Back to 2024 Abstracts
DOES LAPAROSCOPIC PULL-DOWN HELLER MYOTOMY FOR ACHALASIA WITH MEGAESOPHAGUS IS AN IDEAL TREATMENT STRATEGY?
Andric Perez-Ortiz
*2, Janette Furuzawa-Carballeda
1, Ana M. Villa-González
1, Dulce P. Méndez-Hernández
1, Luis O. González-Alcocer
1, Luis G. López-Mosqueda
1, Carlos D. Romero-Osorio
1, Enrique Coss-Adame
1, Miguel A. Valdovinos
1, Gonzalo Torres-Villalobos
11Surgery, Instituto Nacional de Ciencias Médicas y Nutrición Salvador Zubirán, Mexico, Distrito Federal, Mexico; 2Centro Medico ABC, Mexico City, Mexico City, Mexico
Background: Megaesophagus is the end-stage of achalasia, and its surgical management is still controversial. In recent meta-analyses, esophagectomy was effective for patients with failed endoscopic dilations. However, this approach may be too aggressive and pose an increased risk for severe postoperative complications and mortality.
Aim: To describe the long-term outcomes of achalasia cases that underwent Laparoscopic Pull-Down Heller myotomy (PD-LHM) instead of esophagectomy.
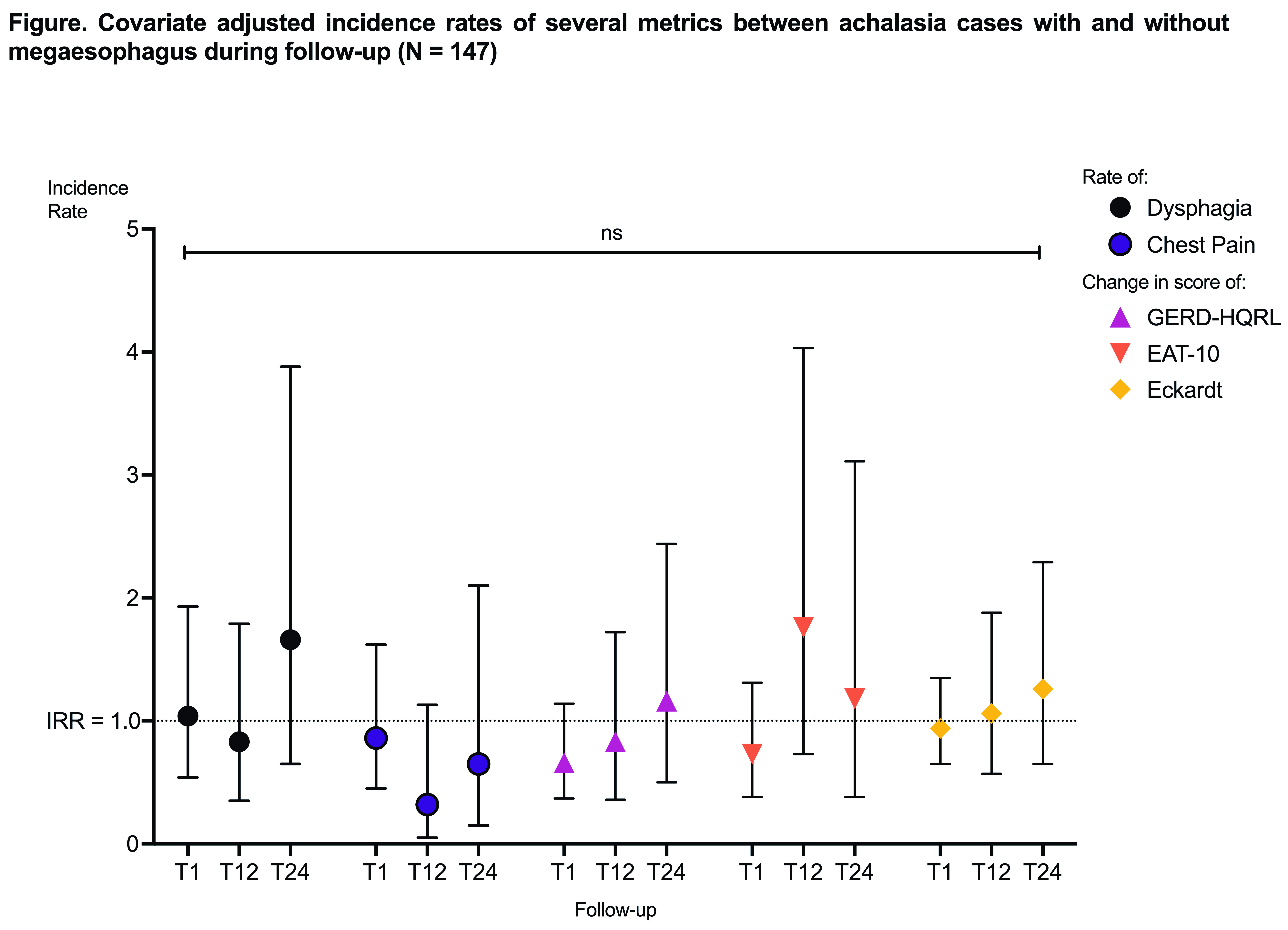
Methods: We conducted a 2:1 case-control study nested in a cohort of 49 achalasia patients with megaesophagus and 98 achalasia controls stratified by sex and achalasia subtype. All patients had confirmed achalasia diagnosis by esophagogram, upper endoscopy, and high-resolution manometry and were treated with PD-LHM. Megaesophagus cases had at least one imaging study with >6 cm of esophageal dilation. We followed up on symptom questionnaires and the incidence of dysphagia and chest pain during the immediate postoperative period at one-, six-, 12-, 24-, and 48 months after LHM. We compared both groups at baseline with chi-square and Student's t-test and the change in incidence of all metrics during follow-up with Poisson or Quasi-Poisson regression models based on data dispersion in SAS v.9.4 and R v.4.2.2.
