Back to 2024 Abstracts
IMPACT OF POUCH LEAKS ON QUALITY OF LIFE AND SYMPTOMS IN PATIENTS AFTER ILEAL POUCH-ANAL ANASTOMOSIS SURGERY
Ali Alipouriani
*, Lukas Schabl, Tracy L. Hull, Jeremy M. Lipman, Emre Gorgun, David Liska, Michael Valente, Scott Steele, Stefan D. Holubar
Colorectal Surgery, Cleveland Clinic, Cleveland, OH
Introduction: Ileal pouch-anal anastomosis (IPAA) is the procedure of choice in patients requiring total proctocolectomy. The reported leak rates after IPAA surgery range from 1-12% with well described significant impact on postoperative morbidity and recovery. However, the long-term impact of salvaged pouch leaks on the broader quality of life outcome and pouch function remains poorly understood. This study aimed to compare the bowel movement frequency and quality of life between patients with and without postoperative leaks after IPAA surgery. We hypothesized that patients who had salvaged pouch leaks would have worse long-term quality of life and pouch function compared to matched patients without postoperative leaks.
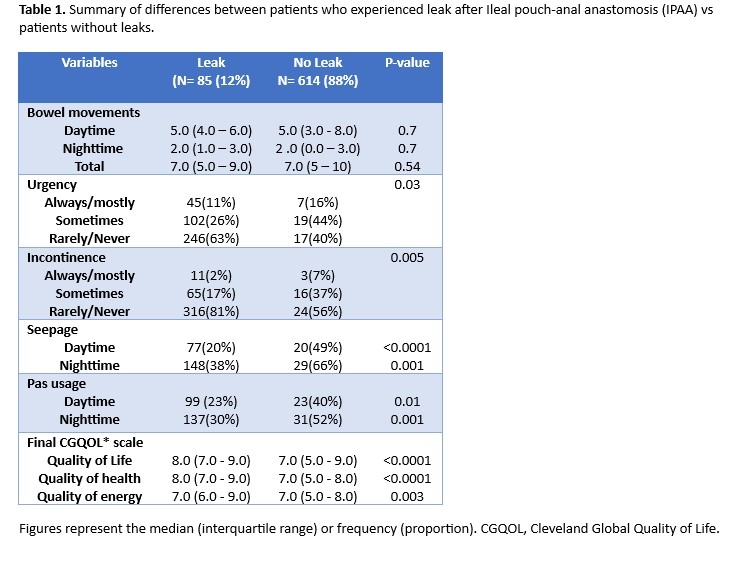
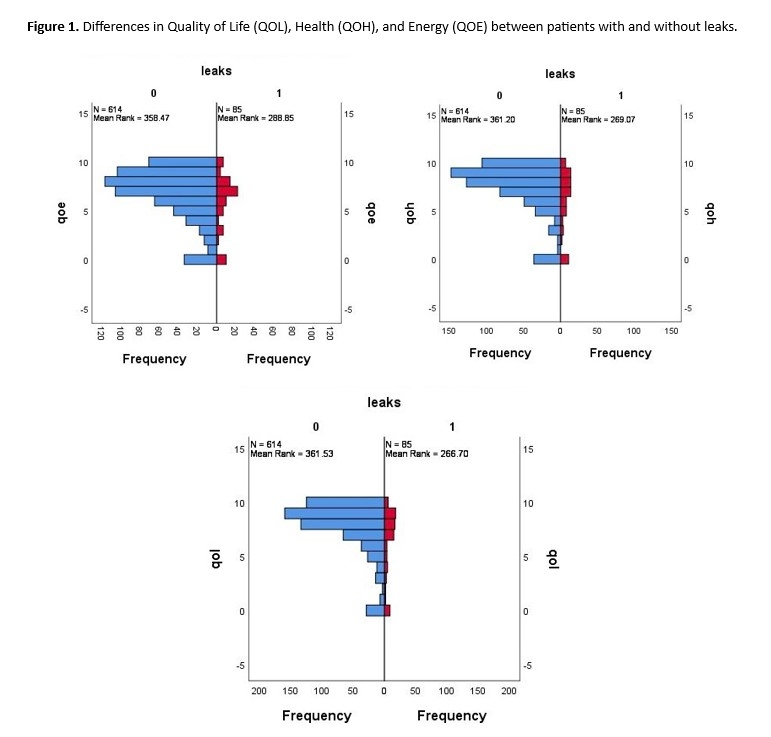
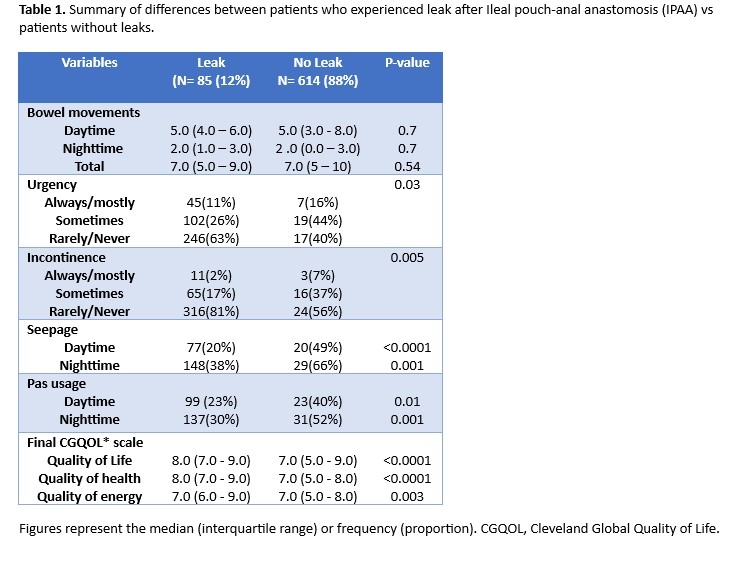
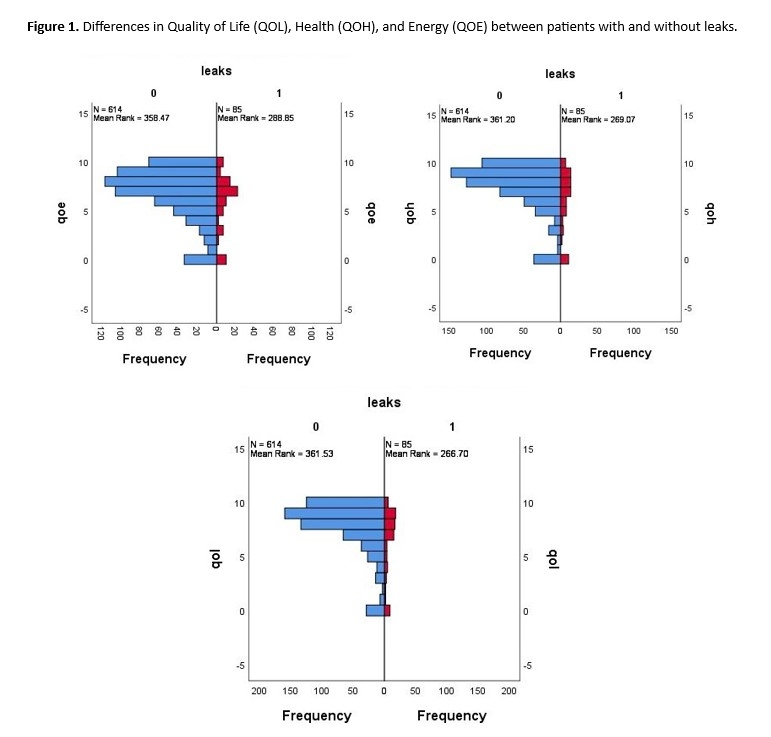
Methods: This retrospective cohort study included patients who underwent IPAA (n=4058) between 1995-2022. Leak was defined as abscess or fistula requiring intervention, who had definitive resolution of their pouch leaks, whether with conservative treatment or after salvage surgery or pouch excision with end ileostomy creation. The Leak group consisted of 194 patients with treated leaks. The No Leak group included 963 patients without leaks, matched 1:5 on sex, age (± 3 years), and