Back to 2024 Abstracts
PROSPECTIVE EVALUATION OF PROVIDER COMPLIANCE WITH RISK-STRATIFIED PANCREATECTOMY CLINICAL PATHWAYS
Reed I. Ayabe
*, Ching-Wei D. Tzeng, Laura R. Prakash, Elsa M. Arvide, Morgan L. Bruno, Whitney L. Dewhurst, Michael P. Kim, Naruhiko Ikoma, Rebecca A. Snyder, Jeffrey E. Lee, Matthew Katz, Jessica E. Maxwell
Surgical Oncology, The University of Texas MD Anderson Cancer Center, Houston, TX
Background: Risk-stratified pancreatectomy clinical pathways (RSPCP) are associated with reduced length of stay (LOS) and major complications. Imperfect provider compliance is expected as RSPCP are guidelines for patient expectations, provider order standardization, and trainee education; however, the association of pathway adherence to postoperative outcomes has never been examined prospectively and remains uncertain. Within this context, this prospective quality improvement study evaluated provider compliance with discrete pathway components and the association of compliance with postoperative outcomes.
Methods: Compliance with published RSPCP components, including postoperative day (POD)1-3 diet advancement, reduced intravenous (IV) fluids, POD1 nasogastric tube (NGT) and POD1-3 drain removal, POD1-2 transition to oral medications, and immediate venous thromboembolic prophylaxis, was prospectively recorded from 4/2022-7/2023. Reasons for pathway deviation were categorized and recorded at the time of occurrence and evaluated for associations with index LOS and 90-day outcomes.
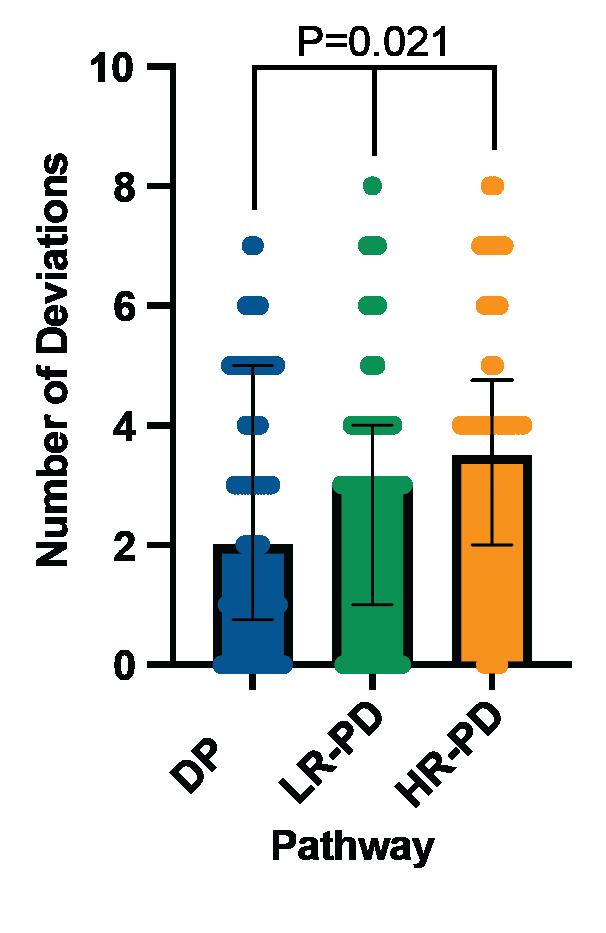
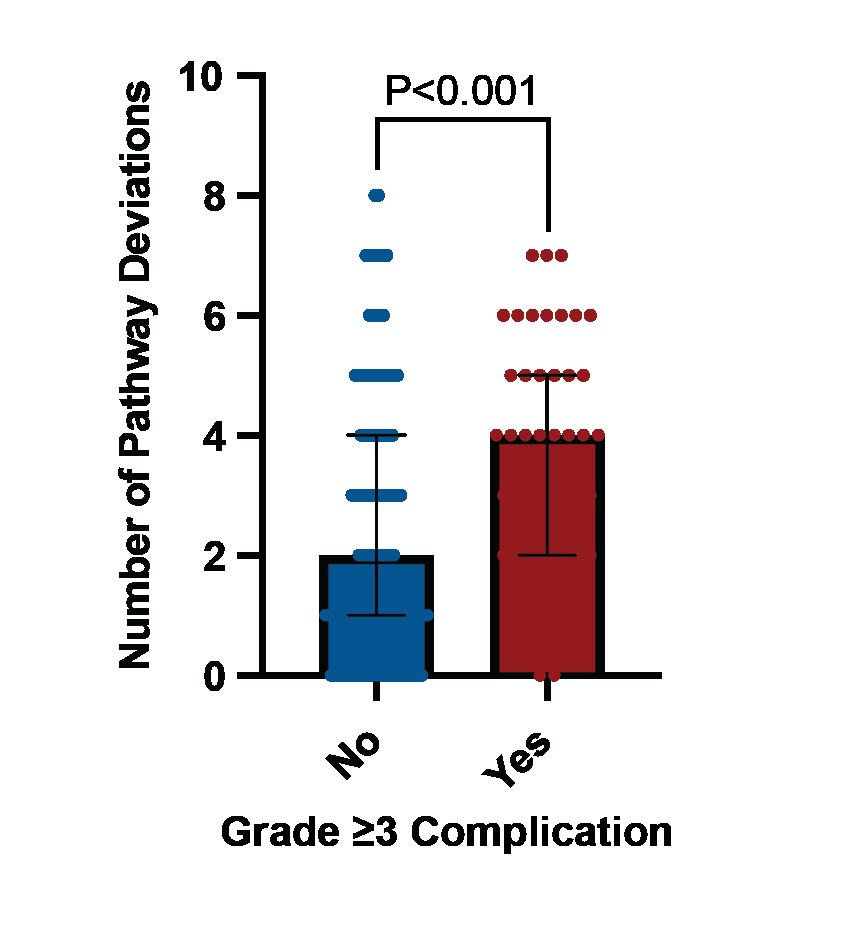
