median 8.1 vs. 28.7 months; p<0.001) (Figure 1A). Overall survival (OS) was also significantly worse in the multifocal cohort (median 34.2 vs. 88.4 months; p=0.001) (Figure 1B). On multivariable analysis, tumor size >5 cm (HR: 1.8), N1 (HR: 2.09), and multifocality (HR: 1.97, all p<0.007) were independently associated with RFS, and multifocality (HR: 1.8, p=0.04) was the only independent factor associated with OS for all patients. Among patients with multifocal ICCA, the only factor independently associated with OS was undergoing portal lymphadenectomy (HR: 0.23, p = 0.005). All other factors, including nodal positivity, lymphovascular invasion, margin status, histologic grade, tumor number, bilateral distribution, and tumor size were not associated with OS.
Conclusion:Outcomes following resection of multifocal iCCA are significantly worse than unifocal iCCA despite higher rates of perioperative therapy. However, a select subset derive long-term survival benefits. Further development of objective biomarkers may lead to improved patient selection and oncologic outcomes for patients with resectable multifocal iCCA.
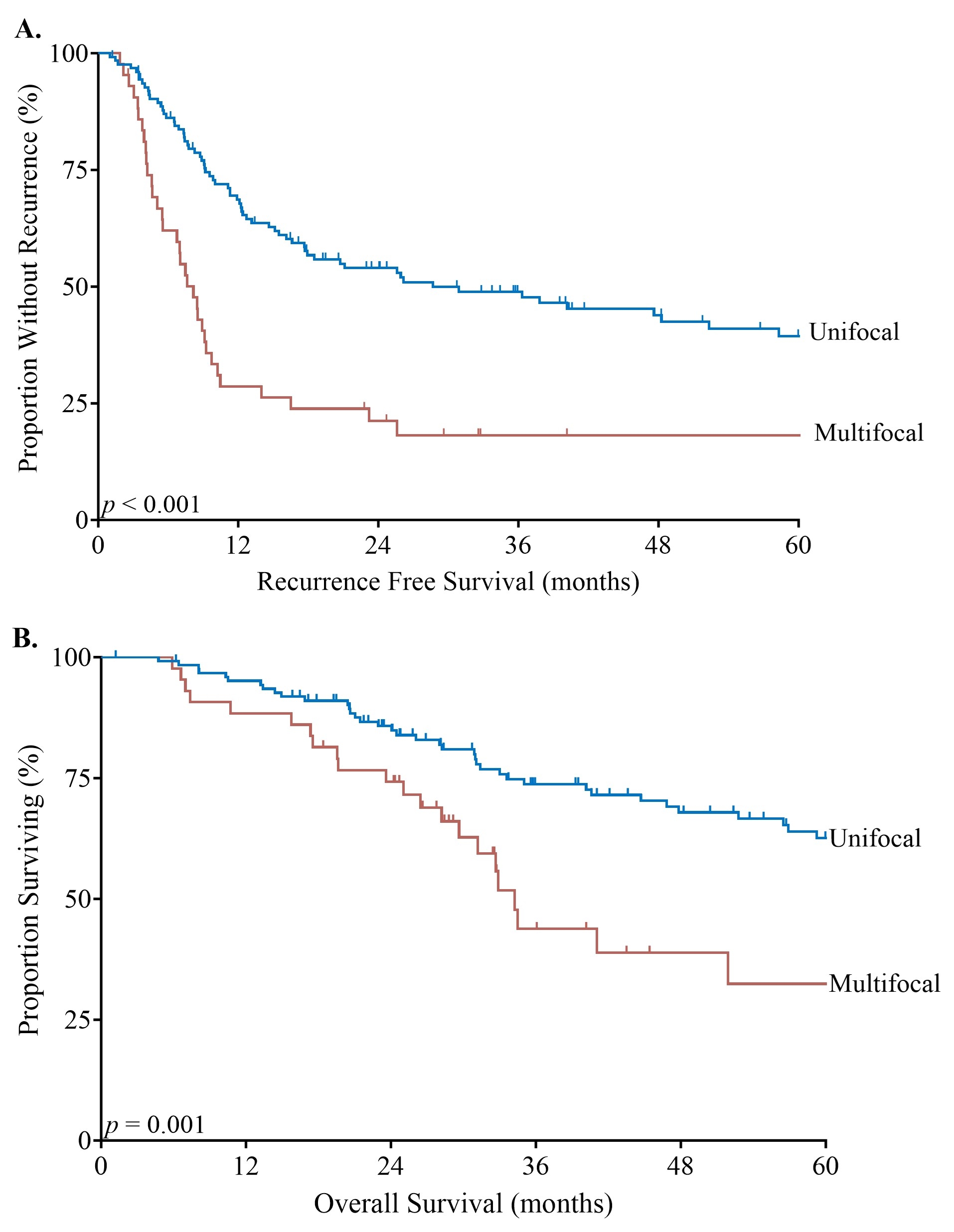
Figure 1. Recurrence Free Survival (1a) and Overall Survival (1b) based on intrahepatic cholangiocarcinoma focality.
Back to 2024 Abstracts