Back to 2024 Abstracts
PROPHYLACTIC ENDOLUMINAL NEGATIVE PRESSURE VACUUM THERAPY AFTER MINIMALLY INVASIVE ESOPHAGECTOMY: A PILOT STUDY
Kunal J. Patel
*1, Andrew Hawkins
2, Evan Rotar
2, Christopher Scott
21Surgery, Duke University Health System, Durham, NC; 2UVA Health, Charlottesville, VA
Purpose: Negative pressure wound therapy (NPWT) is a popular treatment for esophageal perforations and anastomotic leaks. In recent years, NPWT has increasingly been used prophylactically for incisional wounds and even colorectal anastomoses. Given the high anastomotic leak rate after esophagectomy (especially salvage), we investigated the role for routine prophylactic endoluminal NPWT.
Methods: Single center retrospective case series of consecutive patients undergoing esophagectomy between February 2022 and July 2023. All patients underwent a totally robotic-assisted minimally invasive esophagectomy with a single surgeon with trainees, utilizing a linear stapled intrathoracic anastomosis. Prophylactic endoluminal NPWT was utilized via a nasogastric tube that was placed under direct visualization at the time of surgery and correctly positioned after completion of the anastomosis. Evaluation was completed on postoperative day five with an EGD, removal of the NPWT, and on-table fluoroscopic esophagram.
Results: During the collection period, eight esophagectomies were performed utilizing prophylactic NPWT. The average BMI was 27.6. All patients underwent neoadjuvant chemoradiotherapy. Five patients were considered salvage esophagectomies (average days from neoadjuvant treatment completion to surgery was 201.8 days (range 86-342 days). Four patients had prior gastric surgery (3 gastrostomy tubes, 1 hiatal hernia repair/Nissen). Three of 8 patients had jejunostomy tubes post-operatively, two of which were present prior and the third converted from a gastrostomy tube. The remainder were maintained NPO until anastomotic evaluation. None of the 8 patients in the study experienced an anastomotic leak, either at the time of evaluation or on longitudinal follow up (range 1-17 months). To date, no patient has experienced a symptomatic or clinically relevant stricture requiring intervention. The average diet on hospital discharge was a thickened liquid diet, although 3/8 patients were discharged with a soft food diet. All patients were discharged by post operative day 9 (median length of stay was 8 days).
Conclusions: Anastomotic leak after esophagectomy is an all-too-common complication. We replaced our routine post-esophagectomy use of an NG tube with NPWT to promote anastomotic healing. While our current paradigm involved a second anesthesia event for removal, the outcomes of this small case series are very promising and warrant further investigation.
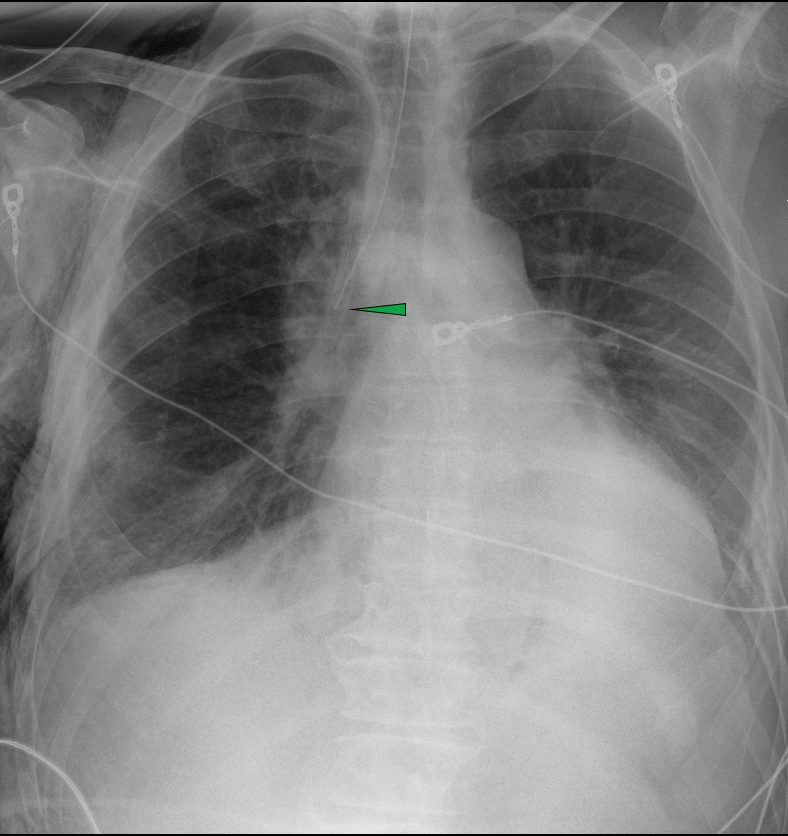
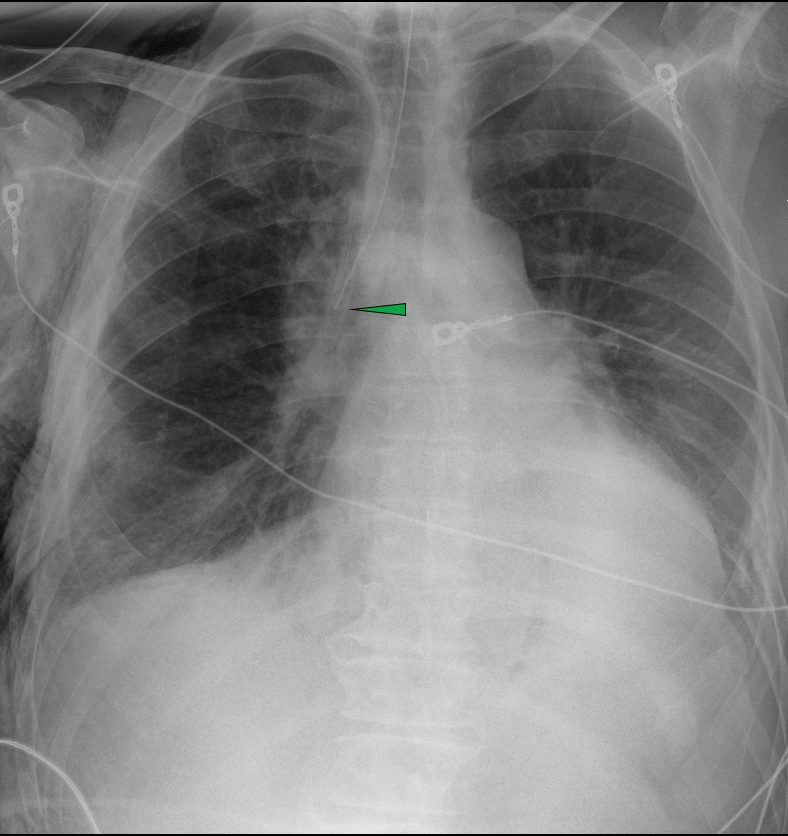
Post operative day #2 chest x-ray demonstrating the tip of the endoluminal negative pressure wound vacuum (nasograstric tube) terminating at the level of the carina where the esophagogastric anastomosis is located (green arrow). The distal gastric conduit is appropriately decompressed.
Back to 2024 Abstracts