Back to 2024 Abstracts
REAL-WORLD WEIGHT LOSS OUTCOMES OF SEMAGLUTIDE: COMPARATIVE ANALYSIS AMONG PATIENTS WITH AND WITHOUT METABOLIC/BARIATRIC SURGERY
Pourya Medhati
*1, Ali Tavakkoli
21Brigham and Women's Hospital, Boston, MA; 2Brigham and Women's Hospital, Boston, MA
Background: Introduction of Nutrient Stimulated Hormone-based agents such as semaglutide, a glucagon-like peptide-1 receptor agonist (GLP-1), have revolutionized weight management strategies given their excellent weight loss outcomes in trials settings. There are, however, several real-world challenges with the use of these medications including cost, medication shortage, side effects, and others. The weight loss outcomes of these medications in those with a past history of Metabolic/Bariatric Surgery (MBS) are not well known. In this study, we aimed to discover weight loss outcomes of semaglutide in real-world practice among surgical and non-surgical patients.
Methods: We conducted a retrospective cohort study of patients who were prescribed semaglutide in our institutional weight management center between 2018 and 2023. The percentage total weight loss (%TWL) was analyzed for the overall cohort using our electronic health records, and a detailed chart review was performed on a 20% subgroup to assess for medication compliance. Those with or without a history of MBS were compared.
