Back to 2024 Abstracts
ENDOSCOPIC SUBMUCOSAL DISSECTION VS APC FOR TISSUE PREPARATION IN GASTRO-GASTRIC FISTULA CLOSURE DEMONSTRATES IMPROVED PATIENT OUTCOMES
Thomas J. Mathews
*2, Pichamol Jirapinyo
1, Christopher C. Thompson
11Division of Gastroenterology, Hepatology and Endoscopy, Brigham and Women's Hospital, Boston, MA; 2University of Missouri-Kansas City, Kansas City, MO
Introduction:
Roux-en-Y Gastric Bypass (RYGB) is a well-known safe and effective surgical option for weight loss in patients with obesity. However, RYGB has many complications, including gastro-gastric fistula (GGF) formation. Although rare, GGF has many serious implications, including weight regain, ulcer formation, and other GI side effects. We aim to compare endoscopic techniques for GGF closure, specifically suture with endoscopic submucosal dissection (ESD) versus Argon Plasma Coagulation (APC), and its impact on patient outcomes.
Methods:
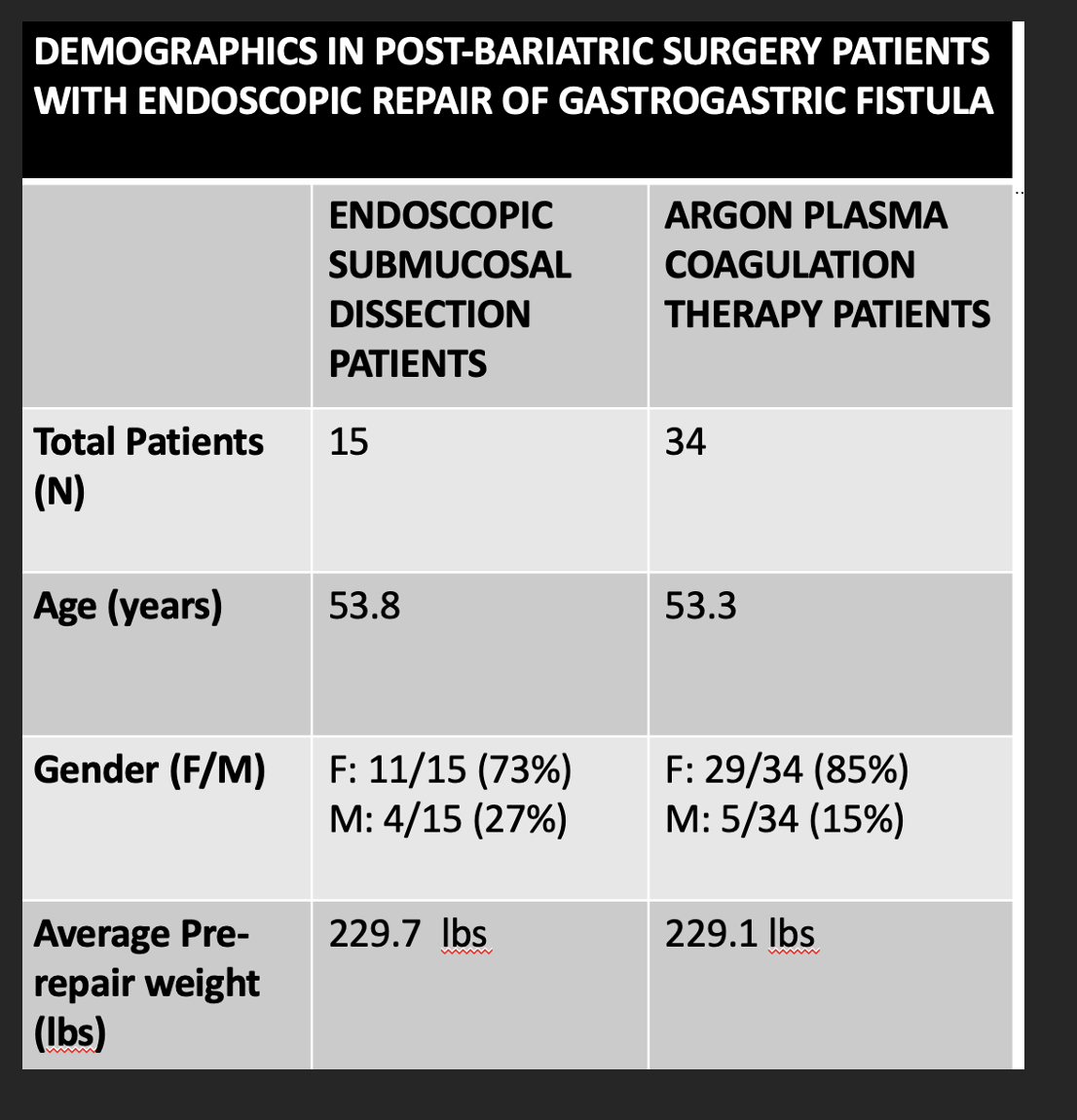
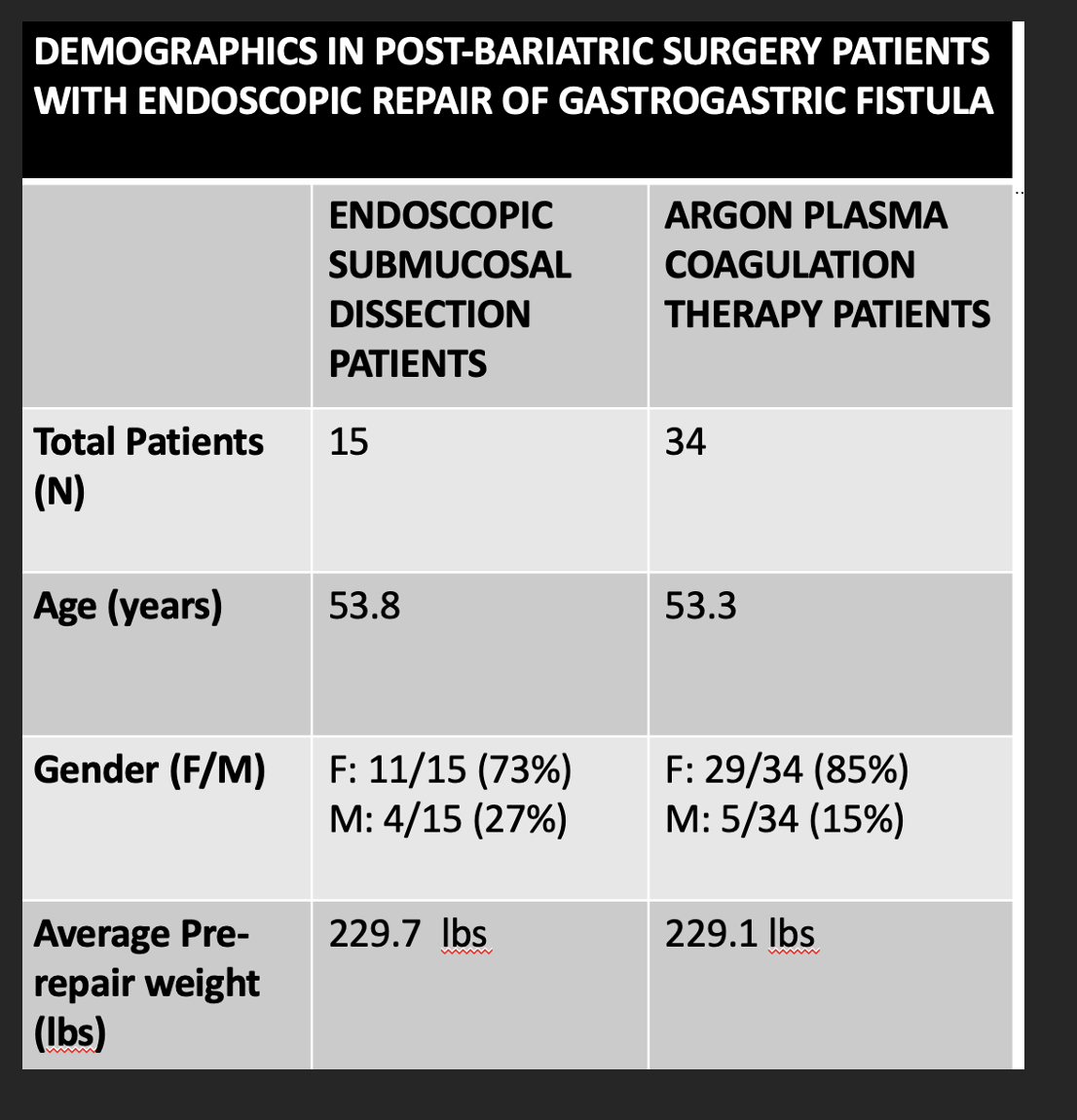
In this retrospective single-tertiary center, data was collected prospectively, which included all patients who underwent RYGB and later developed GGF. Of these patients, those who underwent endoscopic repair with overstitch technique and either ESD or APC between November 2010 and April 2023 were included. Patients who underwent outlet revision at time of repair were excluded. 2 patients were also excluded for undergoing EMR repair. Endoscopy (EGD)and upper GI series (UGIS) were reviewed and recorded. Successful fistula closure was defined as having no visual evidence of re-fistularization (by EGD or UGIS) within one year of intervention. Symptoms before and after repair was recorded. Chi-square analysis was performed.
