Back to 2024 Abstracts
LAPAROSCOPIC FUNDOPLICATION IMPROVES ESOPHAGEAL MOTILITY IN PATIENTS WITH GERD - A HIGH-VOLUME SINGLE CENTER CONTROLLED STUDY IN THE ERA OF HIGH-RESOLUTION MANOMETRY AND 24-HOUR PH-IMPEDANCE
Arianna Vittori
*, Matteo Santangelo, Giovanni Capovilla, Luca Provenzano, Loredana Nicoletti, Andrea Costantini, Francesca Forattini, Matteo Pittacolo, Lucia Moletta, Michele Valmasoni, Edoardo V. Savarino, Renato Salvador
Universita degli Studi di Padova, Padova, Veneto, Italy
Background: Pathophysiology of GERD is complex and esophageal motility disorders are frequently contributing to the disease. Most of the existing literature demonstrates that Laparoscopic Fundoplication (LF) is safe in the setting of ineffective or weak peristalsis, however the effect of the wrap on esophageal motility is still debated. This study aimed to assess how a functioning and effective fundoplication could impact the esophageal motility in patients with GERD.
Methods: We analyzed prospectively collected data on patients who underwent laparoscopic Nissen (LN) or Toupet (LT) fundoplication for GERD at our Department between 2010 and 2022. We selected patients who have been treated with LF according to the GERD international guidelines. The exclusion criteria were: patients assessed with conventional manometry before and/or after surgery; patients who had previously been treated surgically or endoscopically for GERD; patients with a giant hiatal hernia (type II, III and IV) prior to surgery; patients with connective tissue disease, diabetes or other pathological conditions known to affect esophageal peristalsis (e.g., eosinophilic esophagitis); patients with a proof of a too-tight LF.
