Back to 2024 Abstracts
THE EFFECTS OF SMALL EXTRACELLULAR VESICLES DERIVED FROM ADIPOSE MESENCHYMAL STEM CELLS ON COLON ANASTOMOSIS HEALING
Zhiwei DONG
*, Siran Zhou, Philip Wai Yan W. Chiu
The Chinese University of Hong Kong Faculty of Medicine, Hong Kong, Hong Kong
Background:
Colorectal cancer (CRC) is one of the most common cancers, and surgery, particularly colectomy, remains a primary treatment approach. However, postoperative complications are associated with increased morbidity and mortality. Mesenchymal stem cells (MSCs) have emerged as promising candidates due to their regenerative potentials. Studies have shown that the beneficial effects of MSCs are largely mediated by their paracrine activity, particularly the small extracellular vesicles (sEVs). These sEVs offer several advantages, such as long-term stability and minimal immune rejection. This project aims to investigate the effects of adipose MSCs-derived sEVs on colon anastomosis healing.
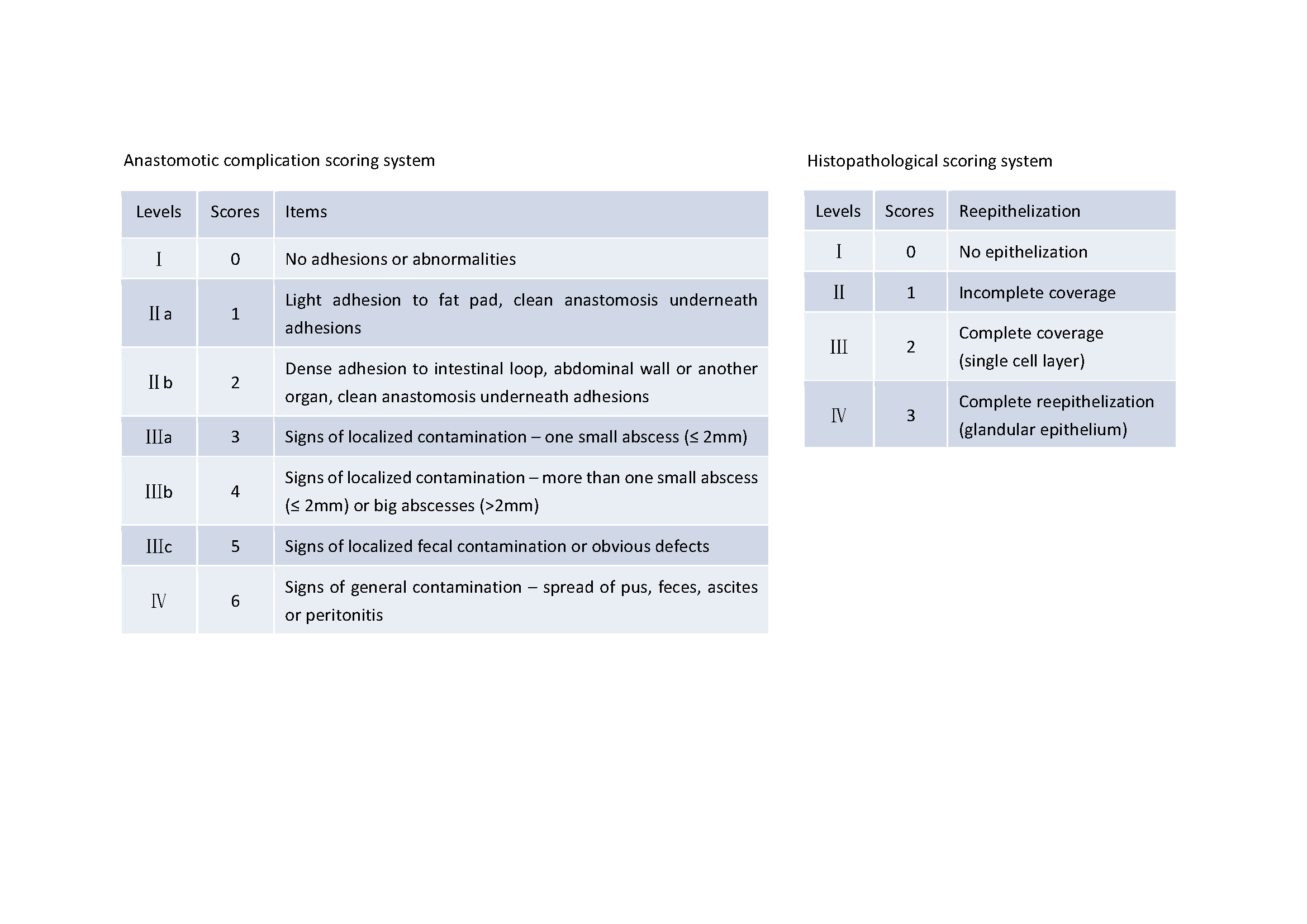
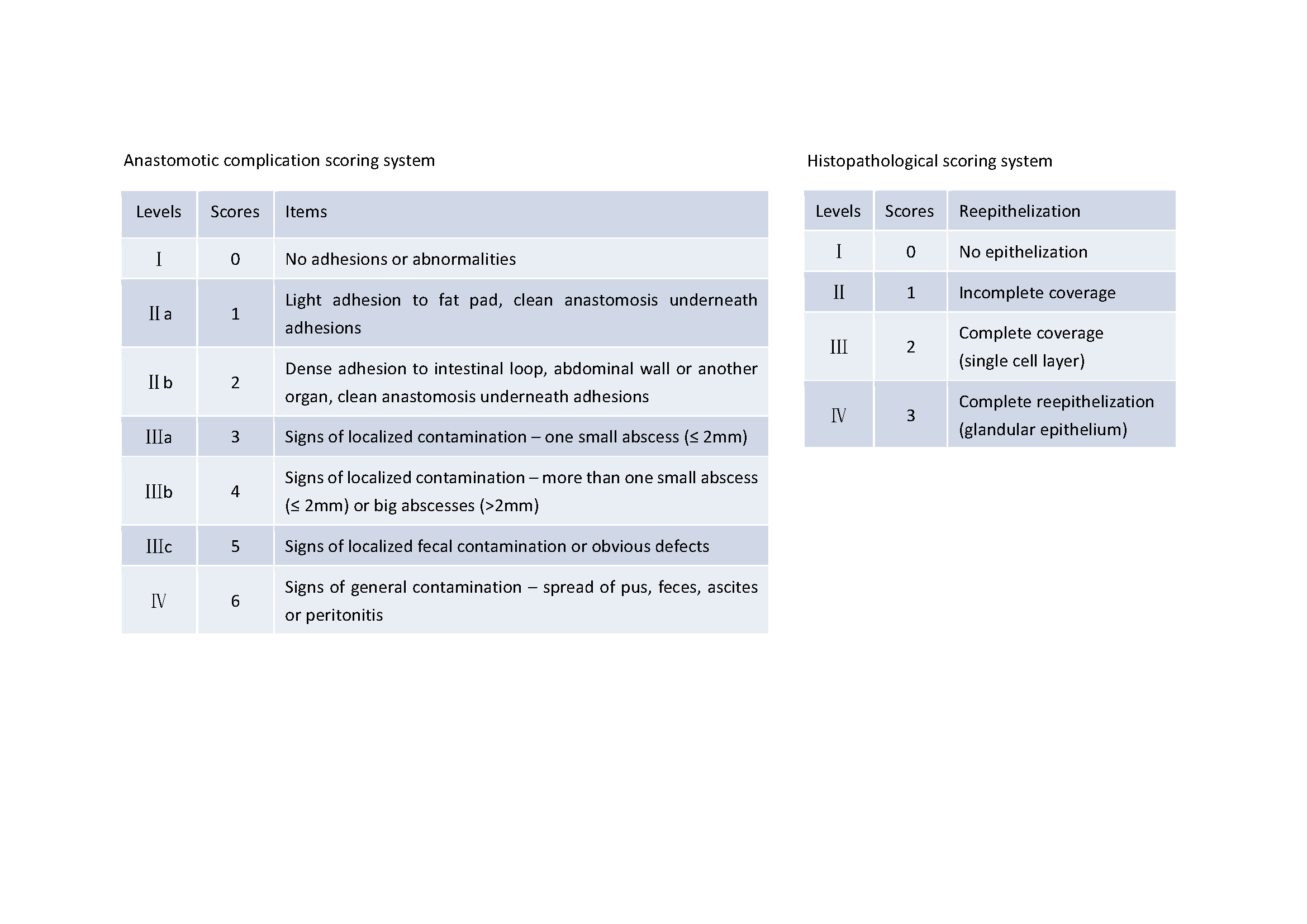
Methods:Firstly, a rat model of colon obstruction is established by placing a medical-grade silicone ring around the distal colon, obstructing the passage of fecal material. A sham colon obstruction model is created by placing the silicone ring beside the distal colon, allowing normal fecal passage. After 24 hours, rats undergo colon anastomotic surgery. The procedure involves resecting a 3mm segment of the descending colon including the obstructive part, followed by an end-to-end anastomosis using 8 polypropylene sutures. Secondly, all rat models with colon obstruction are established. Then anastomosis surgery was performed 24 hours later, at the same time, rats received topical injections of MSCs-derived sEVs into the subserosa, or an equal volume of normal saline as control. Rats are sacrificed after 4 days, and colon anastomosis healing is assessed.
