Back to 2024 Abstracts
SUPERBUGS VS. OLD GUARD: PIPERACILLIN-TAZOBACTAM TAKES ON TRADITION IN SURGICAL PROPHYLAXIS DURING PANCREATODUODENECTOMY: A META-ANALYSIS
Kumar Jayant
*1,2, Isabella Reccia
3, Adriano Carneiro
5, Mauro Podda
4, Francesco Virdis
6, Nikolaos Machairas
7, David Nasralla
8, Kenneth K. Poon
1, Ramesh P. Arasaradnam
9, Christopher J. Gannon
1, John Fung
10, Nagy Habib
2, Omar H. Llaguna
11Surgical oncology, Memorial Healthcare System, Hollywood, FL; 2Imperial College London Faculty of Medicine, London, London, United Kingdom; 3Policlinico ponte, San Pietro, Bergamo, Italy; 4calgiari UNiversity Hospital, Calgiari, Italy; 5Universidade Federal de Pernambuco, Recife, PE, Brazil; 6Dipartimento DEA-EAS Ospedale Niguarda Ca' Granda, Milano, Italy; 7Ethniko kai Kapodistriako Panepistemio Athenon, Athens, Greece; 8Royal Free London NHS Foundation Trust, London, United Kingdom; 9University of Warwick Medical School, Coventry, United Kingdom; 10University of Chicago Pritzker School of Medicine, Chicago, IL
Introduction: Pancreatoduodenectomy (PD) is unique in its surgical complexity, notably marked by extensive preoperative biliary manipulation. Furthermore, a substantial body of research has highlighted the prevalence of Enterococcus and Enterobacter species in both biliary cultures and surgical wound specimens. This highlights the insufficiency of conventional prophylactic measures. Consequently, the primary objective of our study was to evaluate the outcomes of antimicrobial prophylaxis involving piperacillin + tazobactam [PT] in comparison to the use of traditional antibiotics [TA], including cefoxitin/ceftriaxone/cefmetazole/cefazolin/ampicillin+sulbactum
