Back to 2024 Abstracts
IDENTIFYING PRE AND POSTOPERATIVE CHARACTERISTICS OF PATIENTS UNABLE TO RETURN TO INTENDED ONCOLOGICAL THERAPY AFTER DISTAL PANCREATECTOMY FOR ADENOCARCINOMA
Vasalya Panchumarthi
*1, Grace C. Bloomfield
1, Piyush Gupta
2, Matthew Luckman
1, Jean Namgoong
1, Thomas Fishbein
2, Pejman Radkani
2, Emily R. Winslow
31Georgetown University School of Medicine, Washington, ; 2MedStar Georgetown University Hospital, Washington, ; 3University of Wisconsin-Madison, Madison, WI
IntroductionUnlike pancreatic head tumors, there has been a slower shift towards a neoadjuvant approach in treating distal adenocarcinomas. With the traditional sequence of surgery followed by adjuvant therapy, it is important to consider delays in recovery that could preclude initiation of systemic therapy. We therefore examined the frequency and factors leading to delayed recovery in patients with distal tumors who were selected for a surgery first approach.
MethodsThis retrospective study identified all patients who underwent distal pancreatomy between 2017 and 2023. Demographic, clinical, and outcome data were collected from the electronic medical record. We defined adequate recovery as discharge from the surgical clinic without residual nutritional, infectious or wound healing issues by 12 weeks postoperatively. Elevations in preoperative CA 19-9 were dichotomized (≥800).
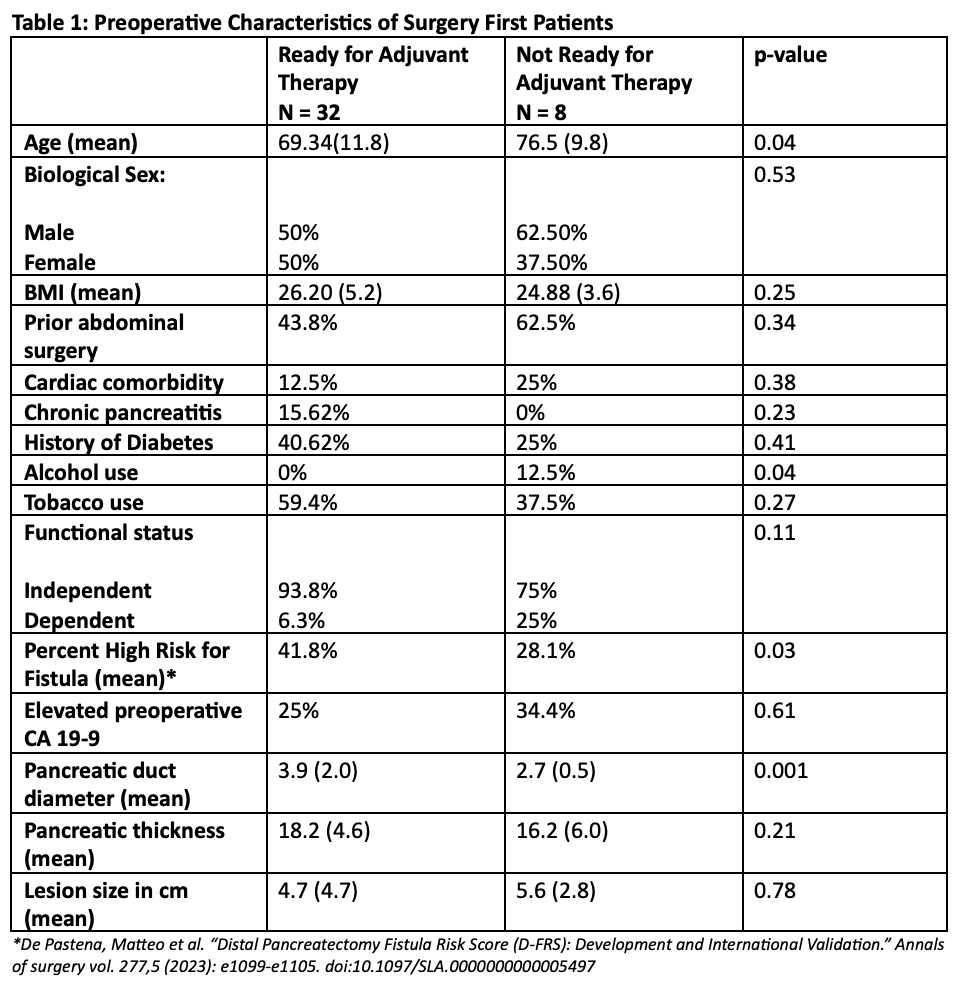
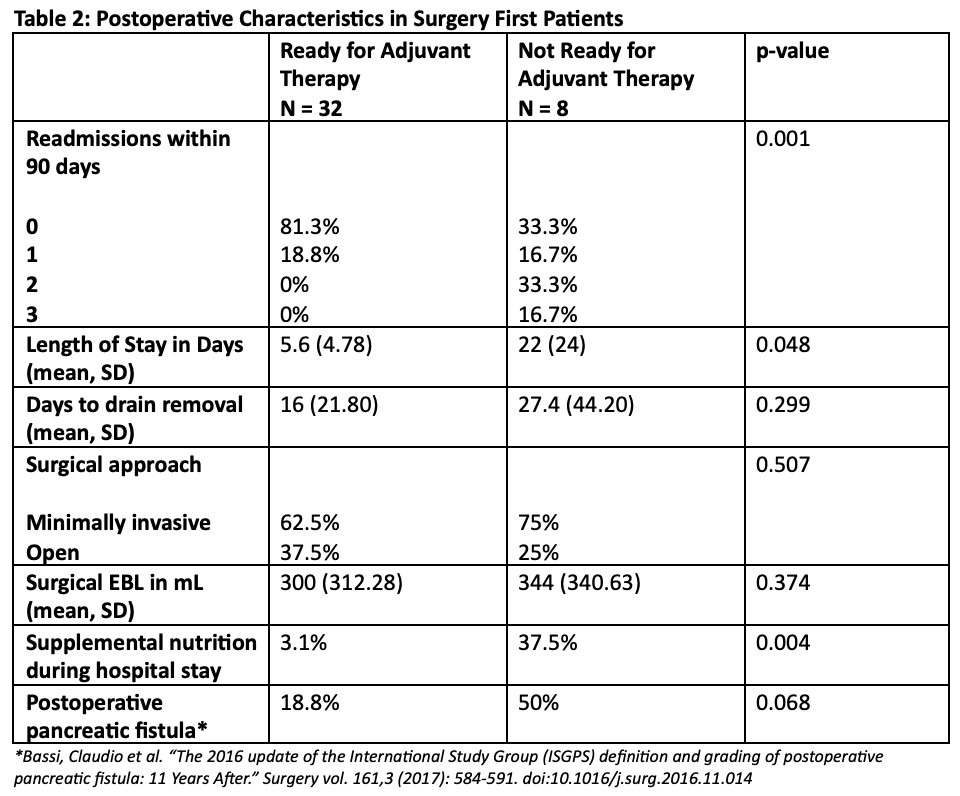