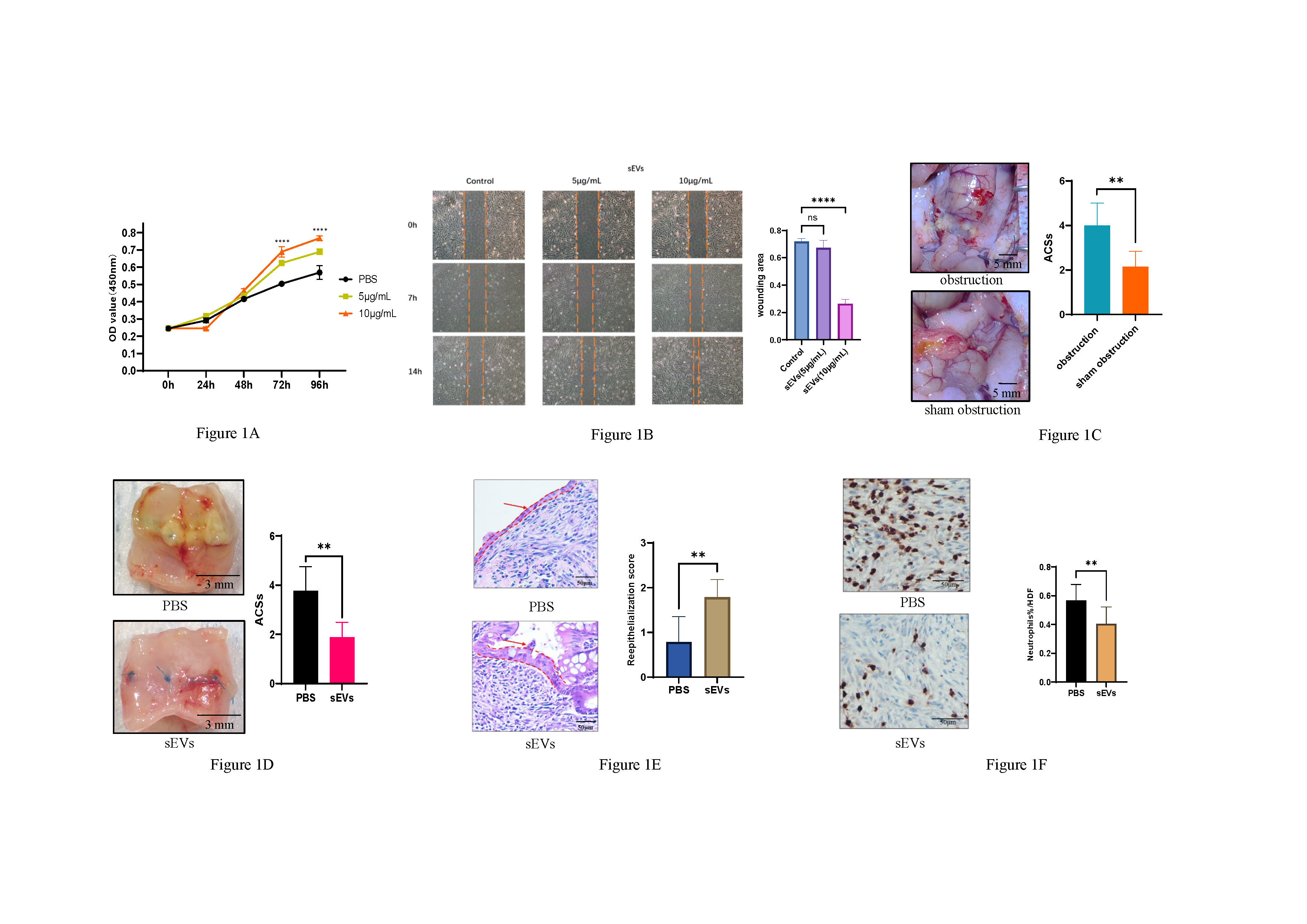
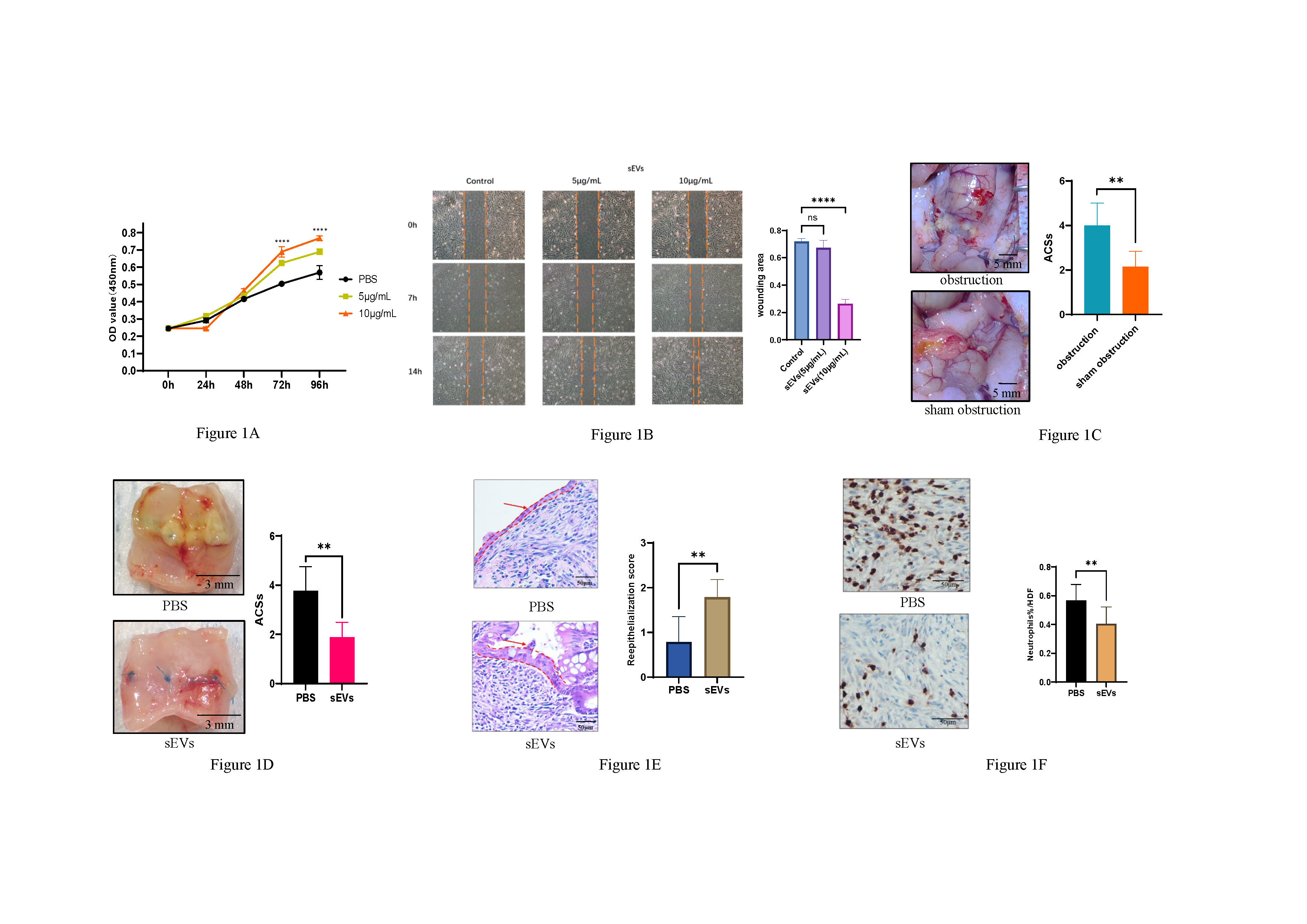
Results:The CCK8 assay demonstrated that MSCs-derived sEVs significantly enhance the proliferation of normal colon epithelial cells in vitro (Fig. 1A). Scratch assay performed on the CCD 841 CoN cell line revealed that MSCs-derived sEVs promoted faster wound closure (Fig. 1B). The colon obstruction rat models showed significantly higher scores on the anastomotic complication scoring system (ACSs) indicating a greater incidence of complications (Fig. 1C). However, the topical injection of MSCs-derived sEVs resulted in a reduction in the complication scores (Fig. 1D). Furthermore, Hematoxylin and Eosin (H&E) staining revealed that the epithelium on the anastomosis site was thicker and displayed a more normal morphology after treatment with MSCs-derived sEVs (Fig. 1E). Immunohistochemical (IHC) staining of Myeloperoxidase (MPO), a marker for neutrophils, demonstrated a significant reduction in neutrophil infiltration in the treated group (Fig. 1F).
Conclusions:In our study, we further investigated that colon obstruction can hinder the anastomosis healing. Importantly, our findings highlight the therapeutic potential of adipose MSCs-derived sEVs in promoting the healing of colon anastomosis by facilitating re-epithelialization and reducing inflammation.
Back to 2024 Abstracts