Back to 2024 Abstracts
POST-PANCREATECTOMY READMISSION CLASSIFICATION SYSTEM PROVIDES FRAMEWORK FOR COST REDUCTION EFFORTS
Brittany C. Fields
*, Ahad M. Azimuddin, Artem Boyev, Laura R. Prakash, Jessica E. Maxwell, Naruhiko Ikoma, Rebecca A. Snyder, Michael P. Kim, Jeffrey E. Lee, Matthew Katz, Ching-Wei D. Tzeng
The University of Texas MD Anderson Cancer Center Division of Surgery, Houston, TX
Introduction Formerly validated risk-stratified pancreatectomy clinical pathways decreased index hospitalization stay without increasing readmissions, which remain major contributors to the financial burden of pancreatectomy. This study aims to define costs of three previously defined readmission categories (infectious [I]; technical [T], e.g., post-operative anastomotic leak; and medical/metabolic [M], e.g., failure to thrive, other non-infectious or non-technical cause) and the relative drivers.
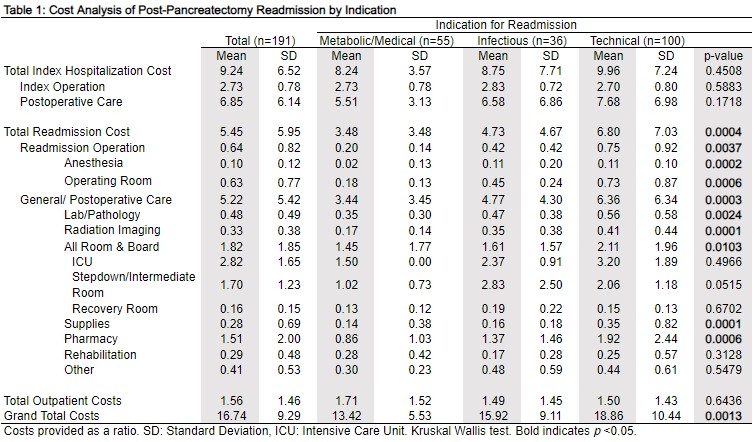
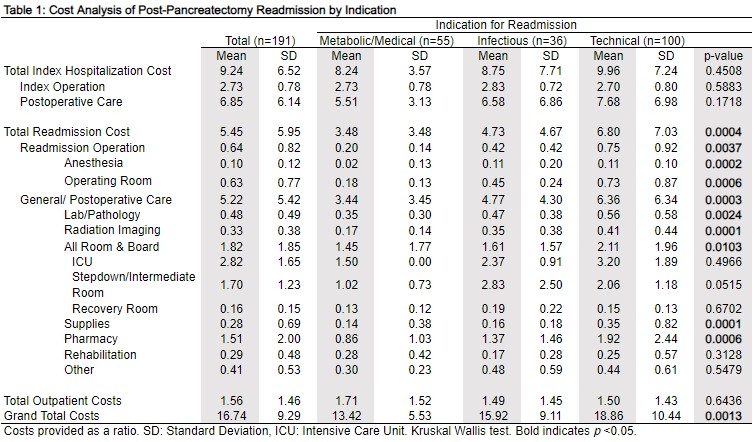
MethodsPatients with readmissions after pancreatectomy between 10/2016-12/2022 were identified using a prospectively maintained, single-institution database. The primary outcome was readmission cost, defined as summative hospital-based cost of any surgery-related or 90-day readmission. Costs were provided as a ratio (CR; mean service cost divided by mean cost of all operations at our center in fiscal year 2022) to protect proprietary financial data and compared between readmission categories.
ResultsOf 860 consecutive patients, 24.7% (212) were readmitted. Cost data were available for 90.1% (191/212). Readmissions were 28.8% medical (55/191), 18.8% infectious (36/191), and 52.4% technical (100/191). Median time to initial readmission after discharge was 8 (IQR 3-18) days. Multiple (≥2) readmissions were observed in 27.8% (53/191) of readmitted patients, most of which were technical (M: 17.0%, 9/53; I: 22.6%, 12/53; T: 60.4%, 32/53).
Mean CR was 5.45 for initial readmission. CR was highest for technical then infectious readmissions (M: 3.48, I: 4.73, T: 6.80) overall and in most subcategories (Table 1). For medical readmissions, “stepdown� (higher acuity observation) unit costs were highest (M: 2.83, I: 2.06, T: 1.02), thus their mean room/board costs approached that of technical readmissions (M: 1.24, I: 1.15, T: 1.28).
Few unplanned re-operations were required (2.1%, 4/191). Other invasive interventions were required for 48.7% (93/191), mostly technical or medical readmissions (T: 55.9%, 52/93; M: 29.0%, 27/93). Median initial readmission stay (6 [IQR 3-10] days, intervention vs. 3 [IQR 2-6] days, no intervention) and overall readmission CR (7.6, intervention vs. 3.0, no intervention; p<0.001) increased if invasive intervention was required. All subcategories demonstrated this trend except room/board, where CR was similar irrespective of need for intervention (1.1 vs. 1.3, respectively, p<0.001).
ConclusionsMost post-pancreatectomy readmissions are technical, requiring invasive intervention and costing nearly the equivalent of 2 medical readmissions. Multiple short-stay readmissions without intervention also have a cumulative cost. Clinical efforts increasing accessibility of outpatient management to prevent short-stay readmissions, and/or reducing invasive interventions may further alleviate the financial burden of post-pancreatectomy care.
Back to 2024 Abstracts