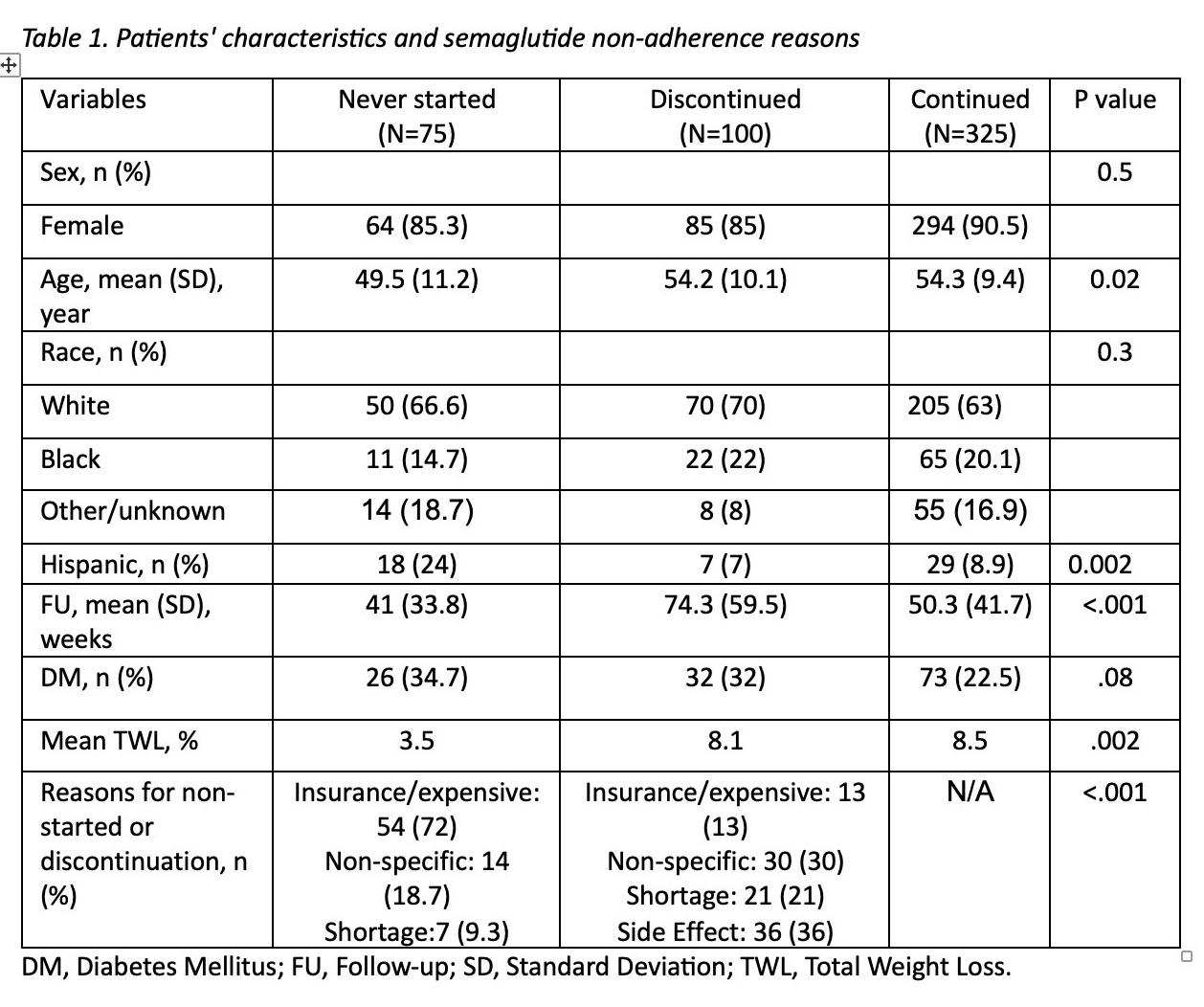
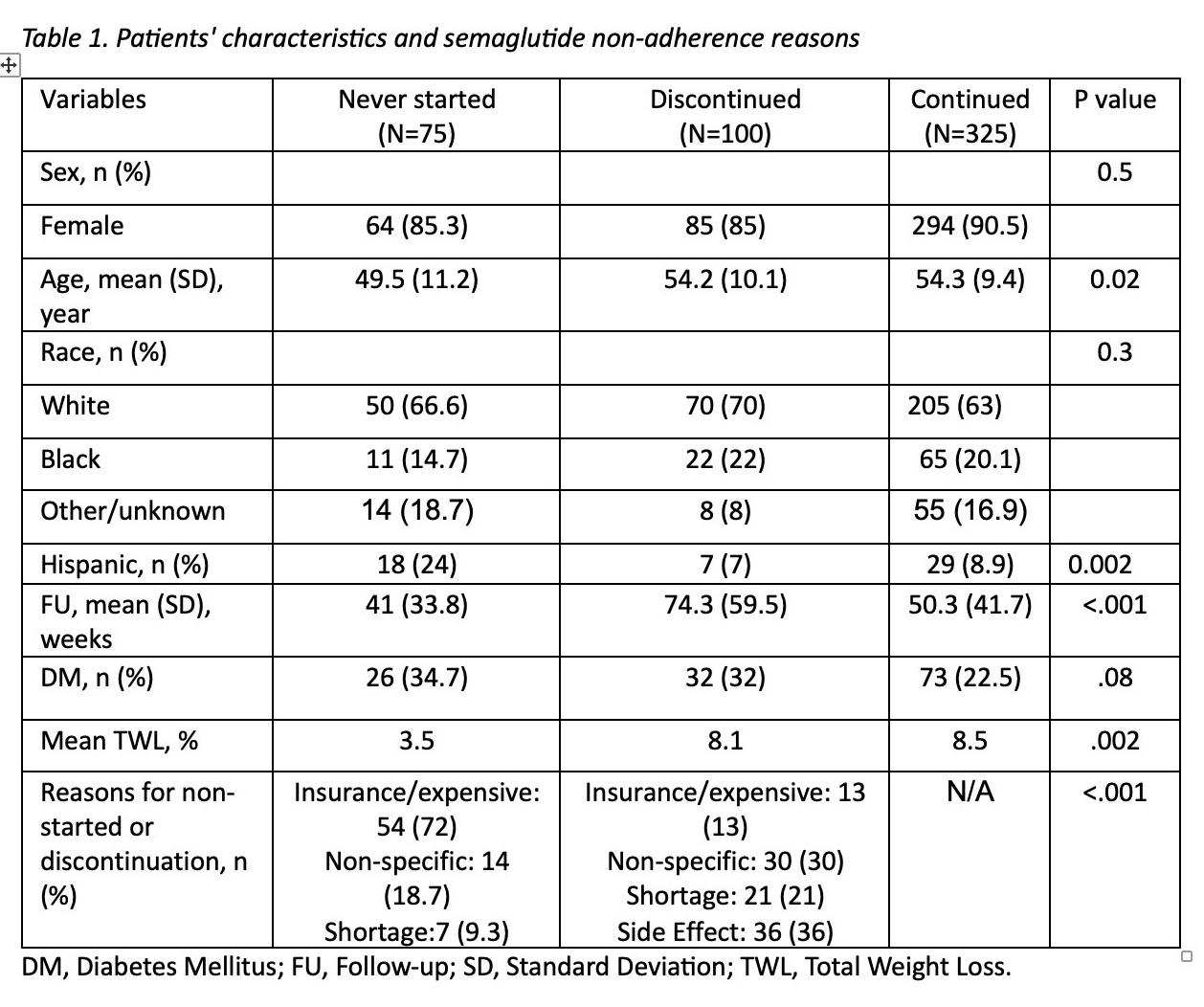
Results: Among 2,491 patients prescribed semaglutide (78% female, 73.5% white, and mean age 50.9±12.9 years), 330 (13.2%) had a history of MBS. In the overall cohort, TWL% was 6%. Individuals with and without MBS had a TWL% of 5.8% and 6% (p=.3), respectively, over a mean follow-up of 59.2 and 52.4 weeks (p=.02). Notably, within the non- MBS subgroup, females exhibited a higher weight reduction compared to males (6.4% vs. 4.8%, p<.001). Table 1 summarizes a cohort of 500 patients with a detailed chart review. Among them, 75 (15%) patients were not able to commence medication primarily due to lack of insurance. 100 (20%) patients had to discontinue the medication predominantly due to side effects. The remaining cases were consistently using the medication at the last follow-up visit attained an average %TWL of 8.5% over 50.3 weeks.
Conclusions: This study highlights the lack of insurance coverage as one of the most common burdens for patients to start semaglutide. Even in patients with a prior MBS history, semaglutide leads to meaningful weight loss similar to those without MBS history, although overall, these results are lower than those achieved in clinical trials.
Back to 2024 Abstracts