Methods: Following PROSPERO registration CRD-42023479100 a systematic database search was conducted for literature published between 2000 and 2023. MeSH terms included: antimicrobial prophylaxis AND prophylaxis, antimicrobial and matched with the following keywords: (“pancreatectomy� OR “pancreatoduodenectomy� OR “duodenopancreatectomy � OR “pancreatic surgery�). All data analyses were conducted using RevMan 5.4 according to published guidelines in Cochrane review.
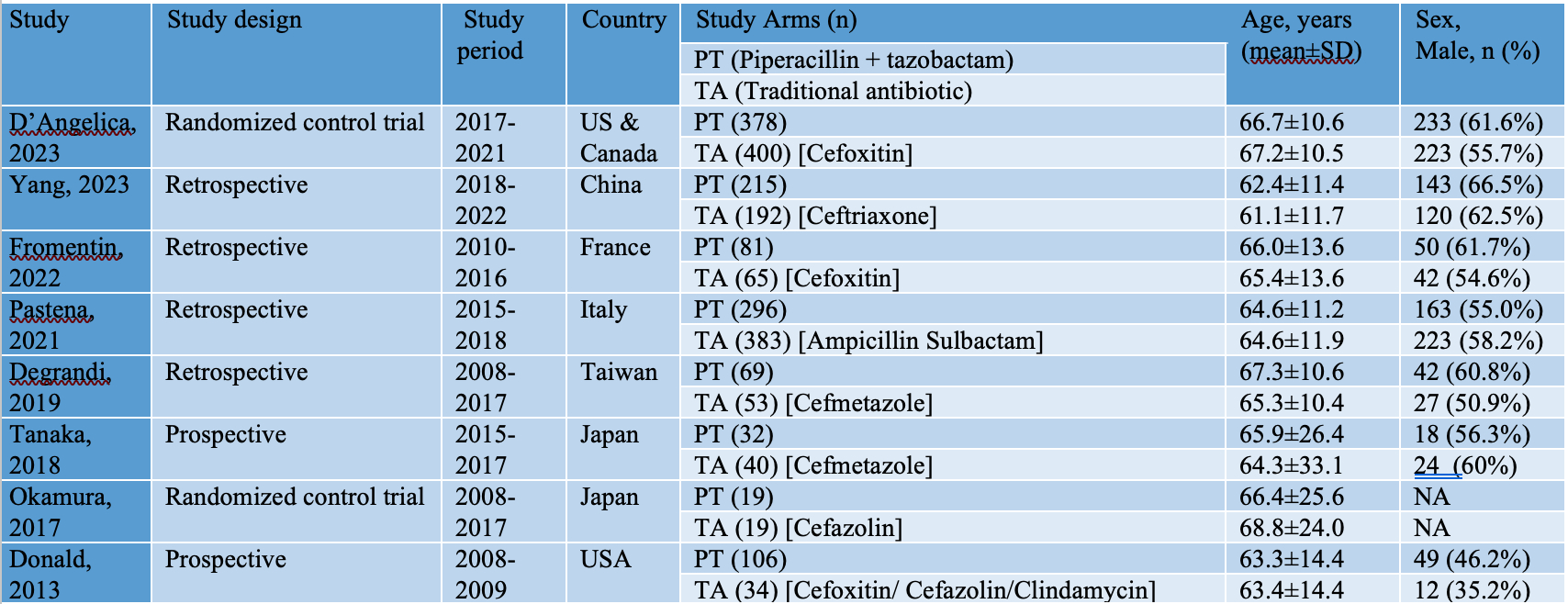
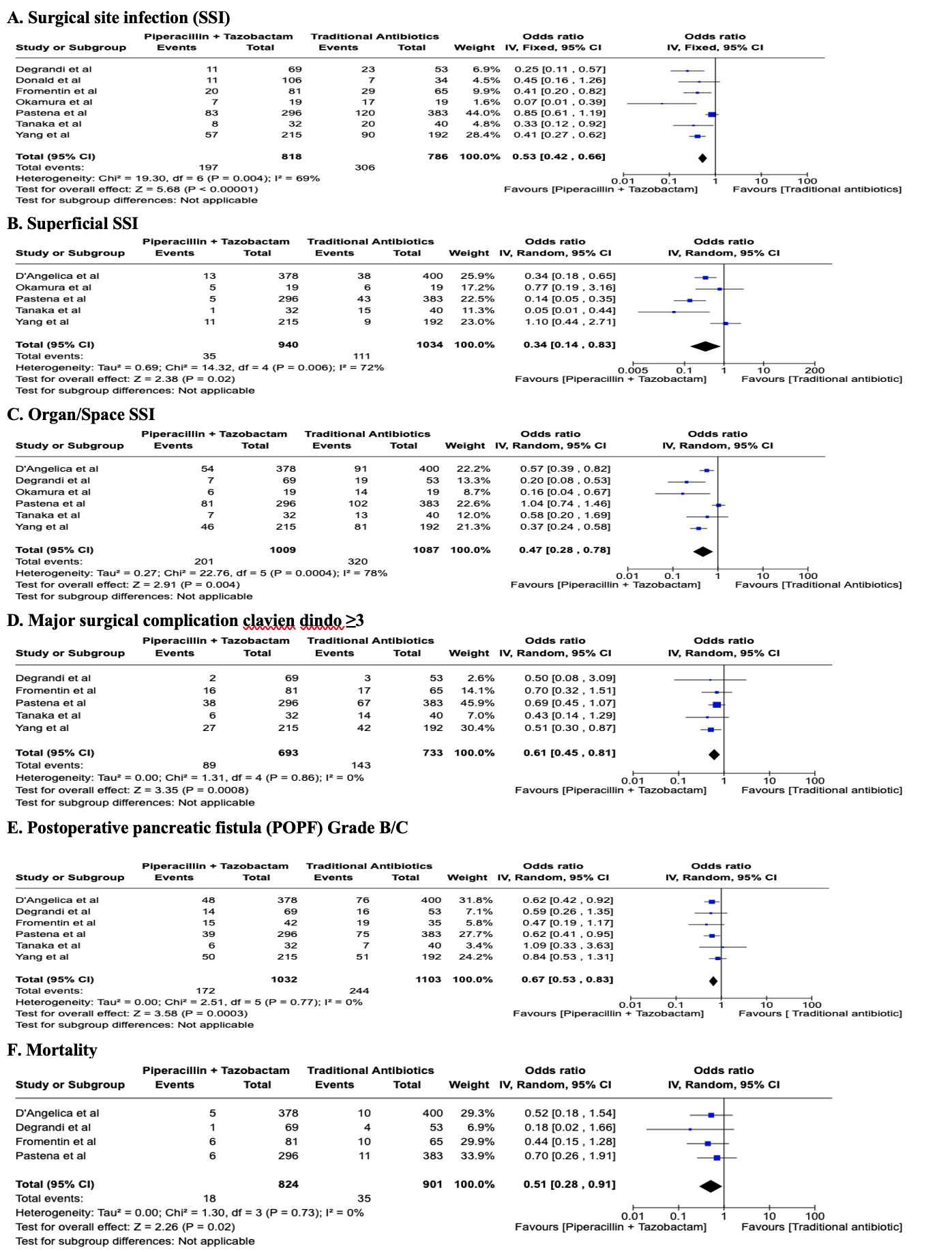
Results: Eight studies with 2382 patients who underwent PD, who received either piperacillin + tazobactam [PT group- 1196 patients) or Traditional antibiotics [TA group- 1186 patients) and submitted for a meta-analysis (Table 1). Both groups were comparable in terms of preoperative biliary drainage [(OR 1.06 (0.89-0.27); P- value 0.5]. Patients in TA group had significantly less surgical site infection (SSI) and major surgical complication clavien dindo ≥3 [OR 0.34 (0.14-0.83); P – value 0.02) and OR 0.61 (0.45-0.83); P-value 0.00]. Further, subgroup analysis of SSI, highlighted significantly less superficial and organ/space SSI in PT group. Further, analysis also demonstrated significantly lower clinically relevant postoperative pancreatic fistula (POPF) grade B/C and mortality [OR 0.67 (0.53-0.83); P – value 0.00) and OR 0.51 (0.28-0.91); P-value 0.02] (Fig 1).