Results: Of 221 total cases, 82 were distal pancreatectomies (DP) with median LOS 4 days (IQR2-6), 83 were low-risk pancreatoduodenectomies (LR-PD) with median LOS 4 days (IQR2-6), and 56 were high-risk PD (HR-PD) with median LOS 5 days (IQR2-8). Pathway compliance was 100% for only 42 patients (19%). The median number of per-patient deviations increased with complexity of operation (DP 2 deviations, IQR1-5; LR-PD 3 deviations, IQR1-4; HR-PD 3.5 deviations, IQR2-5; P=0.021) (Figure 1). The most common deviations were IV fluids beyond POD2 (46%) and delayed transition to oral medications (45%). Patients with ≥1 pathway deviation (delays in advancement of care) had a significantly longer LOS (5days [IQR4-6] vs 4days [IQR3-4], P<0.001) and a higher rate of ACCORDION grade ≥3 complications (31% vs 7%, P<0.001) (Figure 2), but no reduction in readmission rate, delayed gastric emptying (DGE), or grade B/C fistula. Most common reasons for pathway deviation were delayed return of bowel function (31%), additional interventional drains (23%), and provider preference (23%). By multiple linear regression, initiation of a clear liquid diet by POD1 (after required 8am NGT removal) was associated with a shorter LOS (coefficient 3.361, P=0.018).
Conclusions: Pathway deviations are more common in high-risk PD and are associated with longer LOS and more major complications. While most pathway non-compliance is driven by patient condition, provider preference still affects almost one-fourth of patients, with delays in advancement not reducing DGE, B/C fistulas, or readmissions. While perfect RSPCP compliance is not a realistic goal, improved standardization and engagement of all clinical stakeholders in pathway revision and implementation are critical to iteratively improve patient outcomes.