Results:
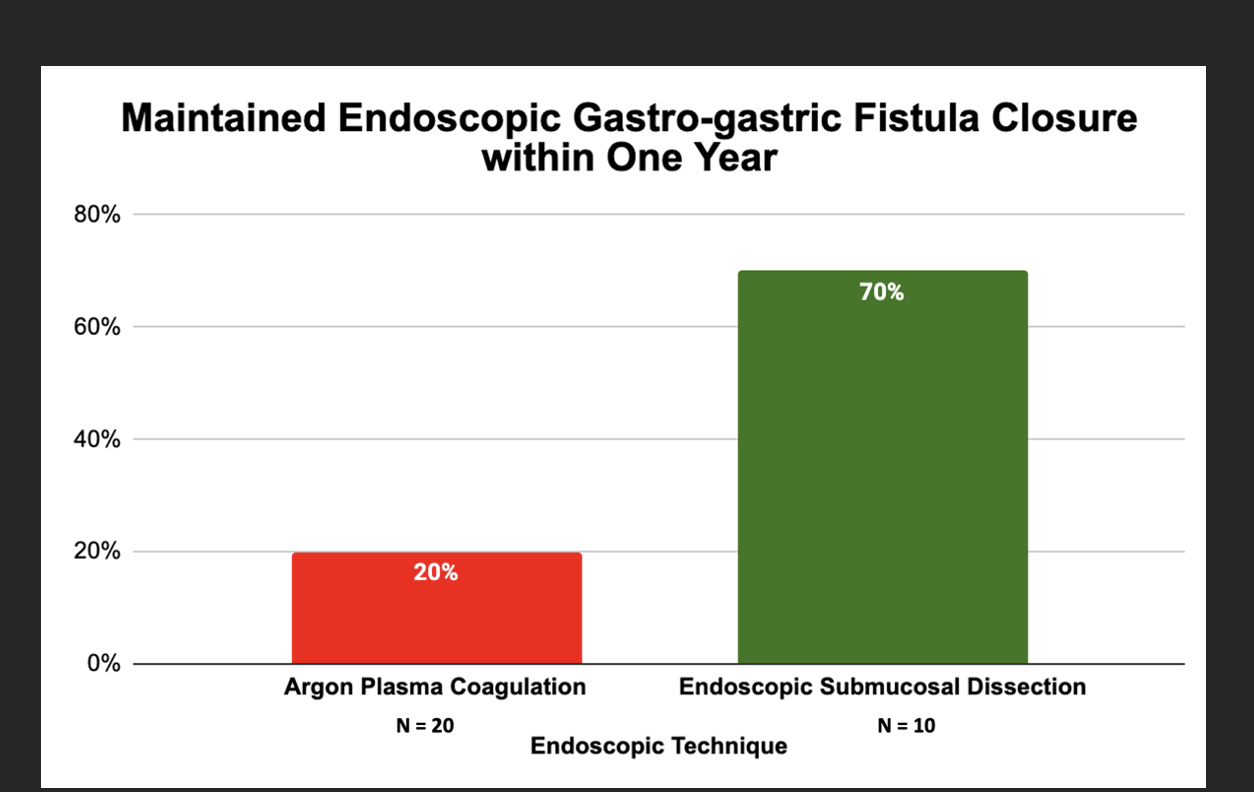
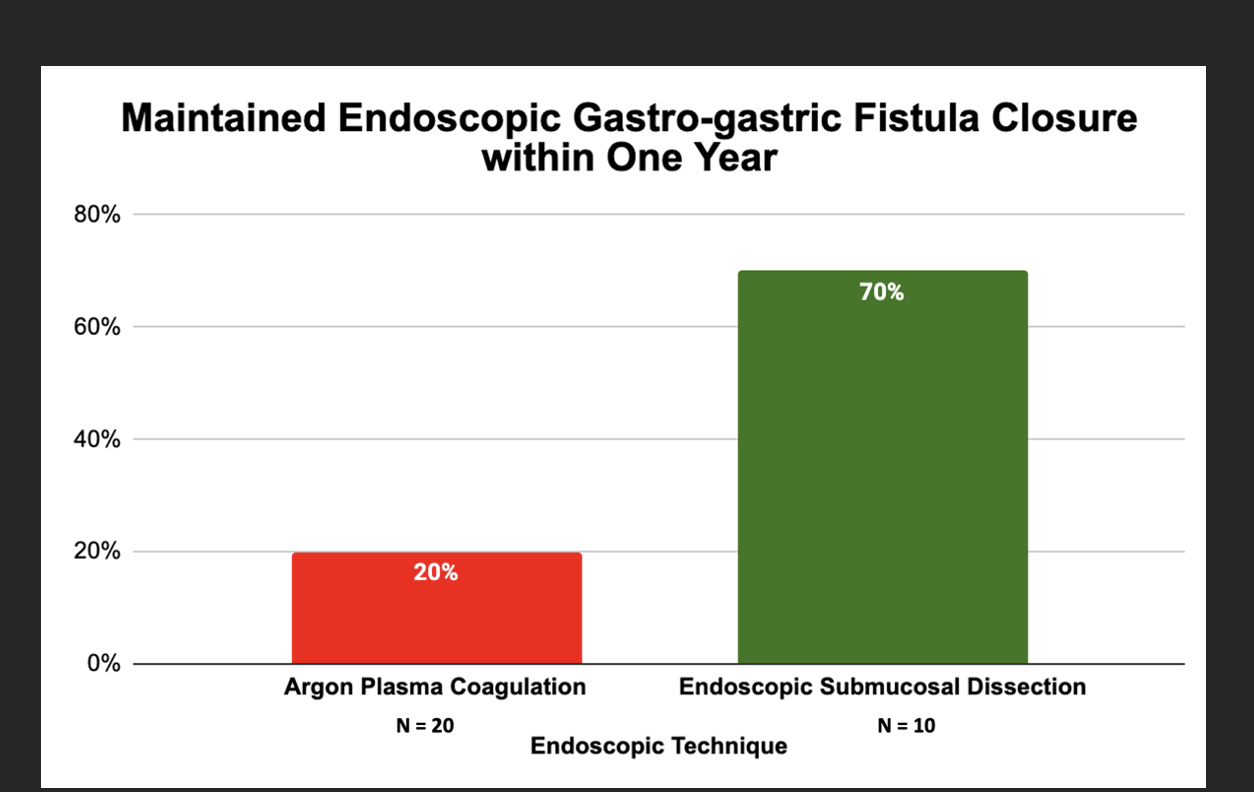
A total of 49 patients underwent ESD or APC for GGF repair. 34 patients underwent APC therapy while 15 patients underwent ESD. In the APC population, 20 patients had at least one imaging study (UGIS or EGD) within one year. 20% (4/20) of these patients had evidence of successful closure of fistula. In contrast, 70% (7/10) of ESD patients showed continued success of fistula closure without a failed study within a year. ESD patients had a significantly increased rate of closure (p=0.01) without failure compared to APC patients within one year.
Regarding symptomatic management, 42% (5/12) of APC patients recorded overall improvement. On the other hand, 90% (9/10) of ESD patients reported symptomatic improvement within one year. Patients who underwent ESD have a significant improvement in symptoms (p = 0.03) compared to those with APC within one year.
Conclusion:
This study demonstrates that ESD is more effective than APC for tissue preparation prior to endoscopic suturing in the treatment of chronic gastro-gastric fistula. Suturing with ESD also significantly improved related symptoms compared to APC.
Back to 2024 Abstracts