Back to 2024 Abstracts
EFFECT OF TELEMEDICINE USE ON MEDICAL SPENDING AND HEALTH CARE UTILIZATION AMONG GASTROINTESTINAL CANCER PATIENTS
Yutaka Endo
*, Muhammad Muntazir M. Khan, Selamawit Woldesenbet, Diamantis Tsilimigras, Mujtaba Khalil, Erryk Katayama, Muhammad Muntazir Mehdi Khan, Timothy M. Pawlik
Surgery, The Ohio State Wexner Medical Center, Columbus, OH
Introduction: Telemedicine use increased with the COVID-19 pandemic, yet the effect of telemedicine on resource utilization has not been investigated. We sought to characterize the impact of telemedicine on healthcare utilization and medical spending among patients with gastrointestinal (GI) cancer.
Methods: Patients with a newly diagnosed GI cancer from 2013 to 2020 were identified from the IBM MarketScan database. To mitigate potential demographic variations, 1:1 nearest neighbor propensity score matching (PSM) was applied, which adjusted for variables including cancer-type and different treatment approaches. Disparities among telemedicine users versus non-users relative to healthcare utilization, total medical outpatient costs within one-year post-diagnosis, and out-of-pocket (OOP) expenses were examined. Outpatient visits accounted for the total of in-person and telemedicine visits.
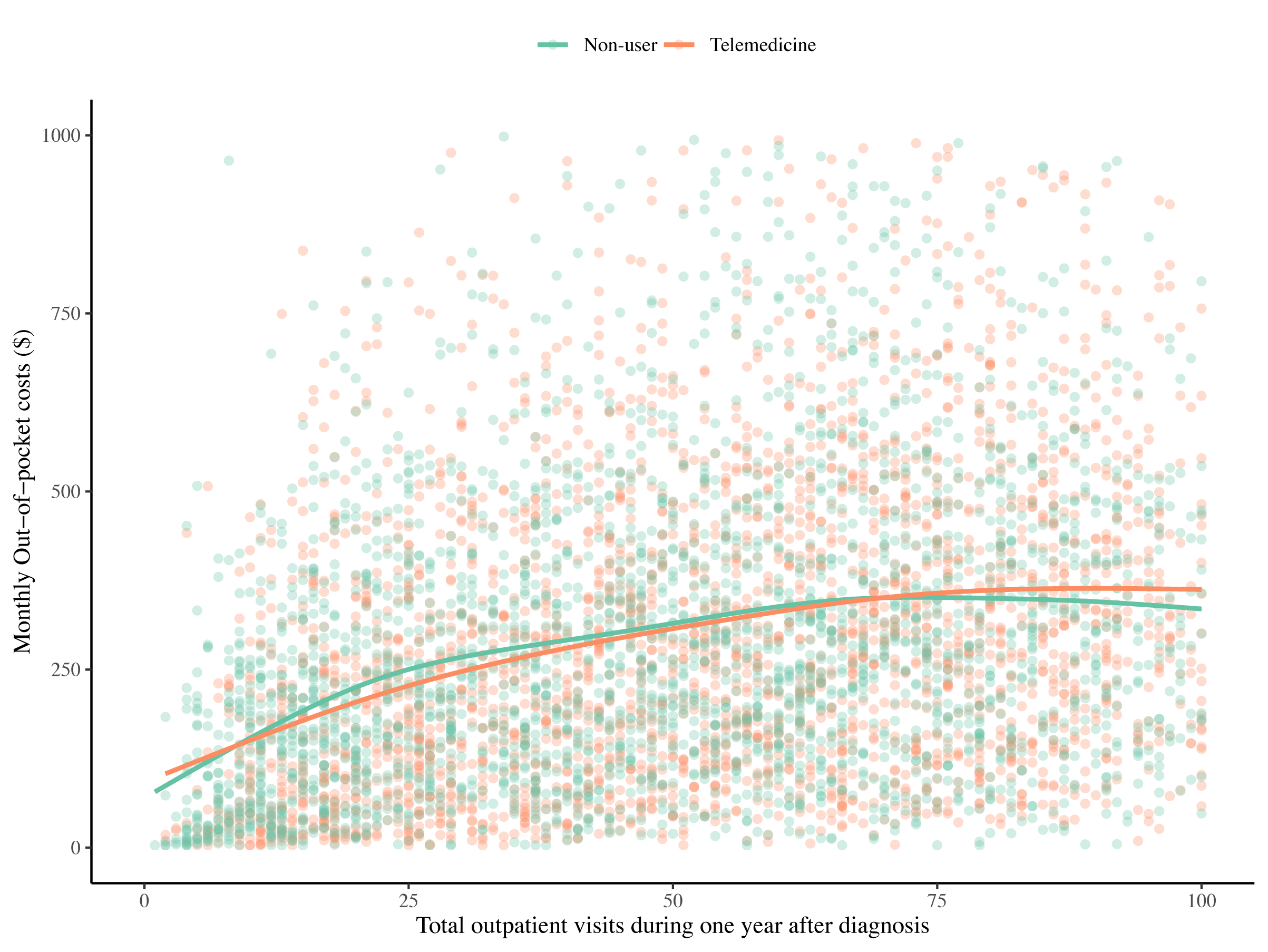
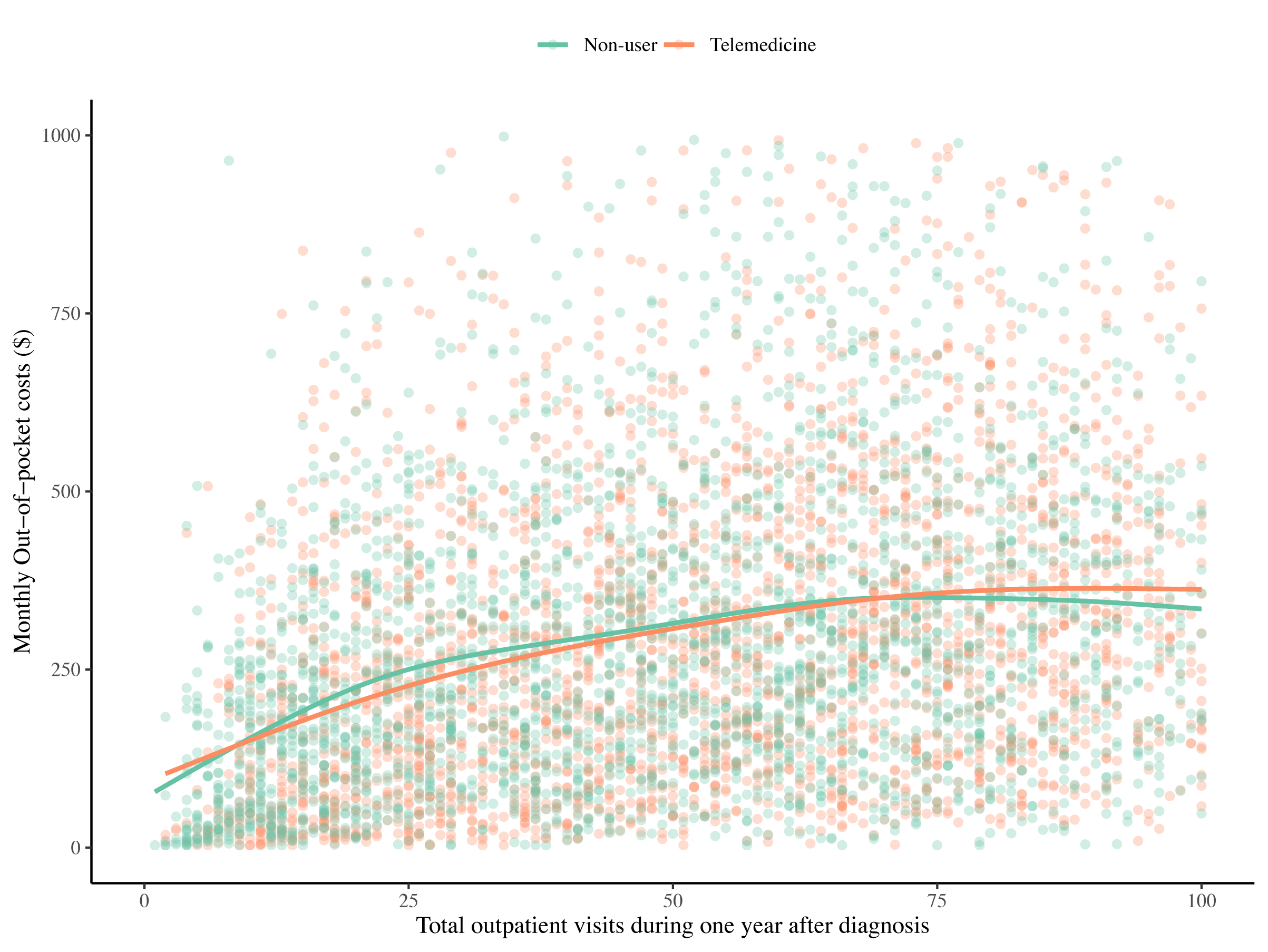
Results: Among 32,948 patients with a GI cancer (esophageal, n=1,878, 5.7%; gastric, n=2,025, 6.1%; liver, n=2,960, 9.0%; bile duct, n=599, 1.8%; pancreas, n=3,105, 9.4%; colorectal, n=22,381, 67.9%), a subset of individuals utilized telemedicine (n=3,068, 9.3%). Telemedicine users tended to be younger (55.0 years, IQR 49.0-60.0 vs. 56.0 