Conclusions:Perioperative piperacillin-tazobactam as antimicrobial prophylaxis lowers the risk of postoperative SSI, major surgical complications ≥3, POPF grade B/C, and mortality, hence supports the adoption of piperacillin-tazobactam for surgical prophylaxis in open pancreatoduodenectomy.
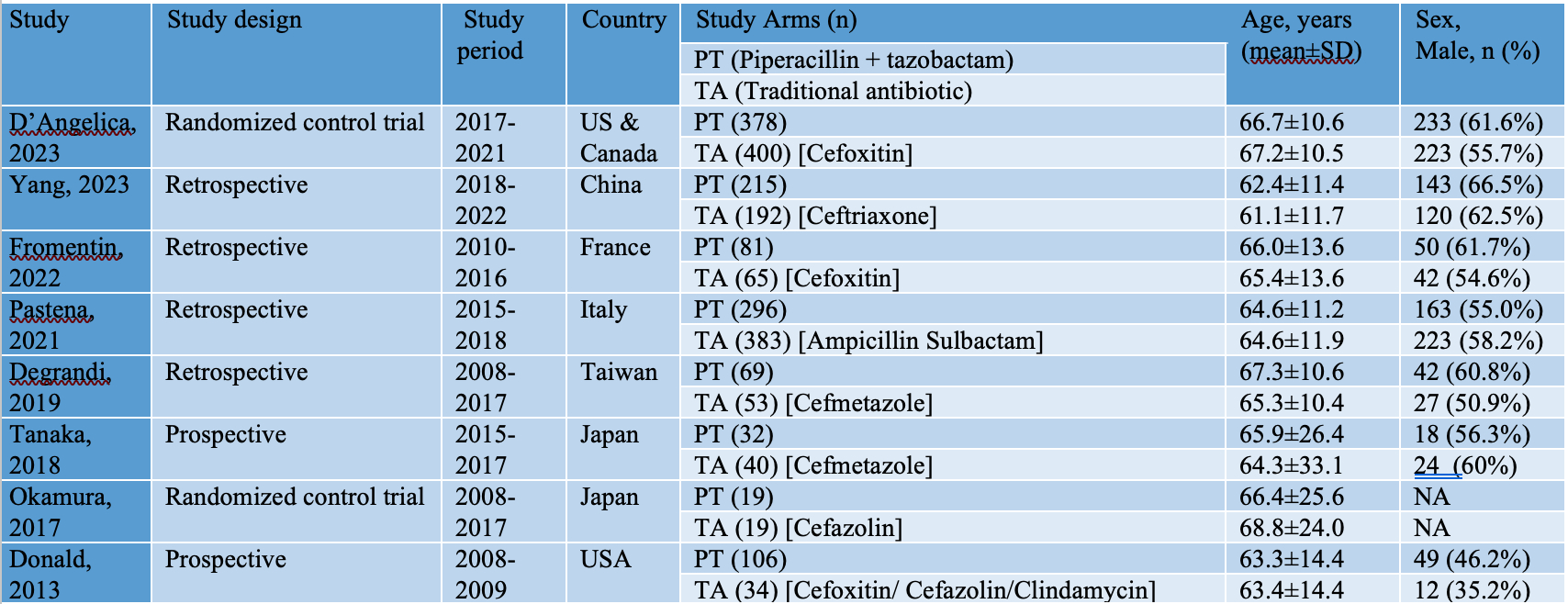
Details of included studies and participant characteristics
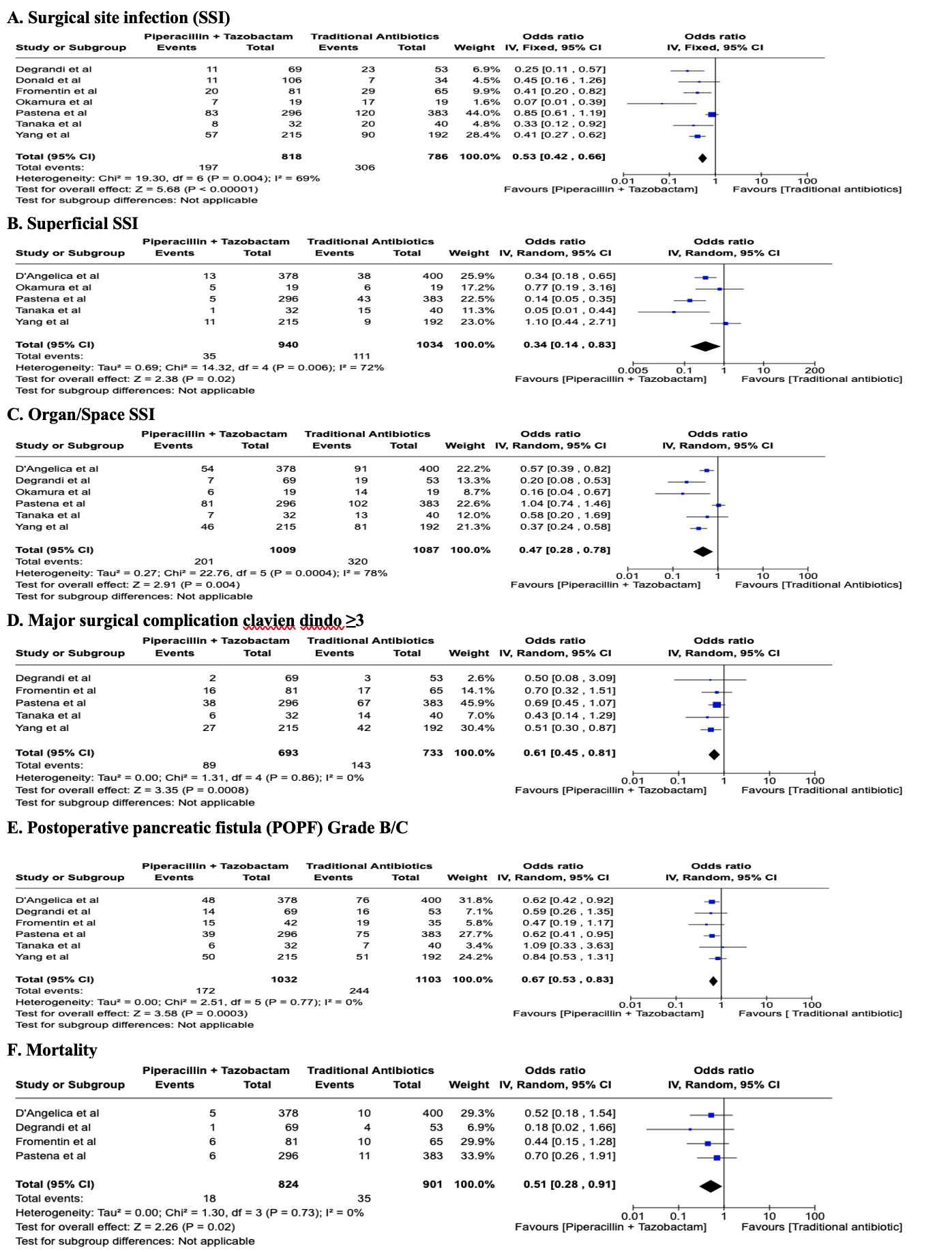
Forest plot depicting significantly lower oberved outcomes in pipercillin + tazobactum group including overall SSI, superfical SSI, organ/space SSI, major surgical complication clavien dindo ≥3, postoperative pancreatic fistula (POPF) Grade B/C and mortality.
The size of the squares depicts the effects while comparing the weight of the study in the meta-analysis. The diamond shows the significant favor towards the PT group following random effects analysis. A 95% confidence interval is represented by horizontal bars.
Back to 2024 Abstracts