Back to 2024 Abstracts
ENDOSCOPIC ULTRASOUND (EUS) BETTER PREDICTS TUMOR SIZE AND VASCULAR INVOLVEMENT COMPARED TO CROSS-SECTIONAL IMAGING IN PANCREATIC CANCER
Rachel C. Kim
*1, Jackson A. Baril
1, Ryan J. Ellis
1, Thomas K. Maatman
1, Alexandra M. Roch
1, Eugene P. Ceppa
1, Nicholas J. Zyromski
1, Attila Nakeeb
2, Michael G. House
1, C. Max Schmidt
1, Aditya Gutta
1, Trang Nguyen
11Surgery, Indiana University School of Medicine, Indianapolis, IN; 2Lahey Hospital and Medical Center, Burlington, MA
Background: Accurate clinical staging plays a key role in the multimodal treatment of pancreatic ductal adenocarcinoma (PDAC). The latest version of the American Joint Committee on Cancer staging guidelines for PDAC (8
th ed, 2016) shifted T-staging to be based primarily on tumor size, and patients with major vascular involvement benefit from neoadjuvant therapy. Patients without vascular involvement often undergo upfront resection, however subsequently demonstrate microscopic vascular involvement on pathology. While endoscopic ultrasound (EUS) is often utilized in the diagnosis of PDAC, cross-sectional imaging via CT or MRI is most used to assess tumor size and vascular involvement. In this study, we aim to compare the accuracy of EUS in the clinical staging of PDAC to that of CT/MRI.
Methods: All patients who underwent oncologic resection for PDAC between Jan 2017-May 2021 were reviewed from a prospectively-maintained database at a single, high-volume institution. Patients who underwent any neoadjuvant therapy prior to surgery and who were not evaluated by both cross-sectional imaging and EUS were excluded. Vascular involvement was confirmed on surgical pathology and was defined as any vascular invasion of tumor that extended to <1mm from the vascular groove.
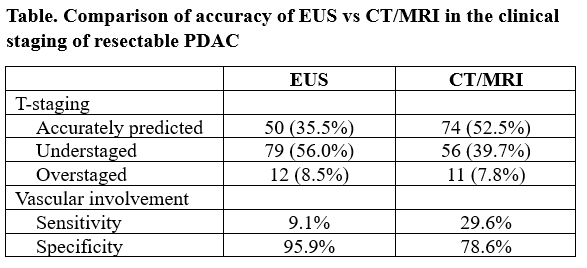
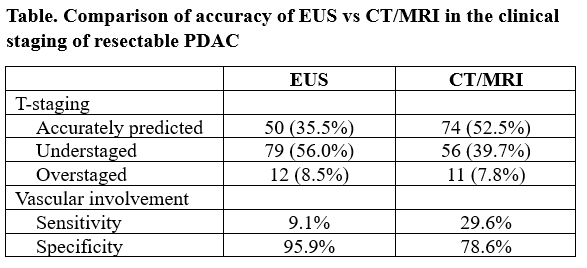
Results: Of the 141 patients included in this study, 22(15.6%) had T1 tumors, 81(57.4%) T2, and 36(25.5%) T3 on pathology. Forty-four(31.2%) patients had both preoperative CT and MRI, 89(63.1%) had CT only, and 6(4.3%) had MRI only. CT/MRI accurately predicted T-staging in 50(35.5%) patients, understaged in 79(56%), and overstaged in 12(8.5%). In comparison, EUS more accurately predicted pathologic T-stage in 74(52.5%) of patients (understaged–56(39.7%), overstaged – 11(7.8%), p<0.001). In terms of vascular involvement, although only 9 patients required major vein resection, a total of 44(31.2%) of patients had pathologic evidence of tumor extension to the vascular groove. CT/MRI predicted this with a sensitivity of 9.1% and specificity 95.9%, while EUS demonstrated a 3-fold increase in sensitivity of 29.6% and specificity of 78.6%. When using both CT/MRI and EUS, the sensitivity was 31.8% and specificity was 77.3%.
Conclusions: While CT/MRI was highly specific, EUS was approximately 3-fold more sensitive than cross-sectional imaging for predicting vascular involvement in the clinical staging of PDAC prior to upfront surgical resection. Additionally, EUS significantly more accurately predicted pathologic T-stage based on the new AJCC staging guidelines. Both cross-sectional imaging and endosonographic evaluation should be carefully considered in the clinical evaluation and subsequent treatment planning of patients with PDAC.
Back to 2024 Abstracts