Results: The 49 cases with megaesophagus were more likely to be male and diagnosed with type I or II achalasia than controls. Preoperatively, there were no differences in symptom questionnaires. However, cases had a lengthened (Mean difference 2.34 cm ± 0.93, P = 0.0168) and tortuous esophagus compared to controls. Post PD-LHM, there were no differences in esophageal angulation and complications. In the long-postoperative period, the adjusted incidence rate of symptoms and their control did not differ between groups (Figure). There were no reinterventions in both groups.
Conclusions: Our data indicates that PD-LHM might be a superior, safer, and more efficacious surgical approach for megaesophagus compared to esophagectomy. Surgical recurrence was null in the long postoperative period, and symptom control was similar to achalasia. Data replication in other cohorts could strengthen our recommendation for LHM in megaesophagus cases.
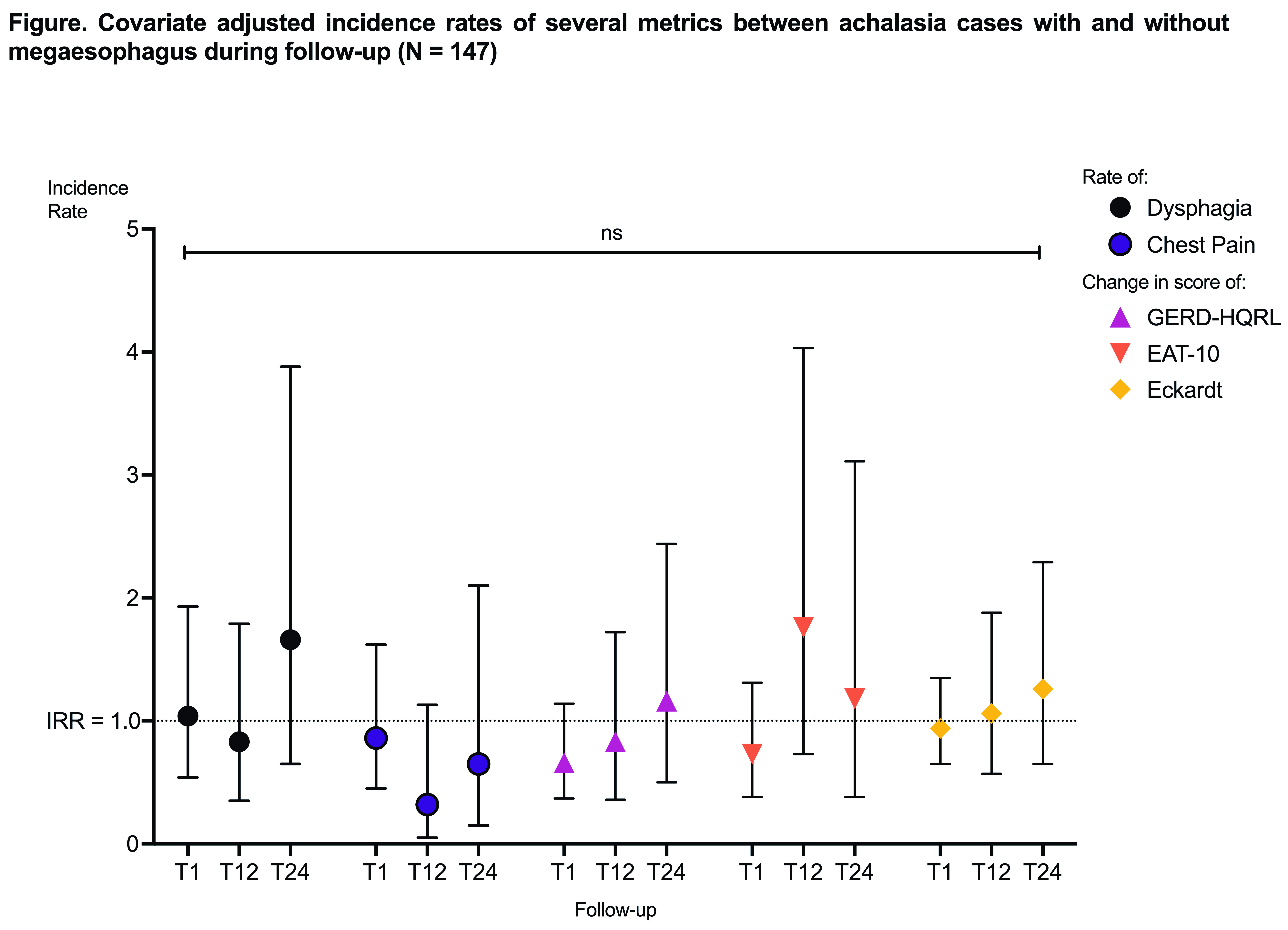
Figure. Covariate adjusted incidence rates of several metrics between achalasia cases with and without megaesophagus during follow-up (N = 147).
Back to 2024 Abstracts