Back to 2024 Abstracts
ROBOTIC AND MINIMALLY INVASIVE ESOPHAGECTOMY AND NEOADJUVANT TREATMENT RELATED DOWNSTAGING ARE ASSOCIATED WITH IMPROVED OVERALL SURVIVAL IN PATIENTS WITH ESOPHAGEAL ADENOCARCINOMA: A NATIONAL CANCER DATABASE STUDY (NCDB)
Eduardo A. Canto
*1,2, Matthew Reilly
2, Alexander Hall
1, Ryan W. Walters
1, Kalyana Nandipati
21Medicine, Creighton University School of Medicine, Omaha, NE; 2CHI Health Creighton University Medical Center Bergan Mercy, Omaha, NE
IntroductionEsophageal adenocarcinoma (EAC) has been associated with poor survival, with an estimated median survival of 15 months. Neoadjuvant chemoradiation (NCRT) followed by esophagectomy is considered the standard of care for locally advanced EAC. Esophagectomy has three surgical approaches: open (OE), minimally invasive (MIE), and robotic assisted minimally invasive (RAMIE). The role of the approach on survival in patients with neoadjuvant treatment has not been well established. The aim of the current study is to estimate the effect of pathological downstaging and surgical approach on survival outcomes in patients with EAC.
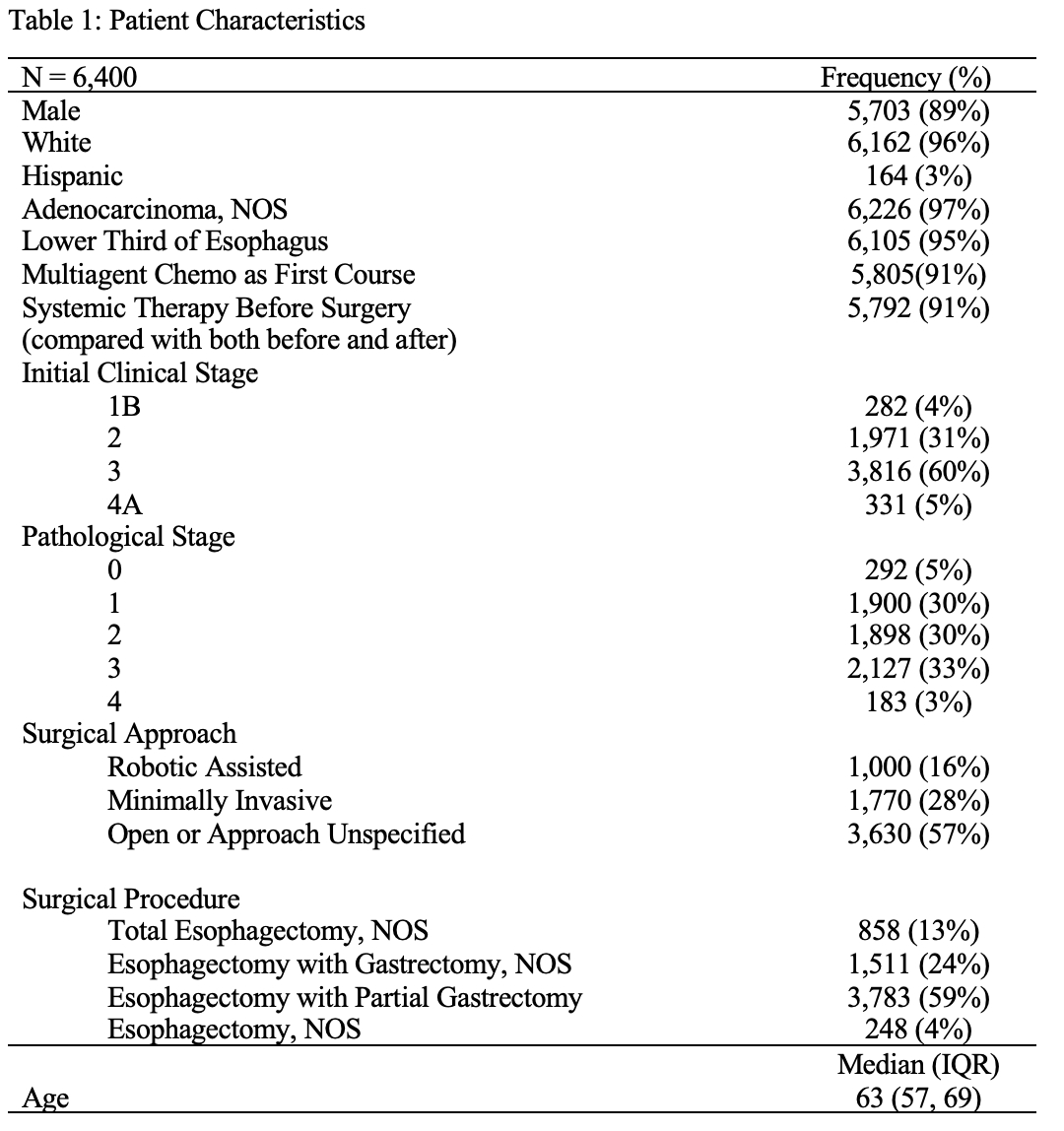
