Back to 2024 Abstracts
COST-EFFECTIVENESS ANALYSIS OF BARIATRIC SURGERY AMONG INDIVIDUALS WITH OBESITY(BMI ≥ 35 KG/M2): A MATCHED COHORT STUDY
S. Julie-Ann Lloyd
*1, Elizabeth Wall-Wieler
2, Yuki Liu
2, Feibi Zheng
1,2, Teresa L. LaMasters
3,41Baylor College of Medicine, Houston, TX; 2Global Health Economics and Outcomes Research Inc, Sunnyvale, CA; 3University of Iowa Hospitals and Clinics, Iowa City, IA; 4UnityPoint Health, Des Moines, IA
Background: Obesity is a global health problem with alarming rates of morbidity and mortality. Despite this significant disease burden, obesity can be safely and effectively treated with bariatric surgery. However, only a small fraction of eligible patients undergoes surgical weight loss.
Objective: To assess the economic impact (total and by source healthcare costs) of bariatric surgery costs in the first 2 years after the index date, and to identify characteristics of individuals who had the largest post-index date cost differences.
Methods: Adults with obesity (BMI 35kg/m
2) were identified in US national employer-based retrospective claims database Merative™ (previously Truven/IBM Marketscan). Individuals who had a bariatric surgery were matched 1:1, based on age, BMI, sex, obesity-related comorbidities, and healthcare costs in the year before the index date, with non-surgical patients. Total costs and costs by clinical care type were compared in the two years after the index date using paired
