Back to 2024 Abstracts
LONG-TERM OUTCOMES ACCORDING TO SURGICAL MARGIN IN MASS-FORMING CHOLANGIOCARCINOMA: THE ROLE OF R1VASC RESECTION
Flavio Milana
*1,2, Fabio Procopio
1,2, Eleonora Calafiore
1,2, Simone Famularo
1,2, Guido Costa
1,2, Jacopo Galvanin
1, Bruno Branciforte
1, Guido Torzilli
1,21Division of Hepatobiliary and General Surgery, Department of Surgery, IRCCS Humanitas Research Hospital, Rozzano, Milan, Italy; 2Department of Biomedical Sciences, Humanitas University, Rozzano, Milan, Italy
INTRODUCTION:R0-resection is the standard for mass-forming cholangiocarcinoma (MFCCC). R1 (margin<1mm) showed bad outcomes, as R2. R1vasc-resection (detaching tumor from vessels) yielded results comparable to R0 and superior to tumor exposure along the transection plane (R1par) for hepatocellular carcinoma and colorectal liver metastases. The initial MFCCC experience did not confirm these results. This study aims to clarify R1vasc outcomes for MFCCC, dissecting tumor exposure patterns.
METHODS:MFCCC patients resected between 2008-2022 were reviewed. Tumor detachment was reserved for locally-advanced cases. R0, R1par, R1vasc, and R1vasc+par margin status were assessed. The endpoint was to analyze R1vasc oncological suitability, evaluating hepatic recurrence with in-patient and per-resection area analyses.