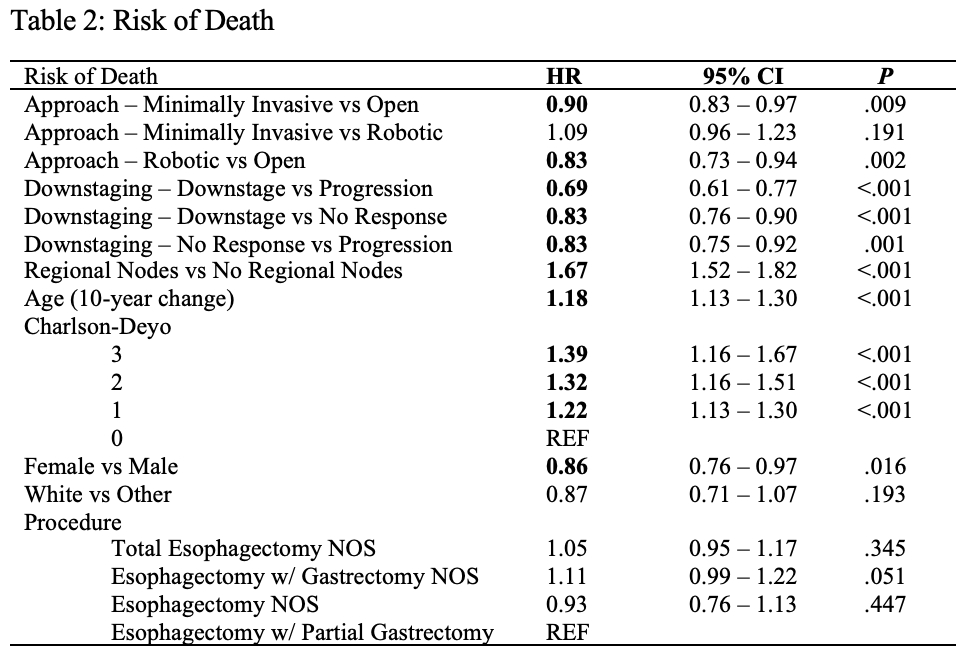
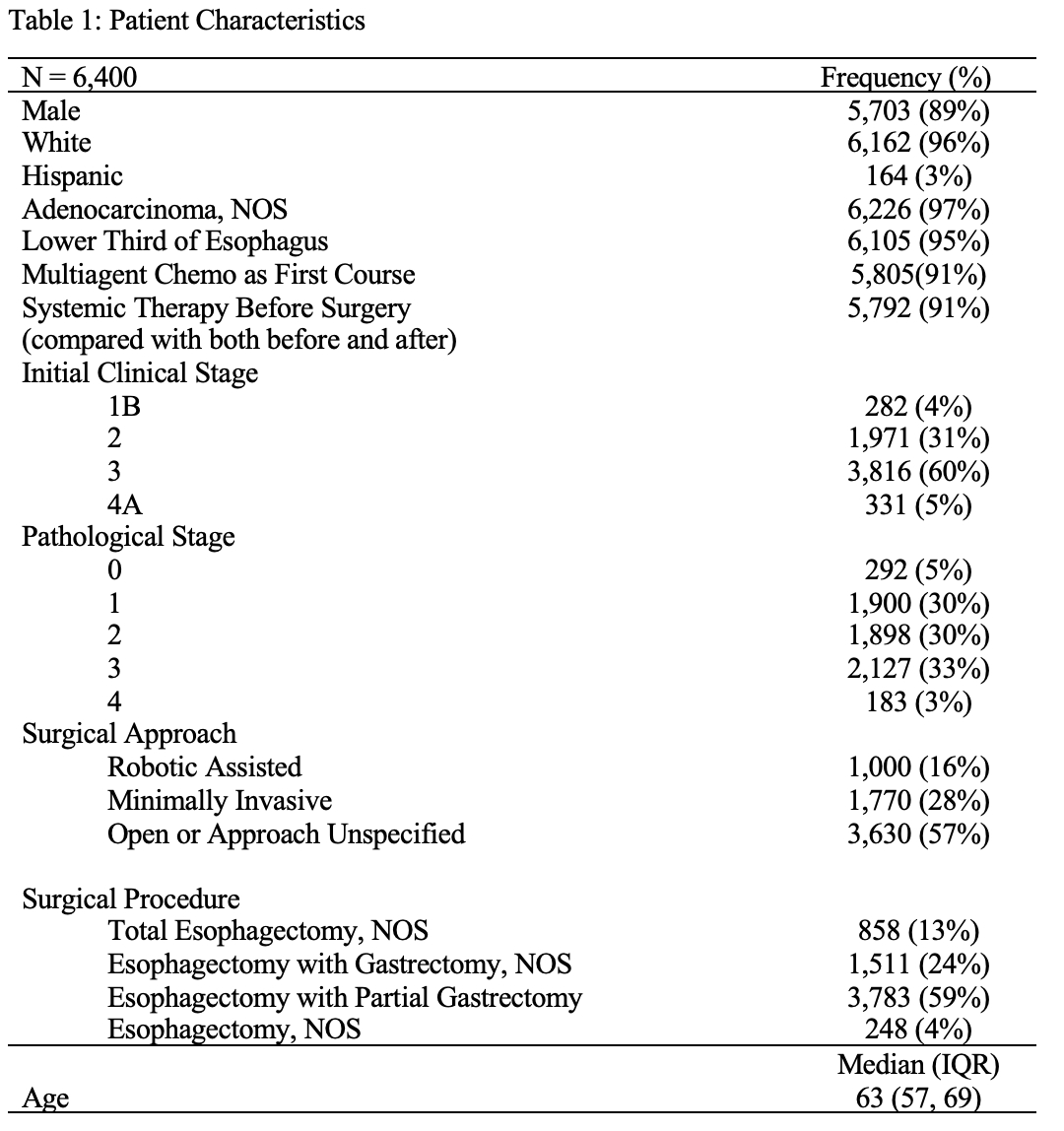
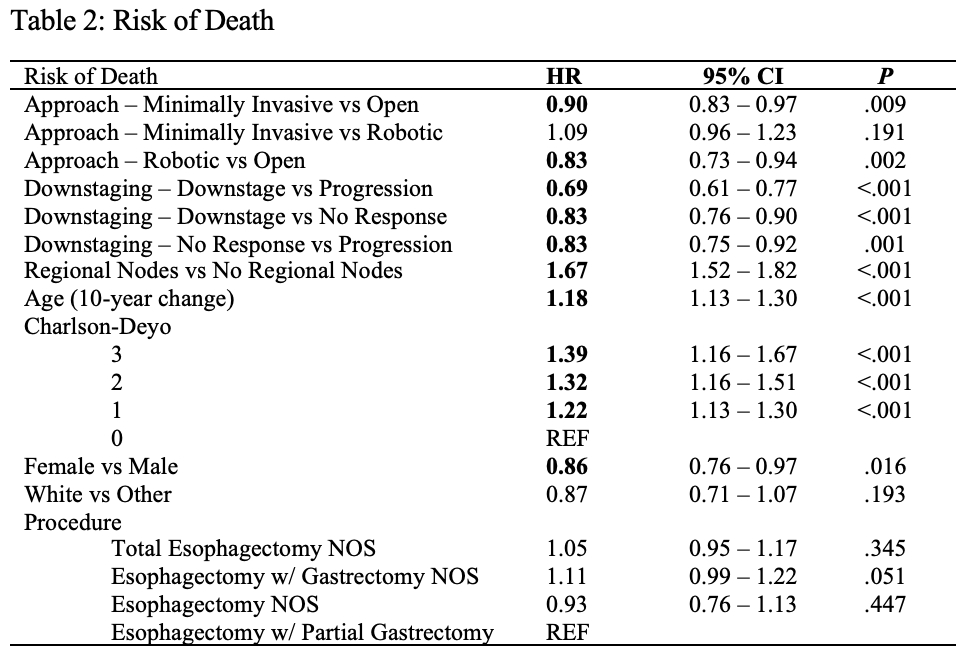
MethodUsing the 2010-2020 NCDB, we identified 6,400 patients with clinical stage 1B to 4A EAC who received NCRT and underwent esophagectomy. Multivariable marginal Cox proportional hazard models were estimated to evaluate risk of death by whether NCRT resulted in pathological downstaging and surgical approach after adjusting for age at diagnosis, biological sex, race, presence of reginal lymph nodes, Charlson-Deyo score, and procedure type. Additionally, two-way interactions between clinical stage and each covariate were estimated to evaluate whether the effect of each covariate was statistically similar across stages.
ResultsOur patient sample primarily consisted of older white males with a clinical stage 2 or 3 EAC (Table 1). Pathological downstaging and surgical approach were both associated with adjusted risk of death (Table 2); no statistically significant two-way interactions were observed between clinical stage and any covariate indicating that HRs reported below apply to all stages. Pathological downstaging following NCRT resulted in 31% lower risk of death compared to progression (HR: 0.69, 95% CI: 0.60-0.77, p < .001). Additionally, 17% lower risk of death was observed for both downstaging compared to no response (HR: 0.83, 95% CI: 0.76-0.90, p < .001) and for no response compared to progression (HR: 0.83, 95% CI: 0.75-0.92, p < .001). Regarding surgical approach, when compared with OE, RAMIE was associated with 17% lower adjusted risk of death (HR: 0.83, 95% CI: 0.73-0.94, p = .002) and MIE was associated with a 10% decrease in adjusted risk of death (HR: 0.90, 95% CI: 0.83-0.97, p = .009).
Conclusions/CommentsIn esophageal adenocarcinoma patients who underwent neoadjuvant chemoradiation, pathological downstaging was associated with lower mortality risk when compared to both patients who did not respond and patients who progressed. RAMIE and MIE were associated with lower risk of death compared to OE, with no statistically significant difference in mortality between RAMIE and MIE. While more long-term investigation is needed to fully understand these treatment effects, NACT followed by RAMIE or MIE demonstrates promising oncologic results for these patients.
Back to 2024 Abstracts