Demographic and clinical characteristics were recorded. Patients were evaluated with the GerdQ questionnaire, barium swallow, endoscopy and HRM and 24-hour pH-Impedance (pH-MII) before and after surgery.
The HRM were reviewed by 2 experts, following the criteria of the Chicago Classification v4.0. LF failure was recorded in case of an abnormal postoperative pH-MII using the Lyon 2.0 criteria.
Results: During the study period, among the 525 patients who underwent LF, 124 (M:F=89:35) were recruited. Fifty-eight patients underwent LN and 66 patients underwent LT. All procedures were completed laparoscopically and the 90-day postoperative mortality was nil.
At the postoperative pH-MII, we recorded a good outcome in 103 patients and a failure in 21 patients.
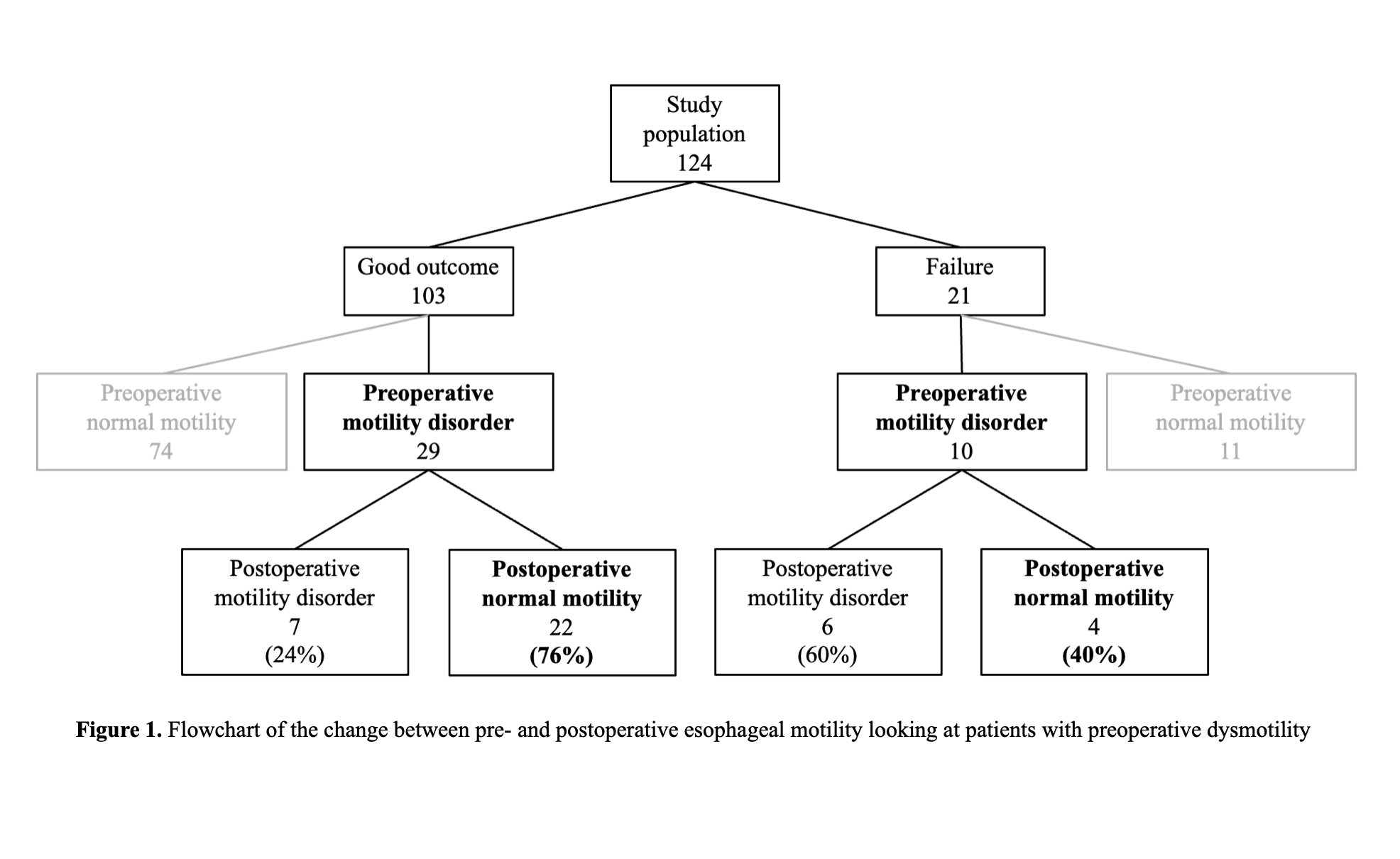
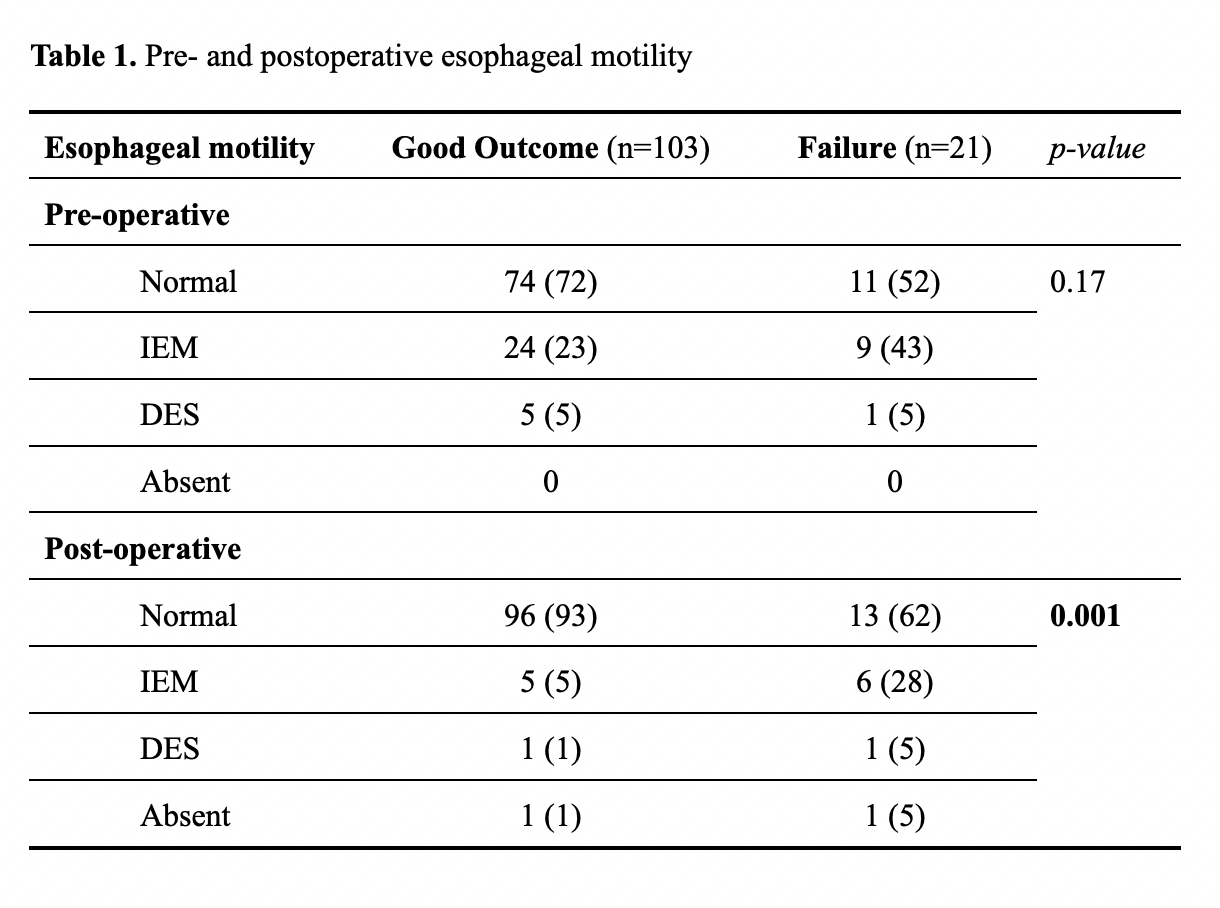
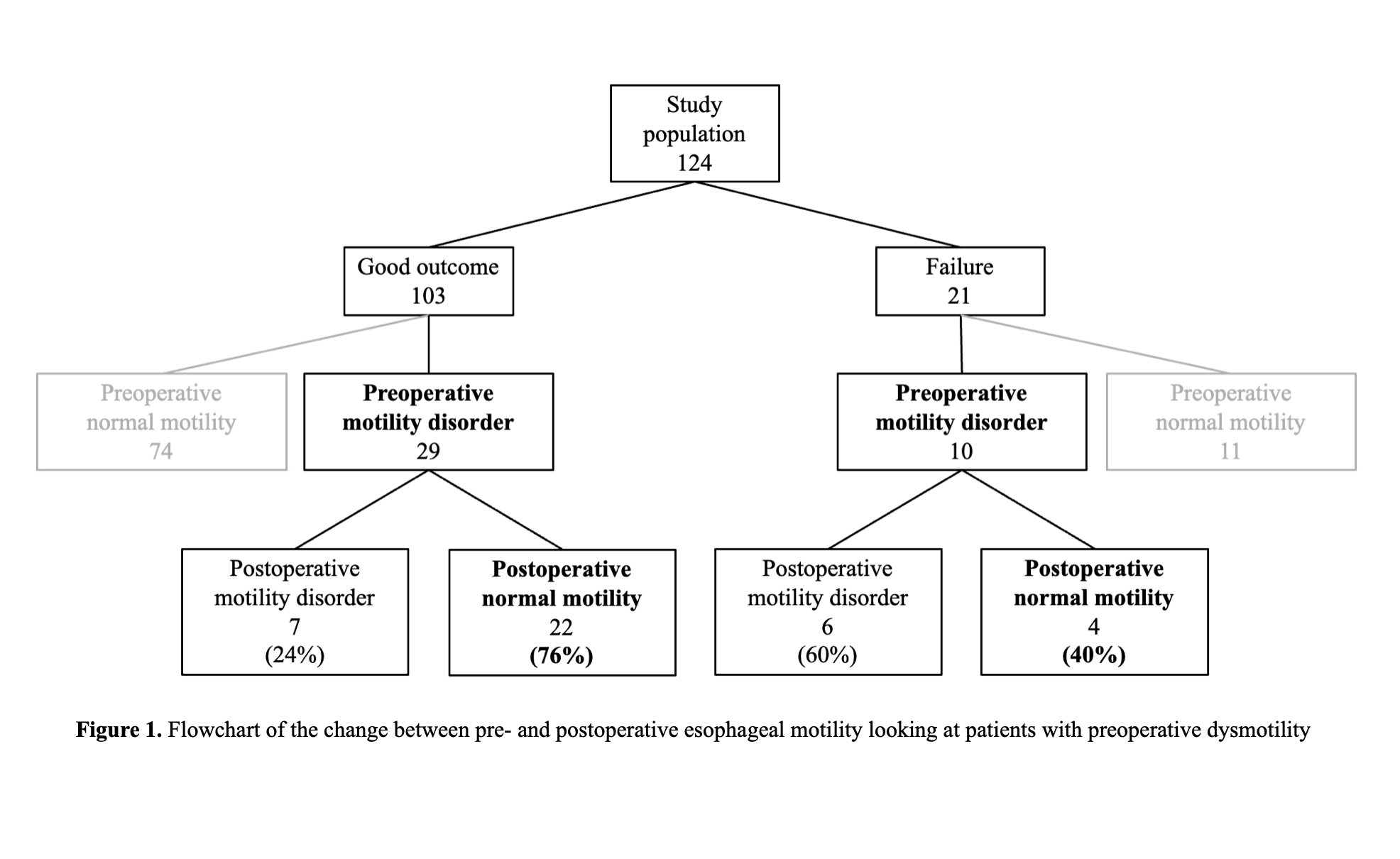
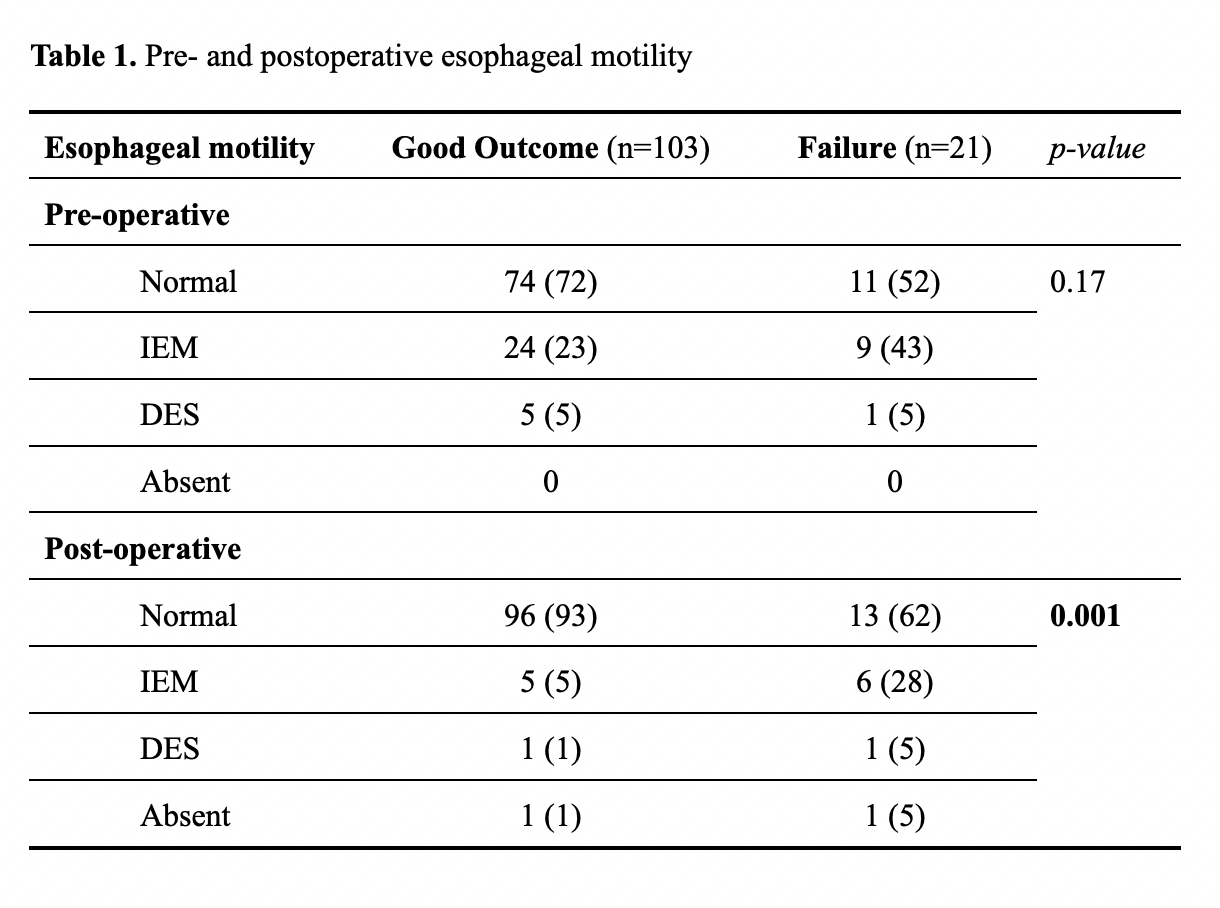
The pre- and postoperative manometric patterns are described in Table 1. A shown in Figure 1, of the 103 patients with an effective fundoplication, 29 presented a preoperative motility disorder (24 patients had a IEM and 5 a DES), and postoperatively 22 (76%) of these patients had a normalization of the esophageal motility. Ten of the patients with a failed fundoplication had a preoperative motility disorder (9 had a IEM and one a DES); 4 (40%) of them showed normal motility after LF. There was a significant association between a successful LF and the normalization of esophageal motility (p<0.05).
Conclusion: This study demonstrated that LF is an effective and functioning treatment in patients with GERD associated with an esophageal motility disorder. Moreover, our results indicate that LF could determine a normalization of the disordered esophageal motor function in patients with GERD.
Back to 2024 Abstracts