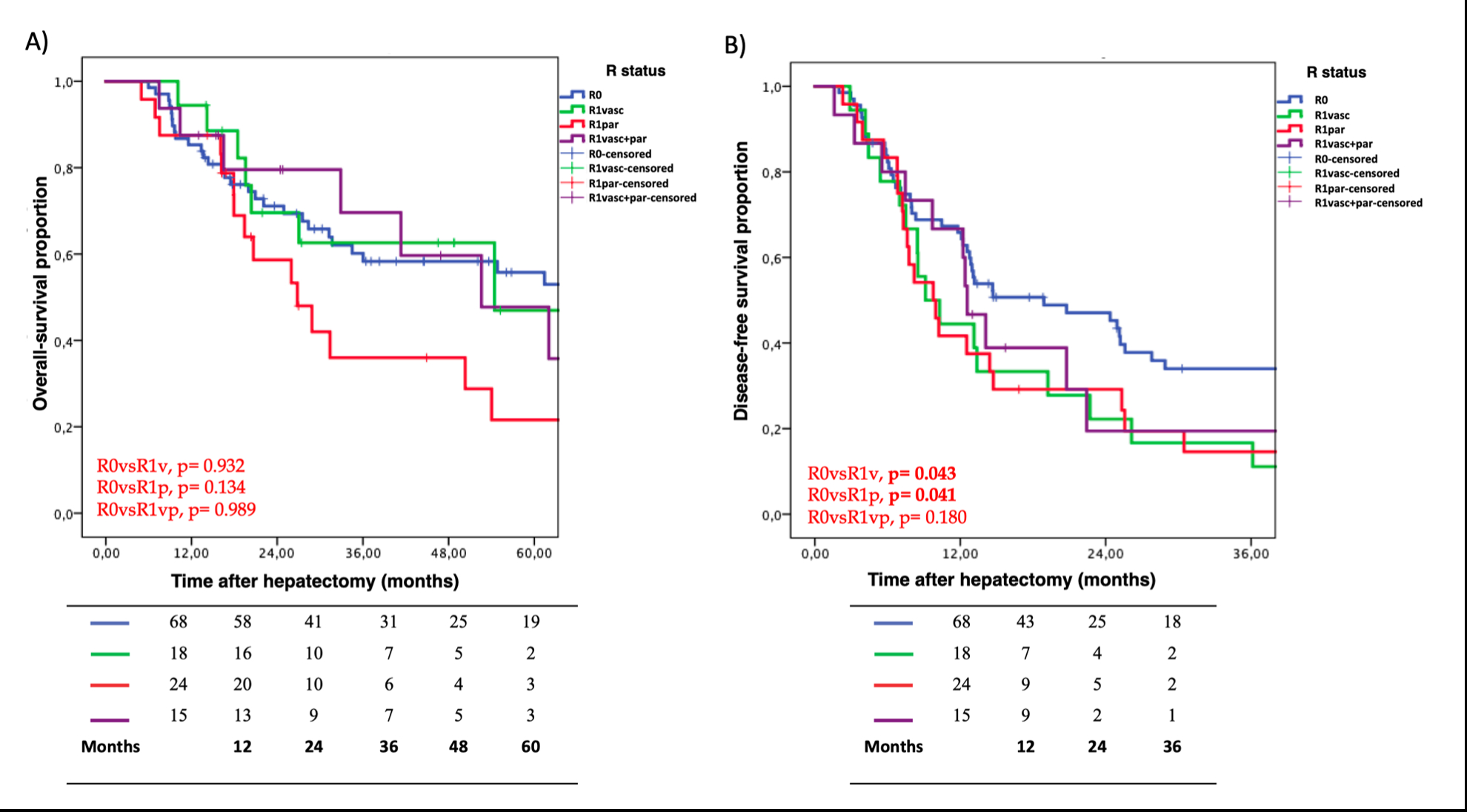
RESULTS:A cohort of 125 patients (161 resection areas), was analyzed with a median follow-up of 56.8months(95%CI:42.7-70.9). Sixty-eight patients (54.4%) achieved R0, 18(14.4%) R1vasc, 24(19.2%) R1par, and 15(12.0%) R1vasc+par. A lower incidence of centrally-located lesions was observed in R0 (48.5%), compared to R1vasc (88.9%,p=0.002), R1par (79.2%,p=0.009), and R1vasc+par (93.8%,p=0.009). Median tumor size was similar between R0 (4.4cm IQR 3.5-6.6) and R1vasc (4.3cm IQR 3.4-6.1,p=0.754), while R1par (8.2cm IQR 4.3-9.9,p=0.005) and R1vasc+par (9.0cm IQR 7.0-11.5,p<0.001) had larger tumors. Similar median overall survival (OS) was reported for R0 (64.8months;95%CI:50.0-79.6) and R1vasc (54.4months;95%CI:19.6-89.2;p=0.932), or R1vasc+par (62.0months, 95%CI:35.6-88.5;p=0.989). Although not significant, R1par showed lower median OS (26.8months;95%CI:16.1-37.6;p=0.134)
(Fig.1A). Higher 1- and 3-year disease-free survival (DFS) was reported for R0 (64.3% and 34.0%) compared to R1vasc (38.9%,11.1%;p=0.043) and R1par (37.5%,9.7%;p=0.041)
