Back to 2024 Abstracts
SURVIVAL OUTCOMES AFTER ADJUVANT TREATMENT IN UPSTAGED CT2N0 RECTAL CANCER: ARE WE UNDERUTILIZING THERAPY?
Simran Kripalani
*1, Caroline Westwood
1, Jill S. Hasler
1,2, Andrea Porpiglia
1,2, Stephanie H. Greco
1,2, Sanjay S. Reddy
2,1, Joshua Meyer
1,2, Jeffrey M. Farma
1,2, Anthony Villano
1,21Temple University, Philadelphia, PA; 2Fox Chase Cancer Center, Philadelphia, PA
Introduction: Per the NCCN guidelines, in general, a patient with clinically staged cT2N0 rectal cancer is recommended to undergo resection upfront. A challenge encountered in clinical practice is cT2N0 disease subsequently upstaged to pT3N0 as there are no clear management guidelines for adjuvant treatment. We aimed to analyze national trends in adjuvant management strategies and identify morbidity or survival differences associated with this clinical scenario.
Methods: The National Cancer Database (2004-2020) was queried for patients
> 18 years of age with a diagnosis of cT2N0 rectal adenocarcinoma who underwent surgical resection and were upstaged to pT3N0. Kruskal-Wallis and Chi-square tests were used to compare characteristics of treatment cohorts. Cox Proportional Hazard Models with treatment group treated as a time-varying covariate and six-month landmark Kaplan Meier (KM) curves were utilized to compare outcomes and five-year overall survival (OS) respectfully. Treatment groups included: (1) surgery alone, (2) surgery + postoperative (post-op) chemotherapy alone, (3) surgery + post-op chemoradiation, and (4) surgery + chemotherapy + radiation.
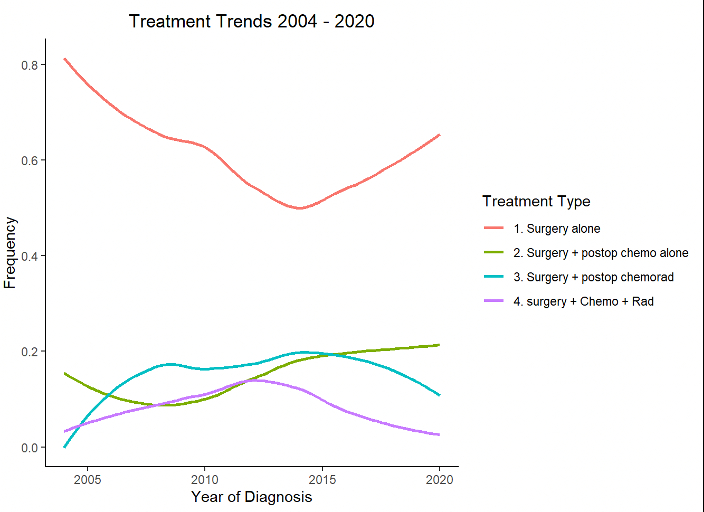
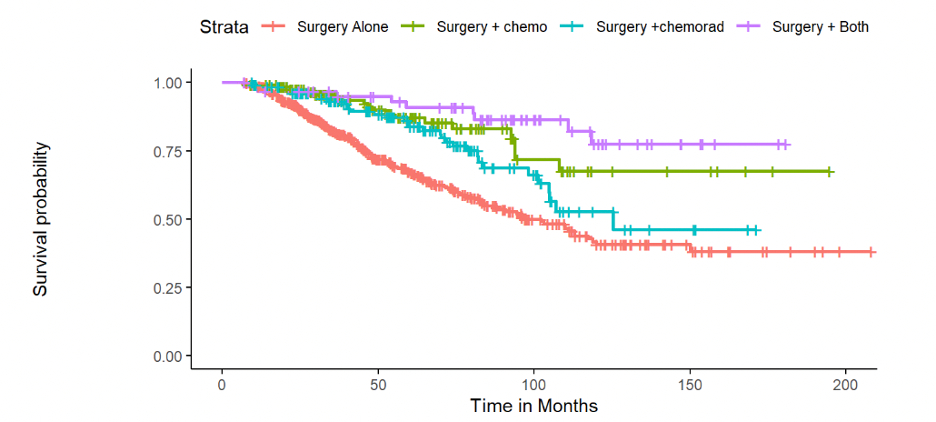
Results: The analytic cohort included 878 patients who received the following treatment strategies: surgery alone (58.9%, n=518), surgery + post-op chemotherapy (16.6%, n=146), surgery + post-op chemoradiation (16.2%, n=142), and surgery + chemotherapy + radiation (8.2%, n=72). The surgery alone cohort exhibited a higher mean age (68 years) and highest frequency of Medicare insurance (56.9%) (p<0.001). Preoperative comorbidity index, tumor size, mean preoperative CEA level, and MSI-status were comparable amongst all treatment groups (p>0.05). Patients who received post-op chemotherapy or chemotherapy + radiation had higher rates of poorly differentiated/undifferentiated tumors (16.4% and 15.3% respectively) than surgery alone (8.9%) and surgery+ postoperative chemoradiation (11.3%) (p=0.006). Over the study period, surgery alone decreased from 86.7% to 65.1%, with concomitant increases in post-op adjuvant therapy (Figure 1). After controlling for covariates, post-op chemotherapy (HR=0.41, 95 CI 0.25-0.67) and chemotherapy + radiation (HR=0.42, 95%CI 0.22-0.82) remained independently associated with improved OS compared to surgery alone, whereas chemoradiation did not (HR=0.87, 95%CI 0.61-1.23). KM Curves showed that five-year survival was lowest in the surgery alone group at 62.4%, whereas all other groups ranged anywhere from 77% to 83.8% (Figure 2).