ResultsOf the 556 patients in the database, 180 patients had left pancreatectomies, of which 55 had pancreatic adenocarcinoma. Among the 55 patients, 15 (27%) received neoadjuvant therapy (NAT) and 40 (73%) were selected for a surgery first approach. The average age was 69 ± 11.5 yrs. The average BMI was 26.11 ± 4.9. There were statistically significant differences in the tumor size (4.9 cm surgery first vs 3.3 cm NAT, p=0.04) and pancreatic duct diameter (3.6 mm surgery first vs 2.9 mm NAT; p=0.03) between those selected for NAT over a surgery first approach. Among the 40 patients who had surgery first, 32 patients (80%) recovered to receive adjuvant therapy within 12 weeks (Table 1). The preoperative variables associated with delayed recovery included advanced age (76 vs 69 years, p=0.04), alcohol use (12.5% vs 0%, p=0.04), and smaller pancreatic duct diameter (2.7 vs 3.9 mm, p-0.001). Postoperative variables associated with delayed recovery include longer hospital stay (22 vs 5 days, p=0.04), readmission (67% vs 19%, p=0.001), and supplemental nutrition (38% vs 3%, p=0.004). Delays in recovery were attributable to pre-existing medical conditions in 3 patients, stroke in 1 patient, delayed wound healing in 1 and 3 delayed mortalities (1 cardiopulmonary, 1 sepsis and 1 oncologic).
ConclusionUntil further evidence emerges on neoadjuvant therapy for distal pancreatic adenocarcinoma, patients and surgeons must carefully consider risks and benefits of each approach. In this study, we found that 80% of patients recovered to initiate adjuvant therapy. Preoperative predictors of longer postoperative recovery were advanced age, alcohol use, and smaller pancreatic duct diameter. However, examination of neoadjuvant strategies continues to need additional data on the pragmatic outcomes of patients selected for a surgery first approach based on subtle preoperative factors and explicit shared decision making.