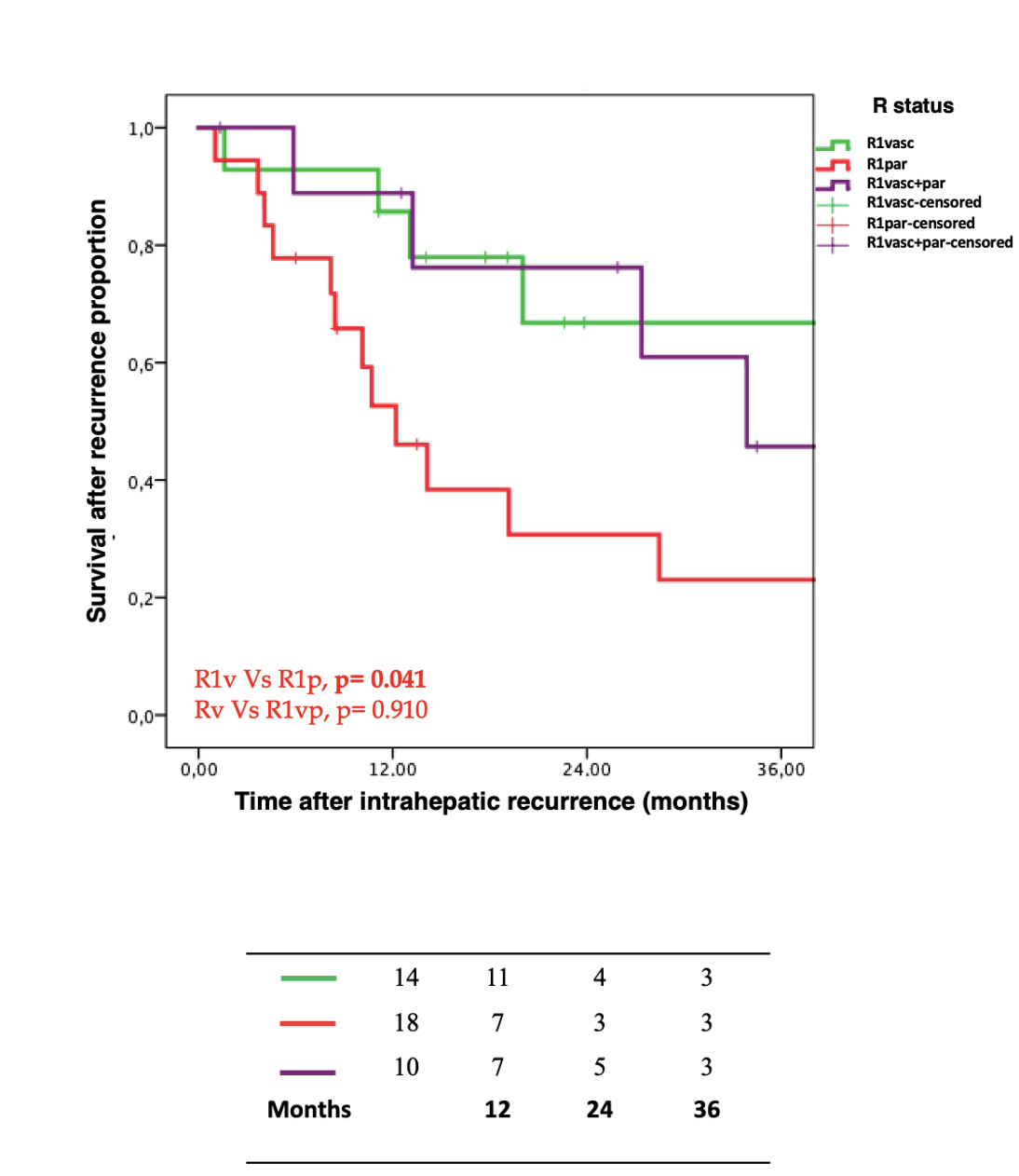
(Fig.1B). In per-patient and per-resection areas analysis, R1par had higher recurrence rates (45.8%,p<0.0001 and 46.1%,p<0.00001), compared to R0 (10.3% and 6.9%), while R1vasc showed comparable rates (16.6%,p=0.453 and 15.8%,p=0.199) as R1vasc+par (20.0%,p=0.296 and 20.0%,p=0.092). At 1- and 3-year, survival after hepatic recurrence was higher for R1vasc (85.7% and 66.8%) compared to R1par (46.1% and 23.0%,p=0.041) and R1vasc+par (76.2%, 45.7%,p=0.910), despite no differences in extrahepatic recurrences among them
(Fig.2). Compared to R0 (13.2%), R1vasc+par (46.7%;p=0.003) and R1par (54.2%;p=0.001) but not R1vasc (27.8%,p=0.137) showed higher rates of extrahepatic recurrence. At multivariate analysis, macrovascular invasion (HR=1.845,95%CI:1.070-3.182;p=0.028) correlated with OS and bilobar disease (HR=2.049,95%CI:1.068-3.933;p=0.031) with DFS.
CONCLUSIONS:R1vasc can be pursued to increase the pool of resectable patients. R1par remains not adequate and R1vasc+par may represent a necessity for larger centrally-located tumors.
