Back to 2024 Abstracts
IDEAL OUTCOME POST-PANCREATODUODENECTOMY: A COMPREHENSIVE HEALTHCARE SYSTEM ANALYSIS
Abdullah Khalid
*1, Lyudmyla Demyan
1, Shamsher Pasha
2, Elliot Newman
1, Matthew Weiss
1, Daniel A. King
1, Marcovalerio Melis
11Surgery, Northwell Health, New Hyde Park, NY; 2The University of Texas Health Science Center at San Antonio, San Antonio, TX
Introduction:
Indicators such as mortality and complications are commonly used to measure quality of care. However, a more informative and comprehensive assessment of surgical quality c is better captured using composite outcome measures such as Textbook Outcome (TO),Optimal Pancreatic Surgery, and a newer consolidated metric, the 'Ideal Outcome' (IO) measure. We reviewed our institutional experience, to assess the impact of various demographics, comorbidities, and operative variables on achieving IO after a pancreatoduodenectomy (PD).
Methods:
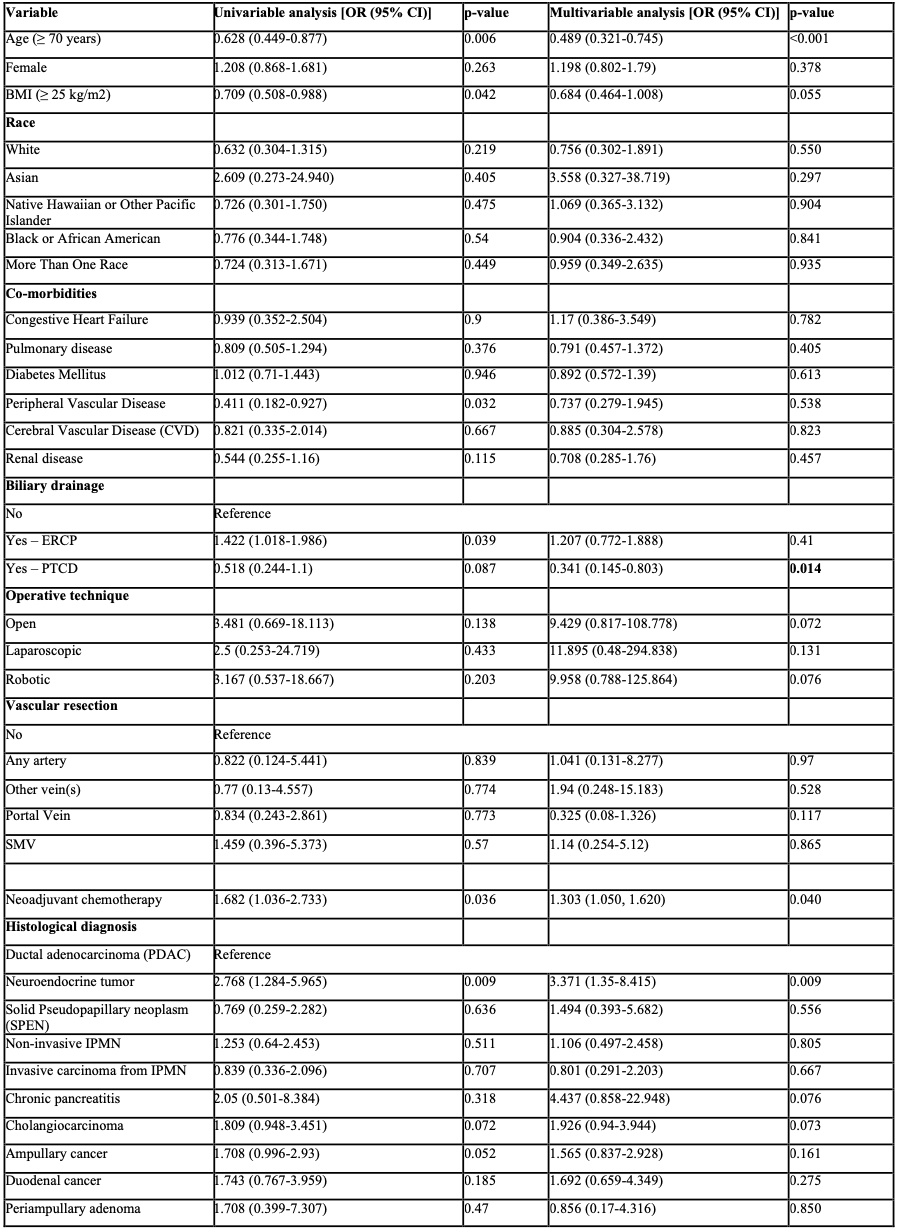
A retrospective analysis was conducted on patients who underwent PD at Northwell Health facilities between 2009 to 2023. IO is defined by the absence of six adverse events: (1) in-hospital mortality, (2) severe complications—Clavien-Dindo ≥3, (3) postoperative pancreatic fistula grade B and above, (4) reoperation, (5) hospital stay >75th percentile, and (6) readmission within 30 days of discharge. Logistic regression models were employed for both univariable and multivariable analyses to evaluate the impact of demographic, co-morbidities, and operative variables on achieving IO.
