Back to 2024 Abstracts
ADJUVANT CHEMOTHERAPY IS NOT ASSOCIATED WITH IMPROVED OVERALL SURVIVAL IN PATIENTS WITH PANCREATIC DUCTAL ADENOCARCINOMA WITH PERSISTENT LYMPHOVASCULAR INVASION OR LYMPH NODE INVOLVEMENT AFTER NEOADJUVANT CHEMOTHERAPY
Valerie Armstrong
*, Yu-Hui Chang, Akash Kartik, Chee-Chee Stucky, Rish Pai, Mohamad B. Sonbol, Christina Wu, Mitesh Borad, Tanios Bekaii-Saab, Nabil Wasif, Zhi Ven Fong
Surgical Oncology, Mayo Clinic Arizona, Scottsdale, AZ
IntroductionThe role of adjuvant chemotherapy (AC) after neoadjuvant treatment (NAT) for patients with pancreatic ductal adenocarcinoma (PDAC) is not well-defined. The aim of this study is to determine the impact of AC on overall survival (OS) for patients with persistent lymphovascular invasion (LVI) and lymph node (LN) involvement after NAT.
MethodsPatients with stage I-III PDAC who underwent surgical resection at US hospitals reporting to the National Cancer Database from 2010 to 2020 were identified. A multilevel, mixed-effects Cox multivariable regression model was used to assess for adjusted between-group differences in OS. An interaction term between LVI or LN involvement and AC use was utilized to test the potential benefit of the selective use of AC in patients after NAT. Landmark analyses set at 6-months were performed to minimize immortal time bias.
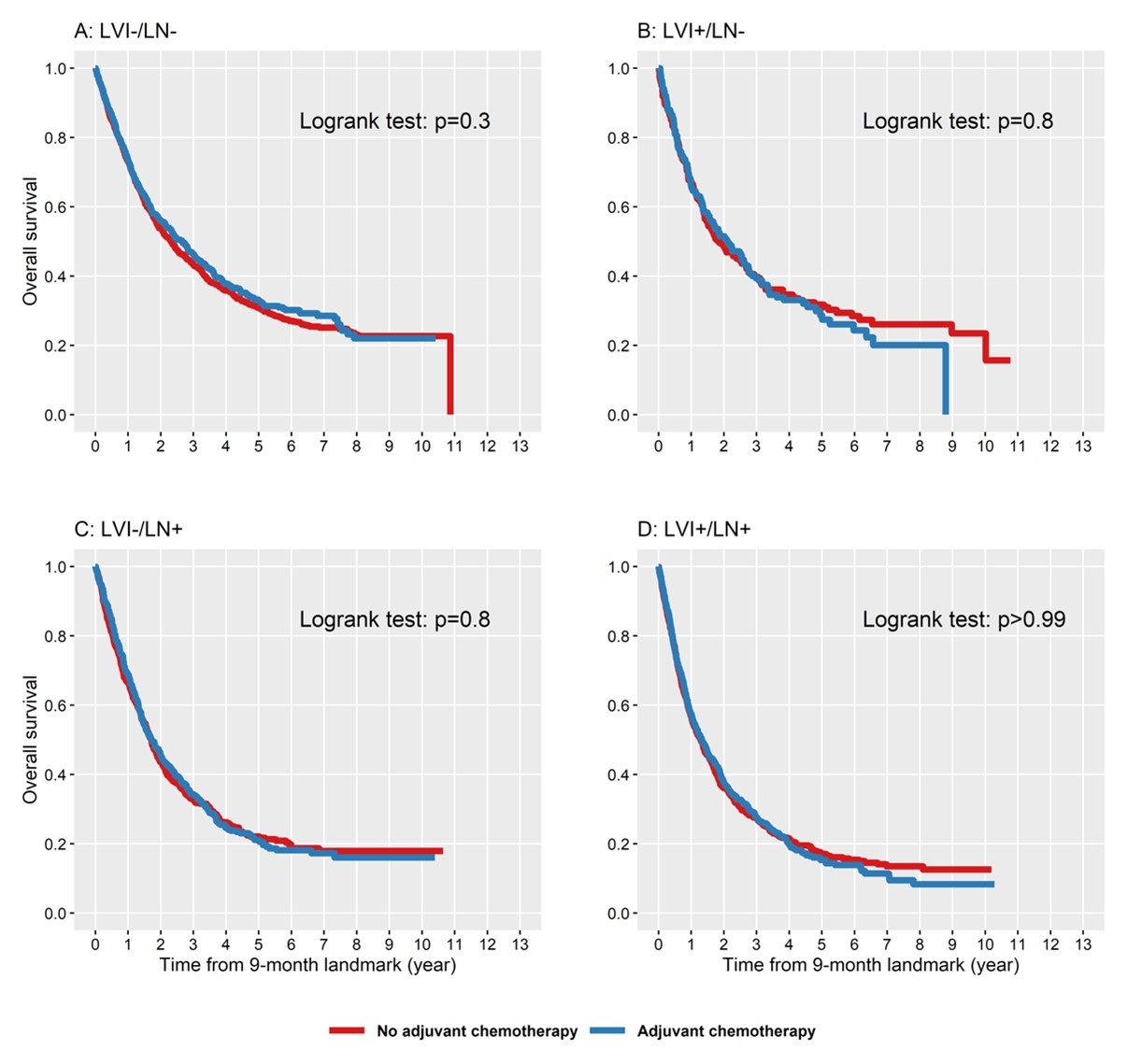
ResultsA total of 47,896 patients were included; group A (LVI-, LN-) had 12,570 patients, group B (LVI+, LN-) 3,767, group C (LVI-, LN+) 11,093, and group D (LVI+, LN+) 20,466. Median OS differed significantly between groups, with group A having the most favorable survival (37.2 months), followed by group B (26.7 months), group C (22.7 months), and group D (18.6 months,
p<0.01). A total of 7,445 patients received NAT, of whom 2,781 (37.4%) received AT. On multivariable analysis, the interaction term for LVI or LN involvement and AC in patients who had NAT was not associated with OS (group A, HR 0.96,
p=0.47; group B and C, HR 1.05,
p=0.57; group D, HR 0.99,
p=0.89).
