Back to 2024 Abstracts
ASSOCIATION BETWEEN BASELINE HEMOGLOBIN A1C AND 30-DAY OUTCOMES AFTER SLEEVE GASTRECTOMY AND ROUX-EN-Y GASTRIC BYPASS
Safraz Hamid
*1,2, Elena Graetz
1, Eric B. Schneider
1, Karen E. Gibbs
11Yale School of Medicine, New Haven, CT; 2National Clinician Scholars Program at Yale University, New Haven, CT
Background: Metabolic and bariatric surgery (MBS) is a well-established treatment option in the management of obesity and its complications. At times, surgeons may delay MBS if the preoperative hemoglobin A1c (HbA1c) is elevated above a specified cutoff value. It remains unclear if there is a HbA1c value above which MBS is prohibitive or should be delayed.
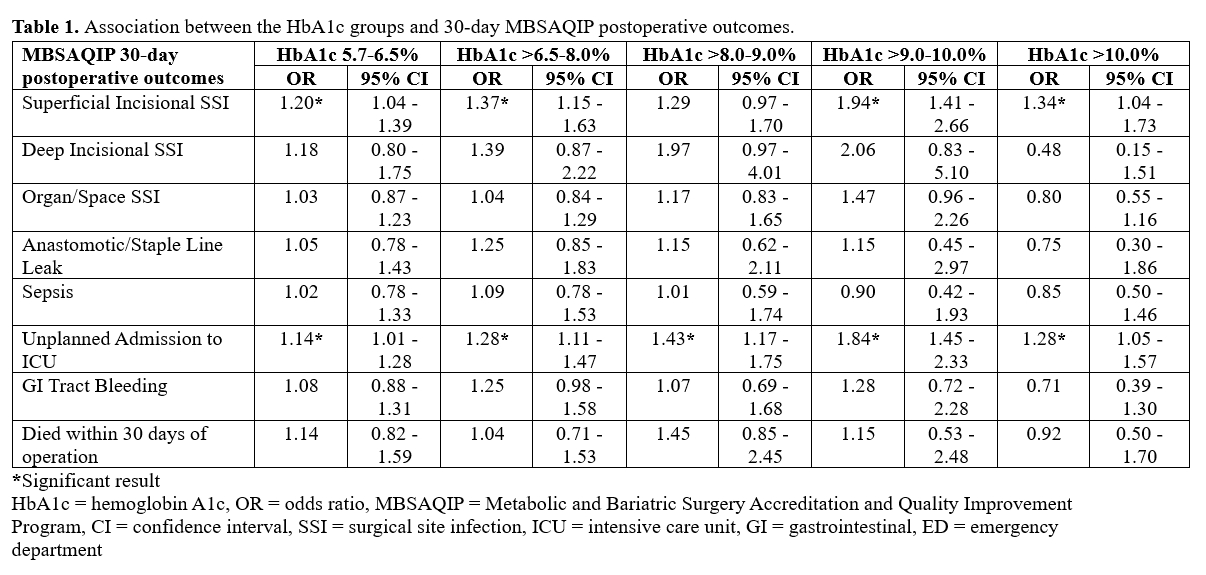
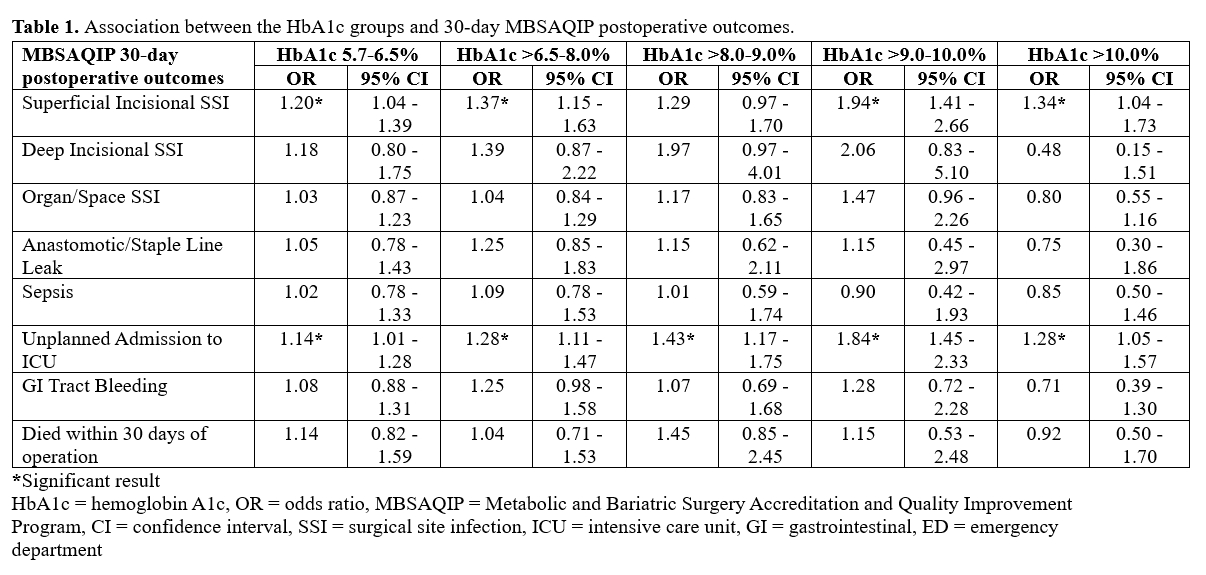
Methods: We identified patients who underwent primary sleeve gastrectomy (SG) or Roux-en-Y gastric bypass (RYGB) from 2017 to 2021 in the Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program (MBSAQIP) database who had preoperative HbA1c data recorded. Using patients with HbA1c <5.7% as a reference group, we used logistic regression models to test the association between five HbA1c groups (5.7-6.5%, >6.5-8%, >8-9%, >9-10%, and >10%) and various 30-day postoperative outcomes available in the MBSAQIP. We covaried for age, sex, race, BMI, procedure type, functional status, ASA class, operation length, insulin-dependence, steroid use, and smoking status.
Results: A total of 802,205 patients underwent primary SG or RYGB from 2017 to 2021. Preoperative HbA1c data was missing for 56.79% of these patients. Our final sample size, therefore, included 346,613 patients. The mean age of the sample was 44.2 years (SD=12). 62.8% of patients were White, 20.2% were Black, and 15.8% were Hispanic. The proportion of patients that were insulin-dependent significantly increased with increasing HbA1c values up until the >10% group which had a lower proportion of insulin-dependent patients compared to the 6.5-8%, 8-9%, and 9-10% groups (p<0.001). All HbA1c groups except the >8-9% group were associated with more superficial incisional surgical site infections (SSIs). All comparative elevated HbA1c groups were associated with more unplanned ICU admissions. There were no significant associations between any of the HbA1c groups and anastomotic/staple line leaks, organ space or deep incisional SSIs, sepsis, GI tract bleeding, and 30-day mortality. Unexpectedly, the >10% group had the fewest adverse postoperative events while the >9-10% group had the most.
Conclusions: Among SG and RYGB patients, odds of anastomotic leaks, deep incisional SSI, sepsis, and mortality were not increased in patients with elevated HbA1c values. A trend toward a positive dose response relationship between HbA1c levels and the incidence of superficial incisional SSI and unplanned ICU admissions was observed; however, it is possible that patient HbA1c levels may have influenced preoperative decision making, which might bias the findings of this study.
Back to 2024 Abstracts