Conclusions: In this analysis, post-op adjuvant regimens including chemotherapy were independently associated with improved survival in cT2N0 rectal cancer upstaged to pT3N0. Adjuvant therapy may currently be underutilized in this setting. Additional research to understand the strategies and settings in which optimal benefit is derived is necessary.
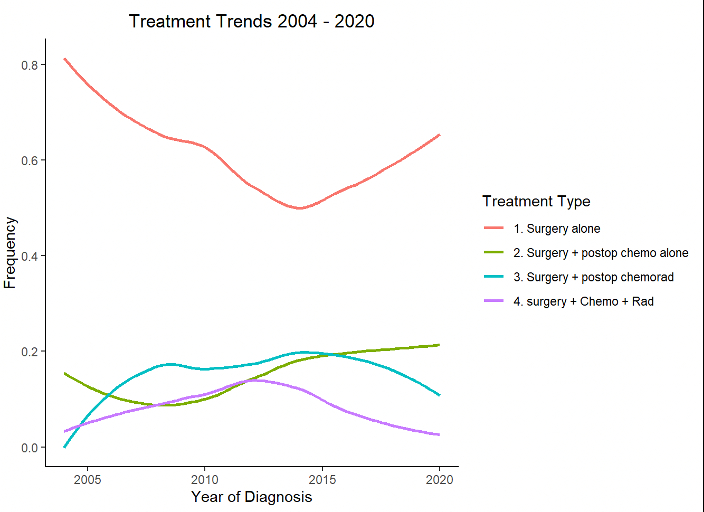
Figure 1: Treatment Trends for cT2N0 Gastric Cancer upstaged to pT3N0 after Resection
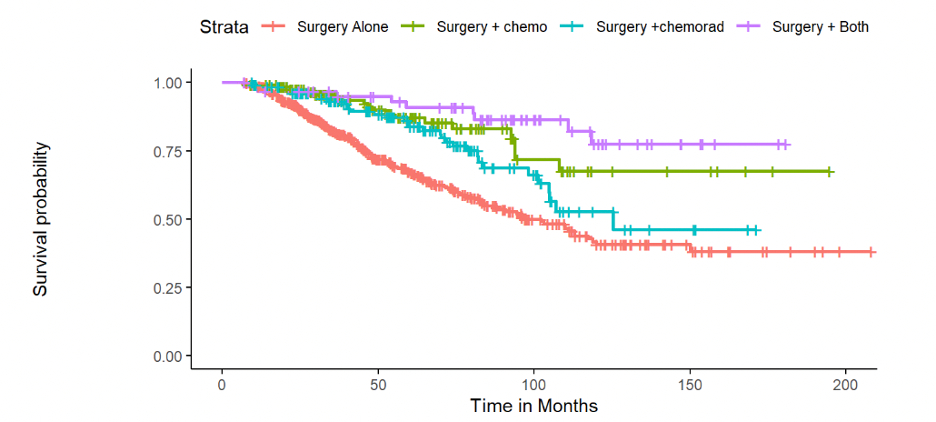
Figure 2: 6-Month Landmark Kaplan Meier Overall Survival
Back to 2024 Abstracts