Results:
From a total of 578 patients who underwent Pancreatoduodenectomy (PD), 330 (57.1%) achieved the Ideal Outcome (IO). In the multivariable analysis, factors associated with increased odds of achieving IO included neoadjuvant chemotherapy (OR 1.303, 95% CI 1.050-1.620) and the presence of neuroendocrine tumors (OR 3.371, 95% CI 1.35-8.415). Conversely, factors such as preoperative percutaneous biliary drainage (PTCD) (OR 0.341, 95% CI 0.145-0.803) and older age (≥ 70 years) (OR 0.489, 95% CI 0.321-0.745) were associated with decreased odds of achieving IO.
Conclusion:
The consolidated composite measure for IO provides a robust tool for evaluating and benchmarking outcomes post-Pancreatoduodenectomy (PD). Identification of factors associated with IO, such as age, neoadjuvant chemotherapy, PTCD, and specific histological diagnoses may offer a foundation for targeted interventions, which, along with quality improvement initiatives should aim to enhance patient outcomes after PD by focusing on modifiable factors and informed clinical decision-making.
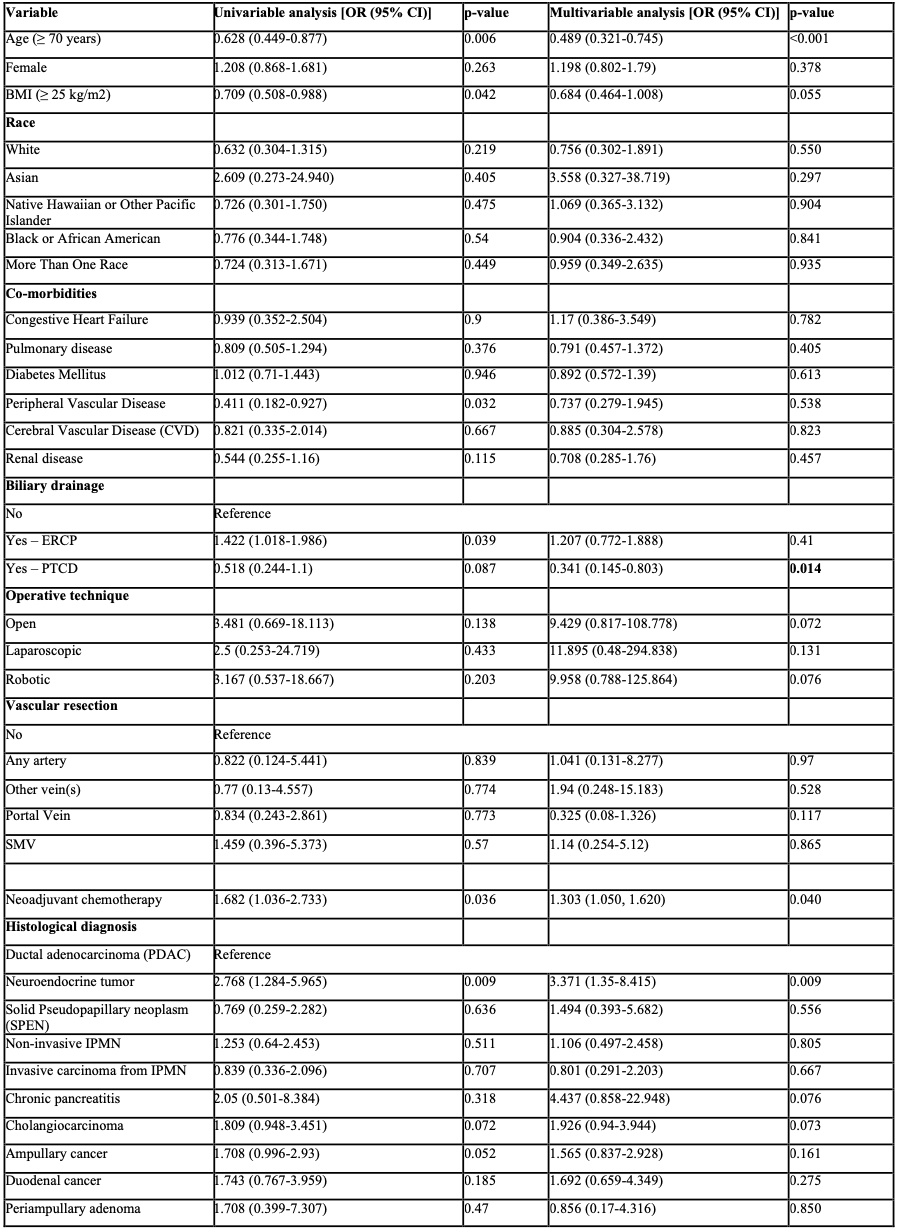 Table 1
Table 1. Logistic Regression Analysis of Factors Influencing Ideal Outcome Post-Pancreatoduodenectomy.
Back to 2024 Abstracts