ConclusionsLVI and LN involvement are independently associated with worse OS in patients with resected PDAC. After NAT, the use of AC in patients with persistent LVI and LN involvement was not associated with improved OS. The incongruency in these findings between “real-world� data and institutional series should be an impetus for future clinical trials to be conducted to better inform clinicians on how to appropriately select patients for additional cytotoxic but potentially efficacious AC after NAT.
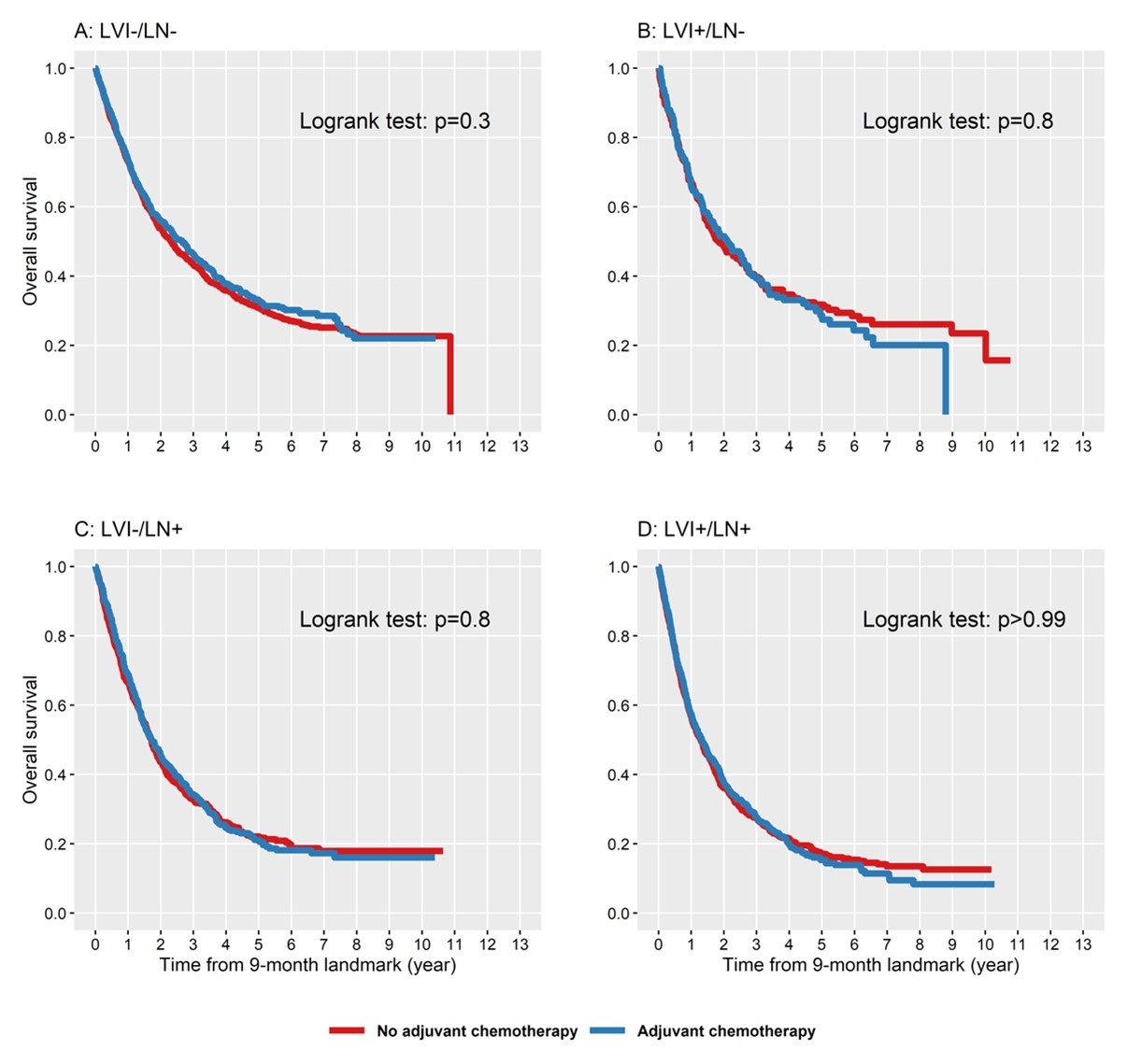
Kaplan-Meier curves comparing those who received adjuvant chemotherapy to those who received no adjuvant chemotherapy.
Back to 2024 Abstracts