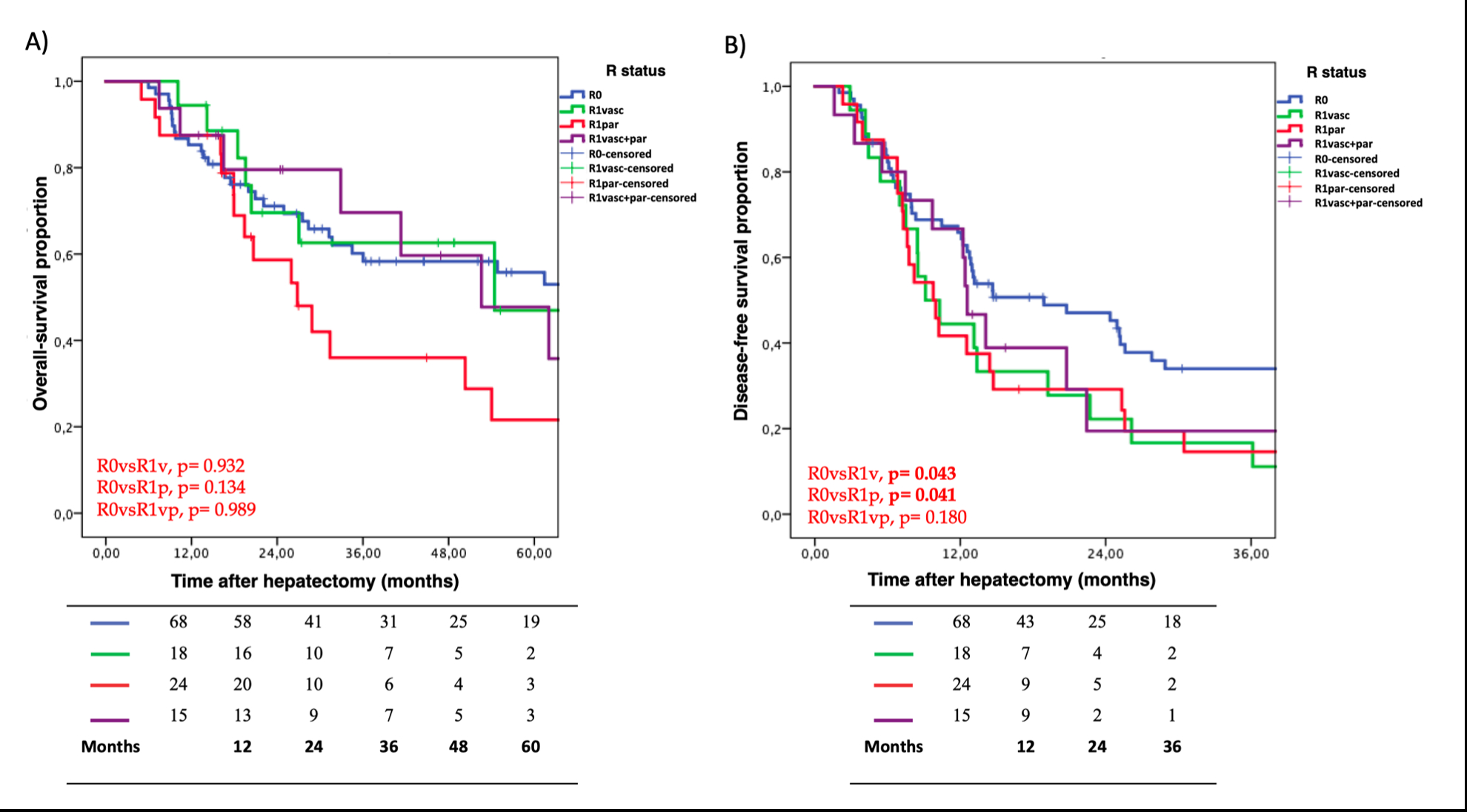
A) Overall survival according to margin status.
B) Disease-free survival according to margin status.