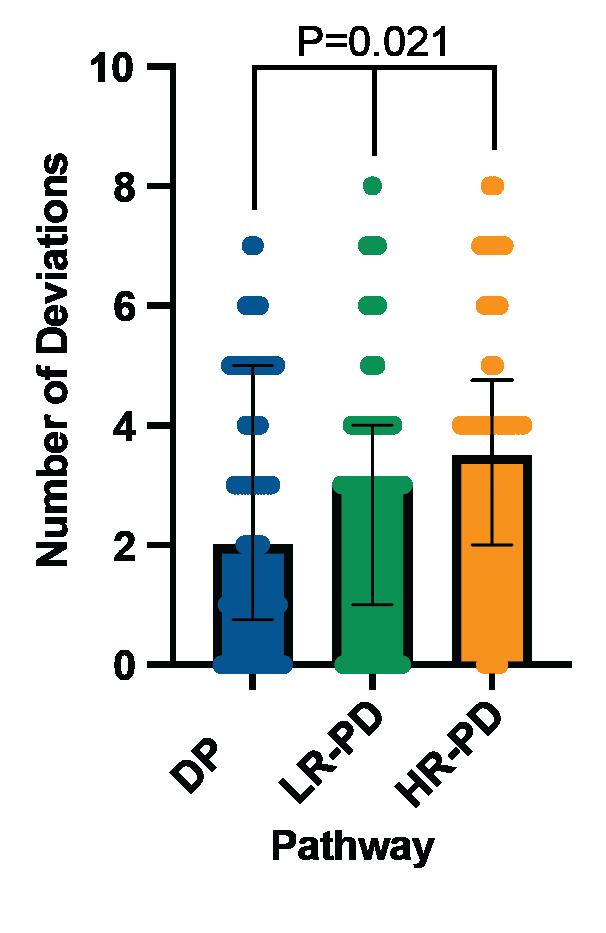 Figure 1
Figure 1: Number of pathway deviations stratified by RSPCP.
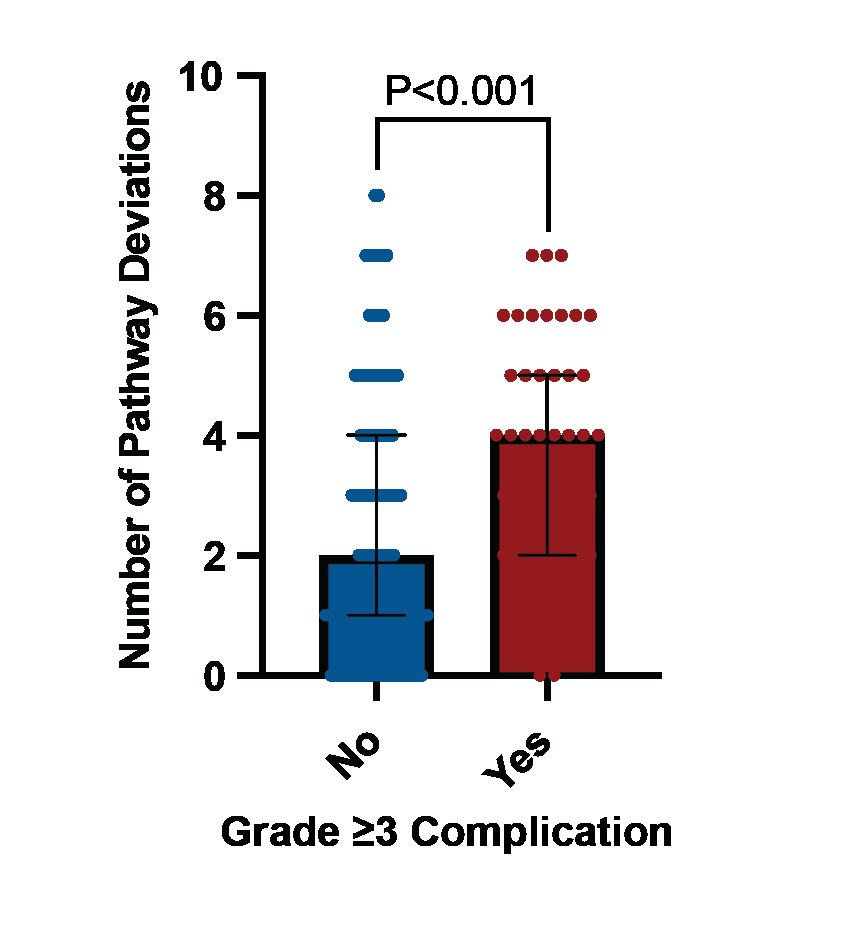 Figure 2
Figure 2: Number of pathway deviations in patients with and without ACCORDION grade ≥3 complications.
Back to 2024 Abstracts