surgery date. Questionnaire data were available for 85 of 194 patients with leaks and 614 of 963 without leaks. Quality of life (QoL) was assessed using SF-36, health status using EORTC QLQ-C30 (QoH), and life enjoyment (QoE) using a standardized scale. Bowel movements, seepage, and pad usage were recorded. Outcomes were compared using Mann-Whitney U, t-tests, and chi-square tests.
Results: A total of 699 patients with IPAA were included, with 85 (12%) in the leak group. The median age was 42 (IQR, 31-53) years, and 54% were male. Median time from surgery to the last QoL assessment was 6.58(IQR: 3.5-11.3) years in the Leak group and 6.05 (IQR: 2.5-11.2) days in the No Leak group. Patients with Leaks reported significantly lower QoL (median 7(IQR: 5-9) vs 8 (IQR :7-9); p<0.001), lower health status on the QoH scale (median 7(IQR: 5-8) vs 8 (IQR :7-9);p<0.001), and lower life enjoyment on the QoE scale (median 7(IQR: 5-8) vs 7(IQR :6-9);p=0.003) compared to the No Leak group. A higher proportion of patients in the Leak group reported daytime (49% vs. 20%,p<0.001) and nocturnal seepage (66% vs. 38%,p=0.001), along with greater daytime (40% vs. 22%,p=0.01) and nighttime pad usage (53% vs. 30%,p=0.001). There were no significant differences in the number of bowel movements per 24 h (p=0.54), daytime bowel movements (p=0.7), or nighttime bowel movements (p=0.695) between the groups.
Conclusions: In matched cohorts, salvaged pouch leaks were associated with reduced quality of life, health status, and life enjoyment compared with matched patients without leaks. Patients with leaks also had increased rates of seepage and pad usage, indicating worse pouch function.
Back to 2024 Abstracts