Back to 2024 Abstracts
PROSPECTIVE EVALUATION OF SURGICAL TECHNIQUES FOR SUBTOTAL CHOLECYSTECTOMY IN PATIENTS WITH ACUTE CHOLECYSTITIS: AN EAST MULTICENTER STUDY
Kazuhide Matsushima
*1, Adam Gutierrez
1, Michael W. Cripps
3, Ryan P. Dumas
2, Caitlin Fitzgerald
2, Erika Bisgaard
2, Henry Jefferson
7, Heather M. Grossman Verner
7, Thomas Schroeppel
3, Janet Lee
3, Tejal Brahmbhatt
8, Jeffrey Melvin
8, Victoria Wagner
4, Sigrid Burruss
5, Liz Penaloza-Villalobos
5, Shedd B. Gregory
5, Nadine Barth
6, Isabella Armento
6, Jeffry Nahmias
9, Erika Tay-Lasso
9, Brandon Shin
1, Emma Longo
1, Morihiro Katsura
1, Zachary Warriner
41Surgery, University of Southern California, Los Angeles, CA; 2The University of Texas Southwestern Medical Center, Dallas, TX; 3University of Colorado Anschutz Medical Campus School of Medicine, Aurora, CO; 4University of Kentucky, Lexington, KY; 5Loma Linda University Medical Center, Loma Linda, CA; 6Cooper University Health Care, Camden, NJ; 7Methodist Dallas Medical Center, Dallas, TX; 8Boston University, Boston, MA; 9University of California Irvine, Irvine, CA
Background: Different techniques have been described for performance of subtotal cholecystectomy, namely fenestrating and reconstituting subtypes. Currently, little remains known about the impact of these different techniques on short-term and long-term patient outcomes. The aim of this study is to compare various clinical outcomes between patients undergoing fenestrated and reconstituting subtotal cholecystectomy for acute cholecystitis.
Methods: This is a multicenter prospective observational study sponsored by the EAST Multicenter Trials Committee. Between July 2019 and June 2022, we included patients (age ≥18 years) who received surgical management of acute cholecystitis defined by the Tokyo Guideline 18 diagnostic criteria. In-hospital and long-term (6-month) outcomes for patients undergoing fenestrating versus reconstituting subtotal cholecystectomy were compared.