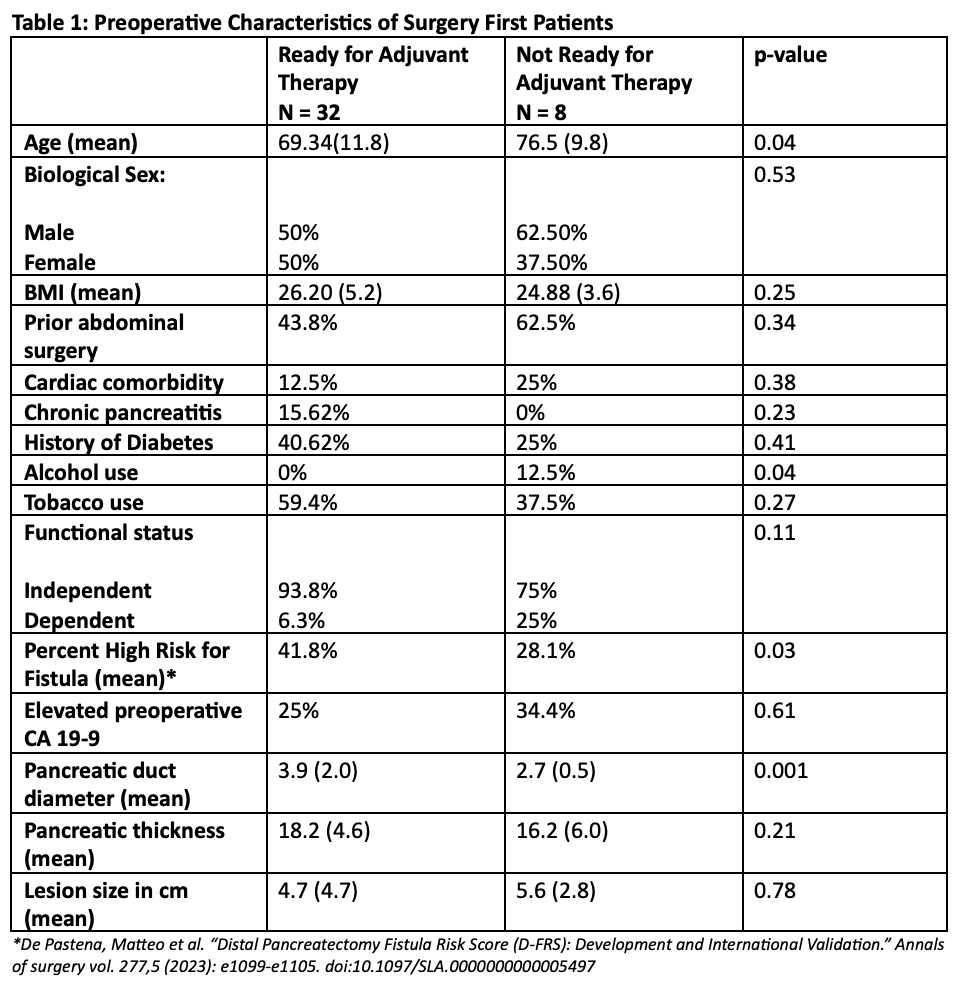 Preoperative Characteristics in Surgery First Patients
Preoperative Characteristics in Surgery First Patients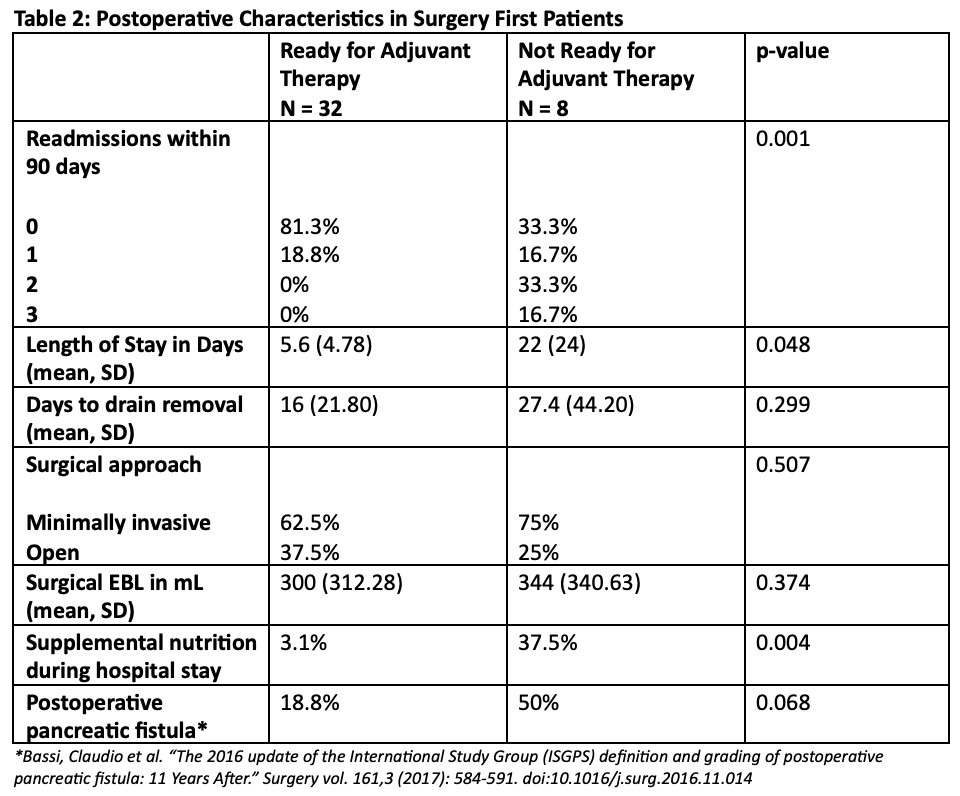 Postoperative Characteristics in Surgery First Patients
Postoperative Characteristics in Surgery First Patients
Back to 2024 Abstracts