Back to 2024 Abstracts
INVERSE RELATIONSHIP BETWEEN INTRAVENOUS âBREAKTHROUGHâ? NARCOTICS AND TEXTBOOK OUTCOMES FOLLOWING COLORECTAL SURGERY
Nathaniel J. Schwartz
*1,3, Joseph Micheal
1,2, Jed Rosen
1, Lindsay V. Cromwell-Rims
1, Christopher R. D'Adamo
1,4, Jessica Felton
1, Joshua H. Wolf
11LifeBridge Health, Baltimore, MD; 2Xavier University School of Medicine, Oranjestad, Aruba; 3Touro College of Osteopathic Medicine, Middletown, NY; 4University of Maryland School of Medicine, Baltimore, MD
Background: Enhanced recovery after surgery (ERAS) has emerged as the standard of care for postoperative management of patients undergoing colorectal surgery and has led to improved outcomes. A central tenet of ERAS is reduction of overall narcotic use through multimodal pain management, but intravenous (IV) narcotics are typically still permitted for âbreakthroughâ? pain, i.e. pain that remains uncontrolled with other forms of postoperative analgesia. The aim of this study was to better understand the relationship between IV narcotics and postoperative outcome within the framework of a comprehensive ERAS program. Our hypothesis was that IV narcotics, though usually limited to âbreakthroughâ? dosing during the early postoperative period, would still be associated with adverse postoperative outcomes.
Methods: This is a retrospective study of patients within a single healthcare system who underwent elective colorectal surgery between 2020 and 2023. Patients were included if they participated in the hospital ERAS program, which included a multi-modal analgesic pathway. Emergency surgeries were excluded. Data regarding narcotic usage in the first 48 hours of surgery were compiled for each patient, and dosages for different