t-tests.
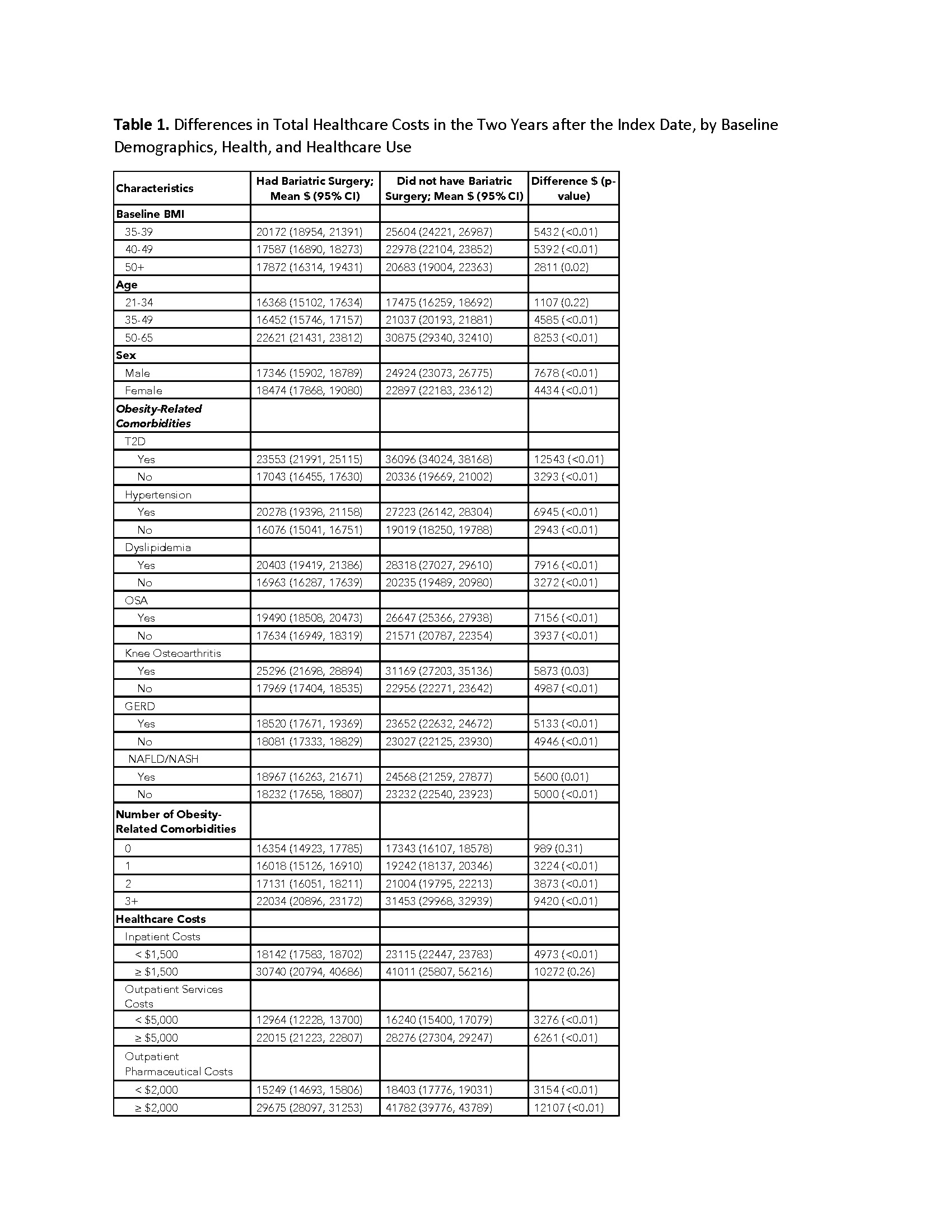
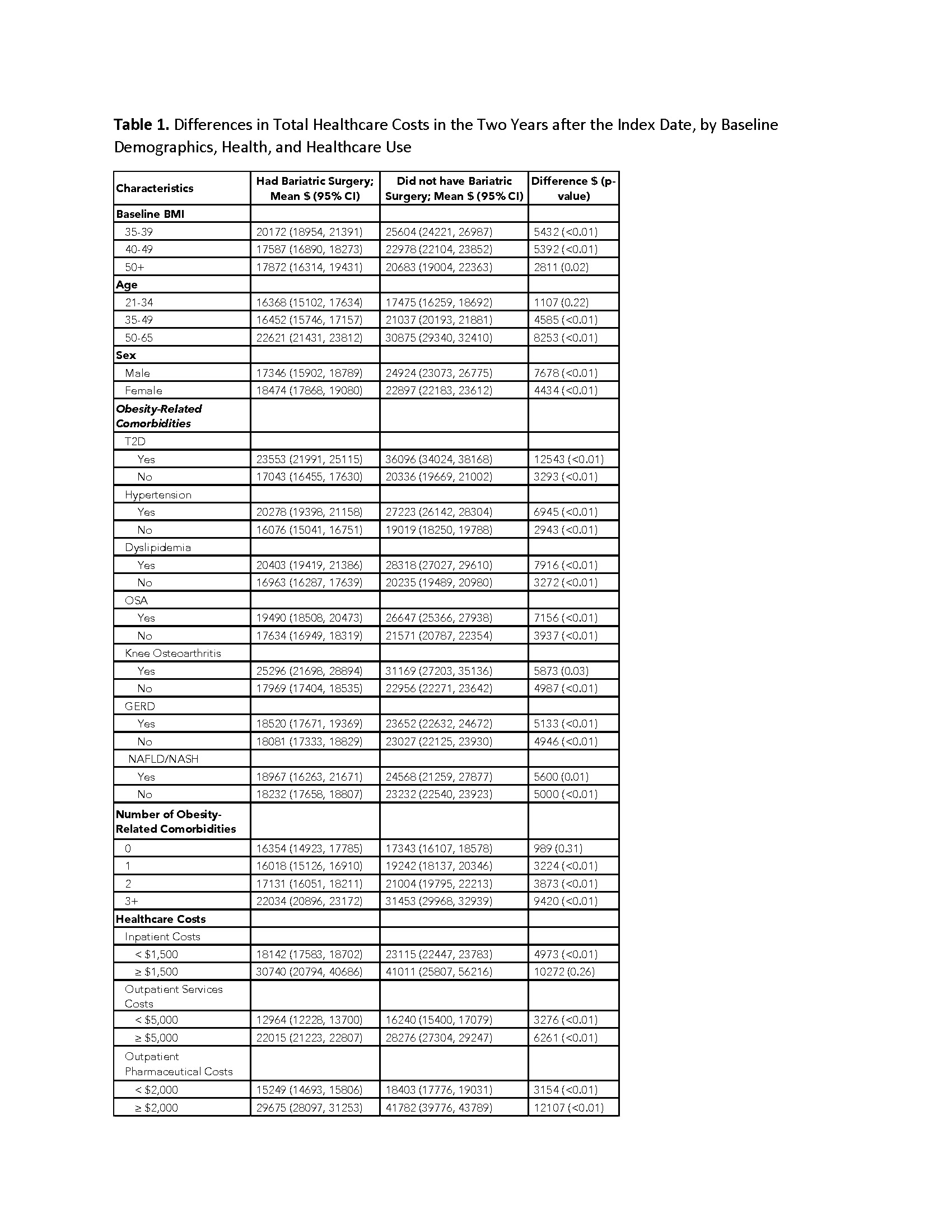
Results: After well-balanced matching, the study population included 9,436 patients who had bariatric surgery and 9,436 similar non-surgical patients. In the two years after the index date, total healthcare costs were $5,022 lower among individuals who had bariatric surgery (
p < 0.01). In 29 of 32 demographic, health, and healthcare characteristics examined, healthcare costs were significantly lower among individuals who had bariatric surgery. The largest post-index date cost differences (all lower among individuals who had bariatric surgery) were for individuals who had Type 2 diabetes at baseline ($12,543), high pharmaceutical costs at baseline ($12,107), and 3 or more obesity-related comorbidities at baseline ($9,420) (see Table 1).
Conclusions: Bariatric surgery is associated with a 27.5% reduction in healthcare costs in the first 2 years after the index date. Differences in post-index healthcare costs varied substantially by baseline demographics, presence of obesity related comorbidities, and pre-existing pharmaceutical spending.
Back to 2024 Abstracts