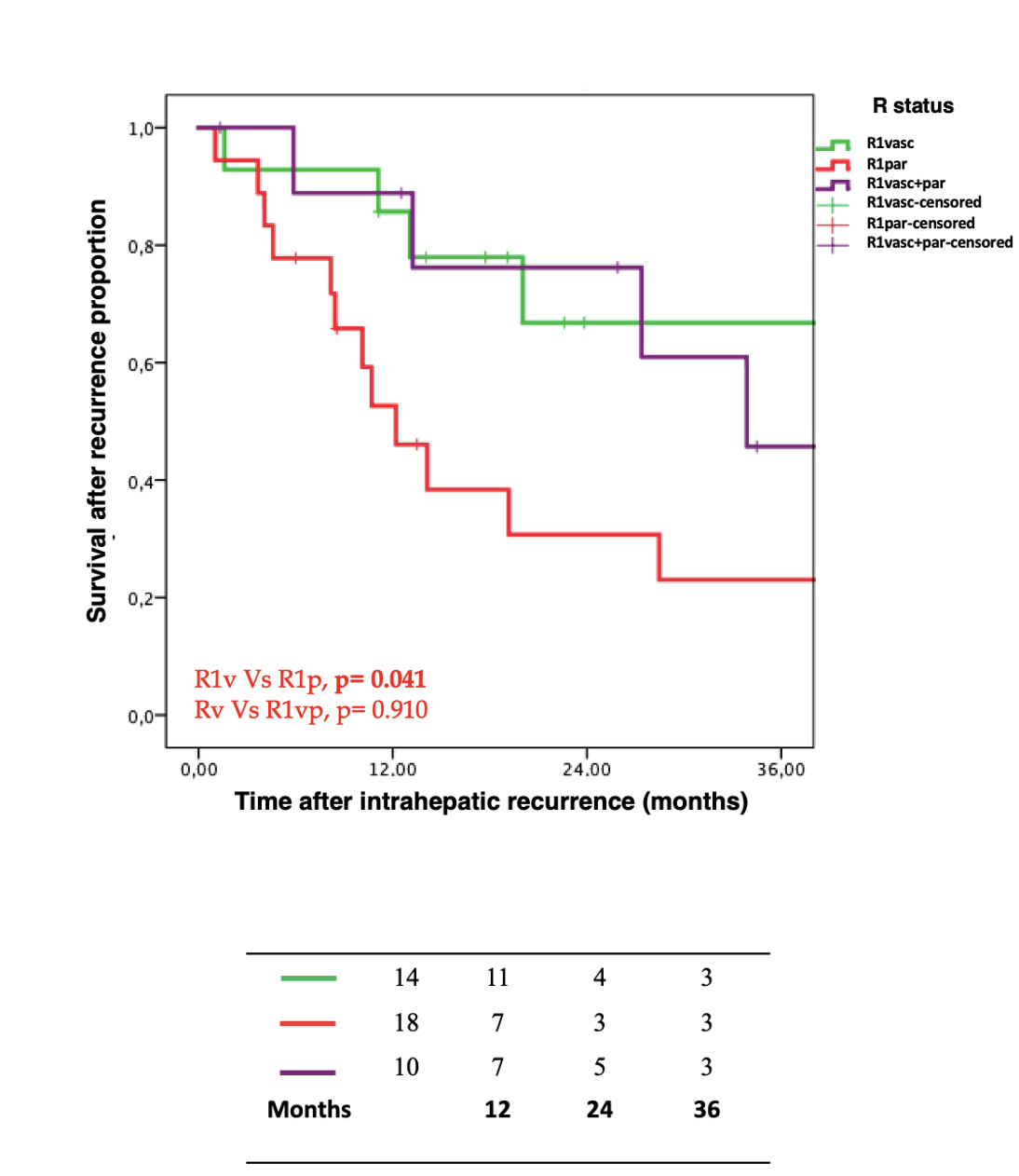
Survival after hepatic recurrence among the R1 patients.
Back to 2024 Abstracts