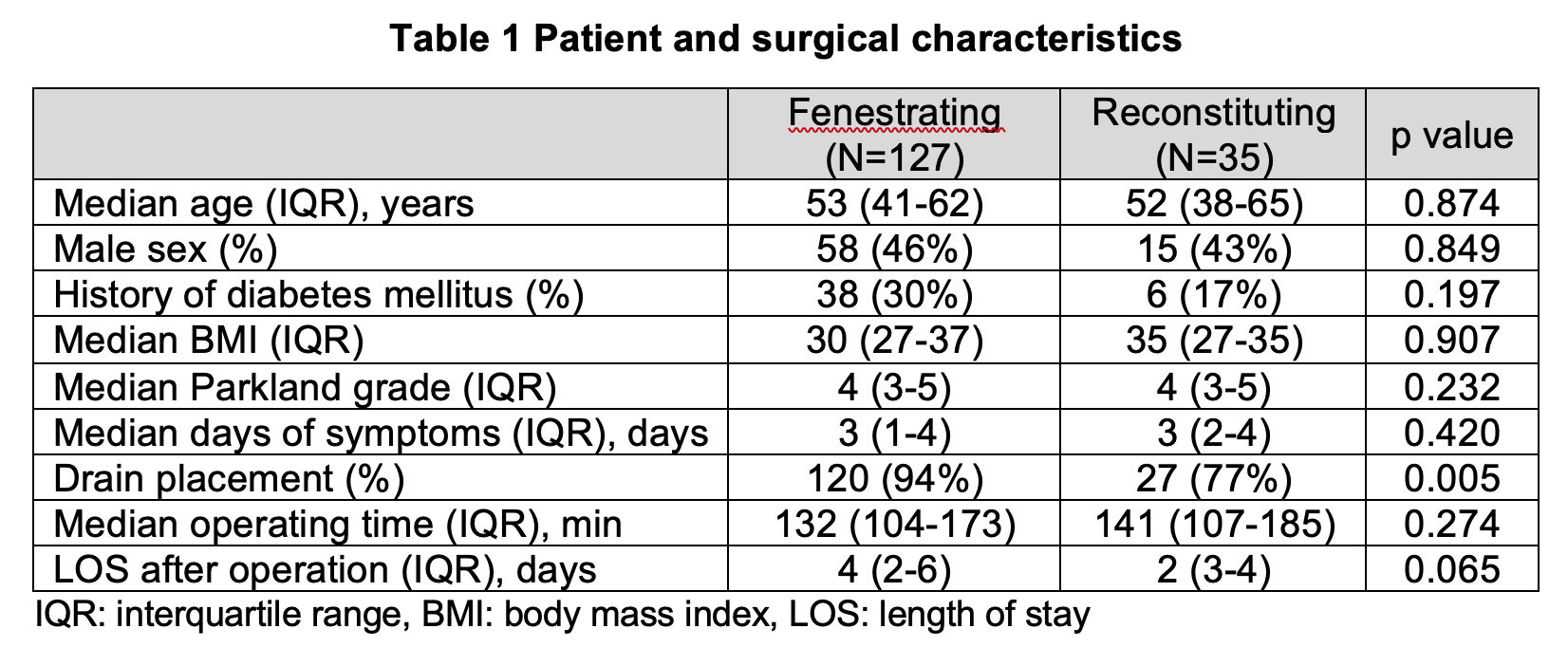
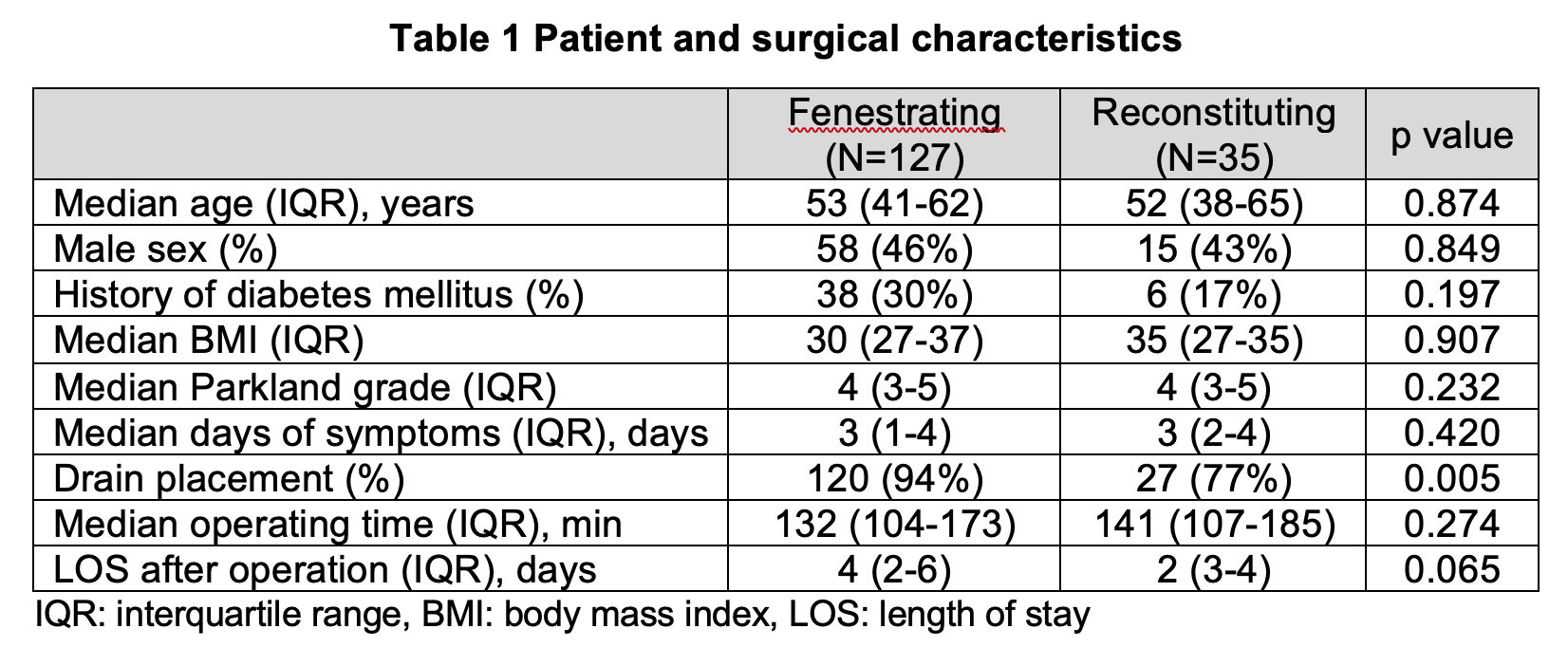
Results: A total of 2,685 patients with acute cholecystitis were enrolled from 9 centers. The median age was 41 years (IQR: 30-53) and 28% were male. Diabetes mellitus was the most common comorbid condition (12%). Of those, 162 patients (6.1%) underwent subtotal cholecystectomy (laparoscopic: 128 (79%), laparoscopic converted to open: 30, open: 4), whereas laparoscopic converted to open total cholecystectomy was performed in 41 patients (1.6%). Approximately 78% of subtotal cholecystectomy used fenestrating technique rather than reconstituting technique (
Table 1). In the early postoperative period, patients in the fenestrating group more commonly developed bile leaks (32% versus 8.6%, p=0.005) and required readmission within 30 days (30/125: 24% versus 2/35: 5.7%, p=0.016). There were not significant differences in the rate of secondary interventions (34% versus 17%, p=0.063). At 6-month follow-up, the incidence of recurrent biliary disease was statistically similar between the fenestrating and reconstituting groups (11% versus 21%, p=0.158). Only 5 patients (4.3%) underwent completion cholecystectomy during the follow-up period.
Conclusions: In this multicenter study, subtotal cholecystectomy was more commonly performed than open conversion total cholecystectomy as a bail-out procedure for acute cholecystitis. Both fenestrating and reconstituting subtypes were associated with recurrent biliary disease and complications requiring secondary intervention and readmission in the early and later postoperative period.
Back to 2024 Abstracts