years, IQR 50.0-60.0), active full-time workers (74.3% vs. 59.4%), as well as be treated with chemotherapy (80.7% vs. 69.5%) or multimodal treatment (60.0% vs. 51.7%) (all p<0.05). PSM was utilized to match telemedicine users and non-users into two cohorts that were well-balanced with respect to covariates (telemedicine, n=3,068 vs. non-user, n=3,068). Notably, while the number of in-person visits were comparable between the two groups (telemedicine, 54, IQR 30-77 vs. non-user, 53, IQR 29-75, p=0.12), telemedicine users had greater overall healthcare utilization (in-patient and virtual) than non-users (telemedicine, 57, IQR 34-81 vs. non-user, 53, IQR 28-75, p<0.001). Overall, total medical spending per month for telemedicine users was higher than non-users (telemedicine, $10,658, IQR $5,112-$18,530 vs. non-user, $9,790, IQR $4593-$16,190, p<0.001), while monthly OOP costs for telemedicine users were comparable (telemedicine, $273, IQR $137-$449 vs. non-user, $262, IQR $142-$427, p=0.30). OOP costs increased proportionally with the number of outpatient visits, with no observed differences between telemedicine users and non-users (
Figure).
Conclusion: Telemedicine use did not mitigate utilization of in-person clinic visits. In fact, patients who utilized telemedicine were more often high health-care utilizers with increased outpatient visits, as well as higher total medical spending per month. Nonetheless, monthly OOP costs were similar across both groups. Although telemedicine may not decrease overall resource utilization, it may facilitate care for a subset of high-intensity GI cancer patients without adverse financial implications.
Back to 2024 Abstracts