narcotics were converted to morphine milligram equivalents (MME) to allow for comparison between patients. The primary outcome of interest was the ERAS textbook outcome (ERTO), which we have defined previously. An ERTO was defined as a 30-day postoperative course without readmission, reoperation, mortality, or morbidity (as defined by NSQIP), and a length of stay of <=3days. Associations between MME and ERTO were assessed using Student's t-test.
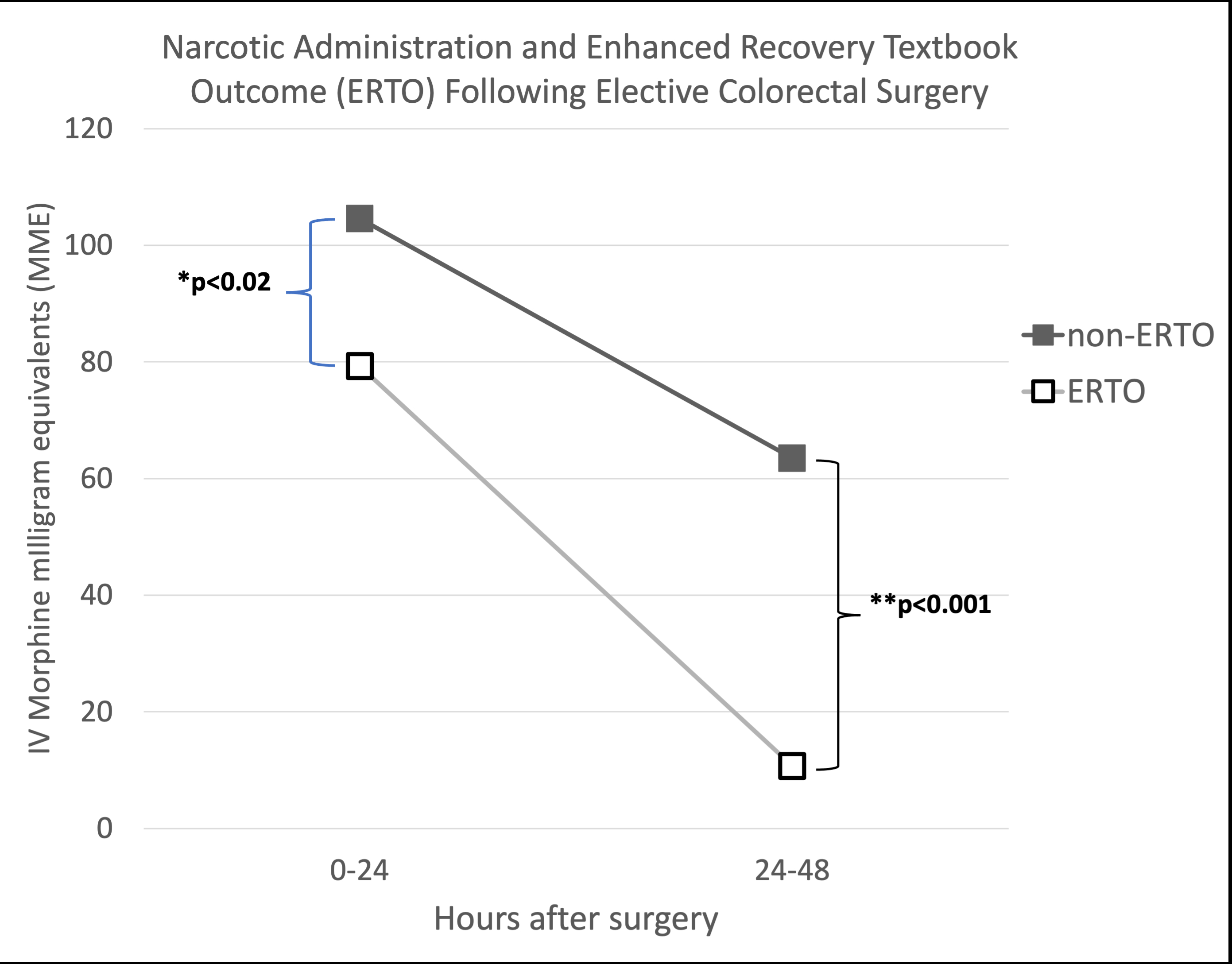
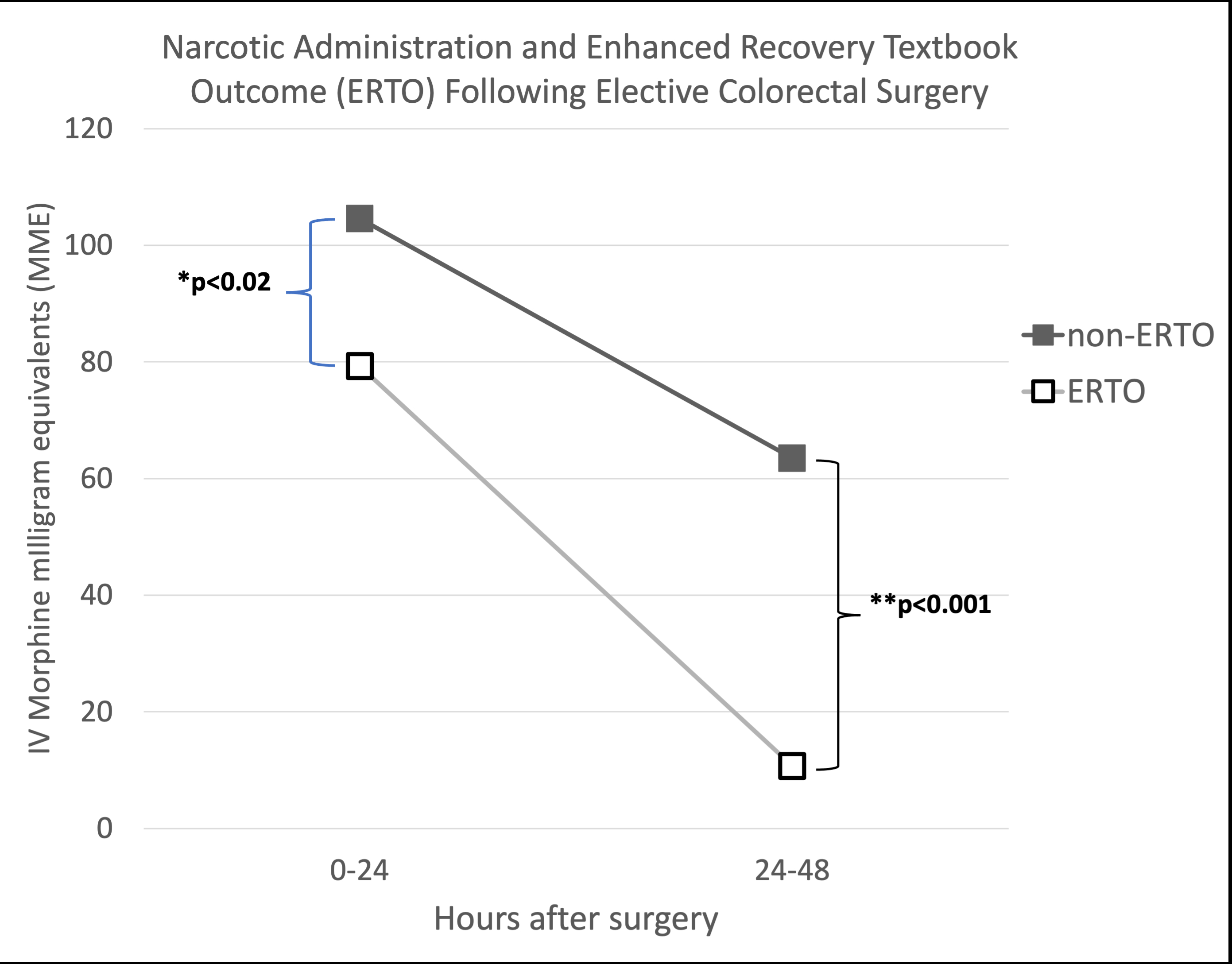
Results: A total of 315 patients were included in the study, 131 (42%) of whom had an ERTO. Average age among study patients was 60.4 (SD 15.7) years. ERTO patients had significantly lower mean intravenous (IV) narcotic usage within 24 (89.6 vs. 108.1 MME, p=0.02) and 24-48 (10.7 vs. 63.4 MME, p<0.001) hours after surgery compared to non-ERTO patients. Mean PO narcotic doses were comparable between ERTO and non-ERTO patients (24 hours: 23.7 vs. 19.1 MME, p=0.06; 24-48 hours: 23.4 vs. 28.2 MME, p=0.6). Total (IV plus PO) narcotic administration was similar between ERTO and non-ERTO patients at 24 hours (102.9 vs. 123.6 MME, p=0.07) and lower in the ERTO group at 24-48 hours (135.9 vs. 215.0 MME, p=0.001)(Figure 1).
Conclusions: Decreased intake of IV narcotics during the first 48 hours after colorectal surgery was significantly associated with ERTO. These findings suggest that IV narcotic administration for "breakthrough" at very early postoperative time intervals is related to adverse outcomes at later timepoints. Structured ERAS programing with multimodal non-narcotic analgesic alternatives should be prioritized for colorectal patients to reduce IV opioid requirements.
Back to 2024 Abstracts