Back to 2024 Abstracts
OPEN-CAPSULE PROTON PUMP INHIBITOR IS ASSOCIATED WITH FEWER COMPLICATIONS OF MARGINAL ULCERATION AFTER ROUX-EN-Y GASTRIC BYPASS
Heesoo Yoo
*, Alvin Kwon, Alison Zhao, Varun Aitharaju, Kristelle J. Imperio-Lagabon, Stephen A. Firkins, Roma Patel, Bailey Flora, Roberto Simons-Linares
Gastroenterology, Cleveland Clinic, Cleveland, OH
Background: Marginal ulceration (MU) is a significant cause of morbidity after Roux-en-Y gastric bypass (RYGB). Proton pump inhibitor (PPI) therapy is the mainstay of treatment. Unfortunately, complications and recurrence of MU are common despite PPI compliance and frequently necessitate surgical or endoscopic intervention. There is a paucity of data describing the association between complications of MU and the use of “open-capsule� PPI (OC-PPI) compared to “intact-capsule� PPI (IC-PPI). This study aims to compare the rate of complications and recurrence of MU when treated with OC- vs. IC-PPI.
Methods: A retrospective study of patients with a history of RYGB diagnosed with MU on endoscopy from August 1
st, 2016 to April 3
rd, 2022 was conducted. MU recurrence and complications, including strictures, perforations, malnutrition, gastrointestinal bleeding (GIB) requiring transfusions and/or hospitalizations, were investigated. PPI type, dose, and formulation were recorded pre- and post-MU diagnosis. Recurrence of MU was recorded until the time of analysis in November 2023. The primary outcome was the rate of composite MU complications and recurrence rate. Logistic regression analysis was performed to assess the association of OC-PPI (vs. IC-PPI) with predefined key variables.
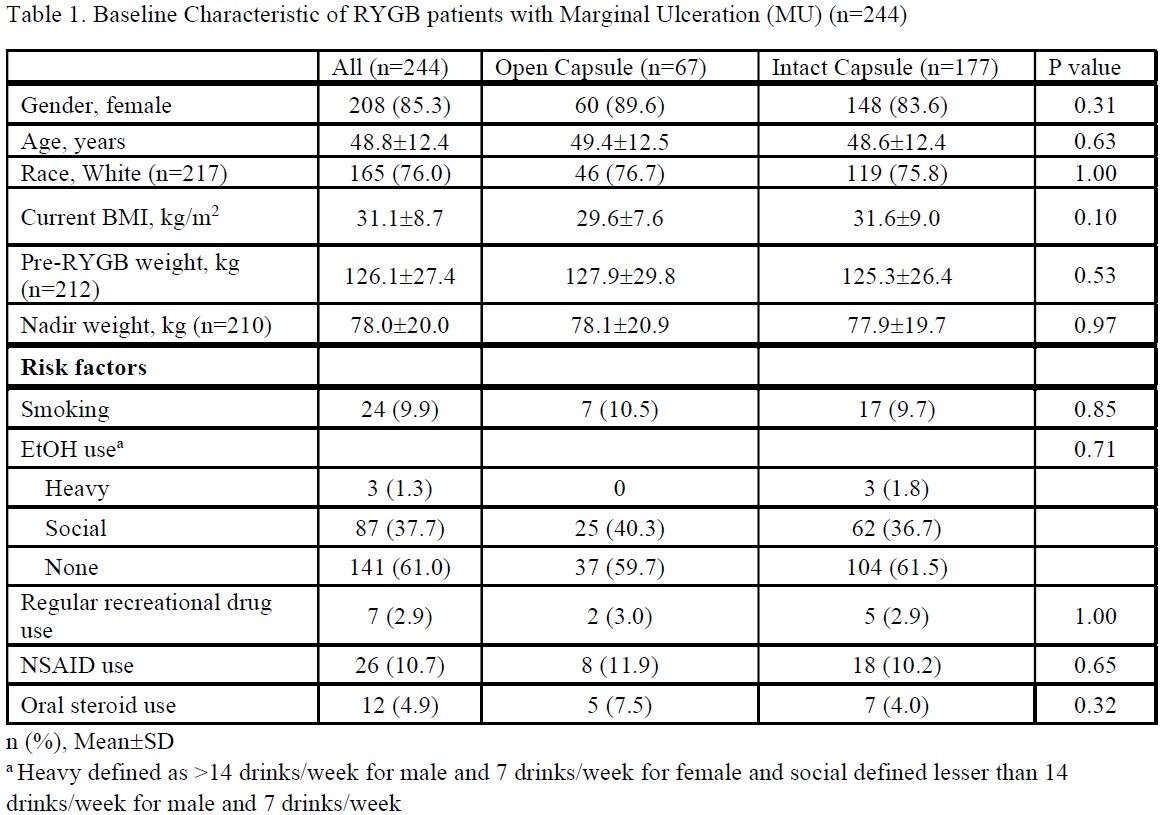
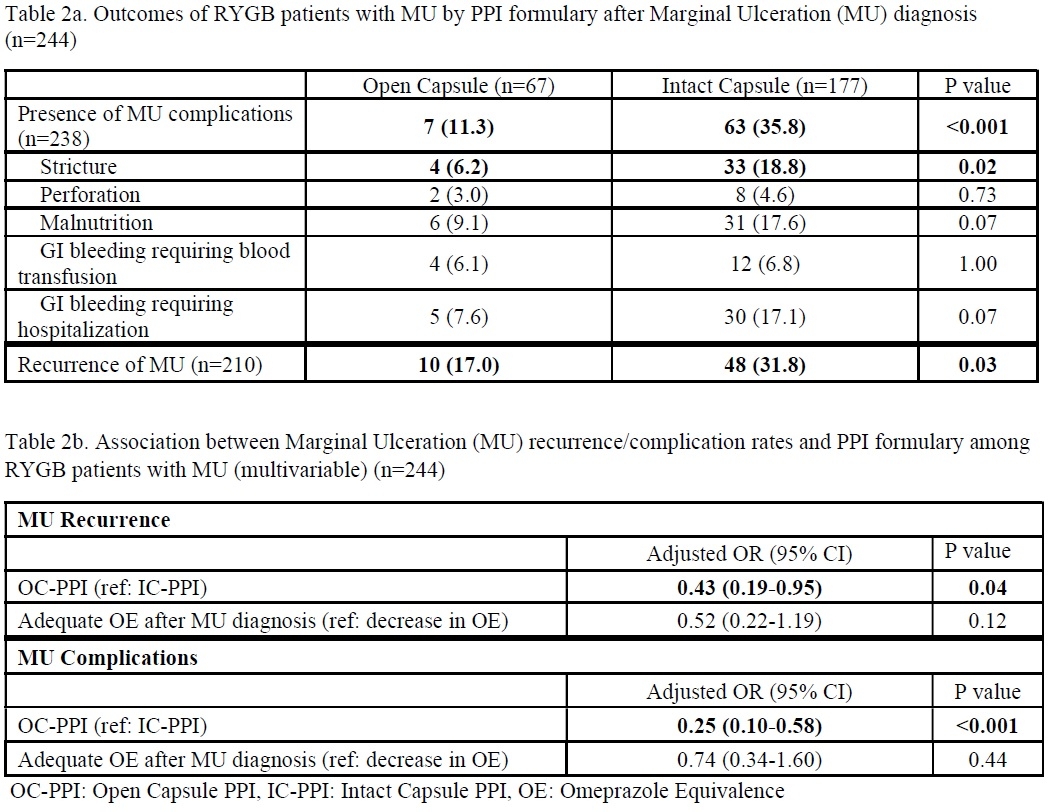
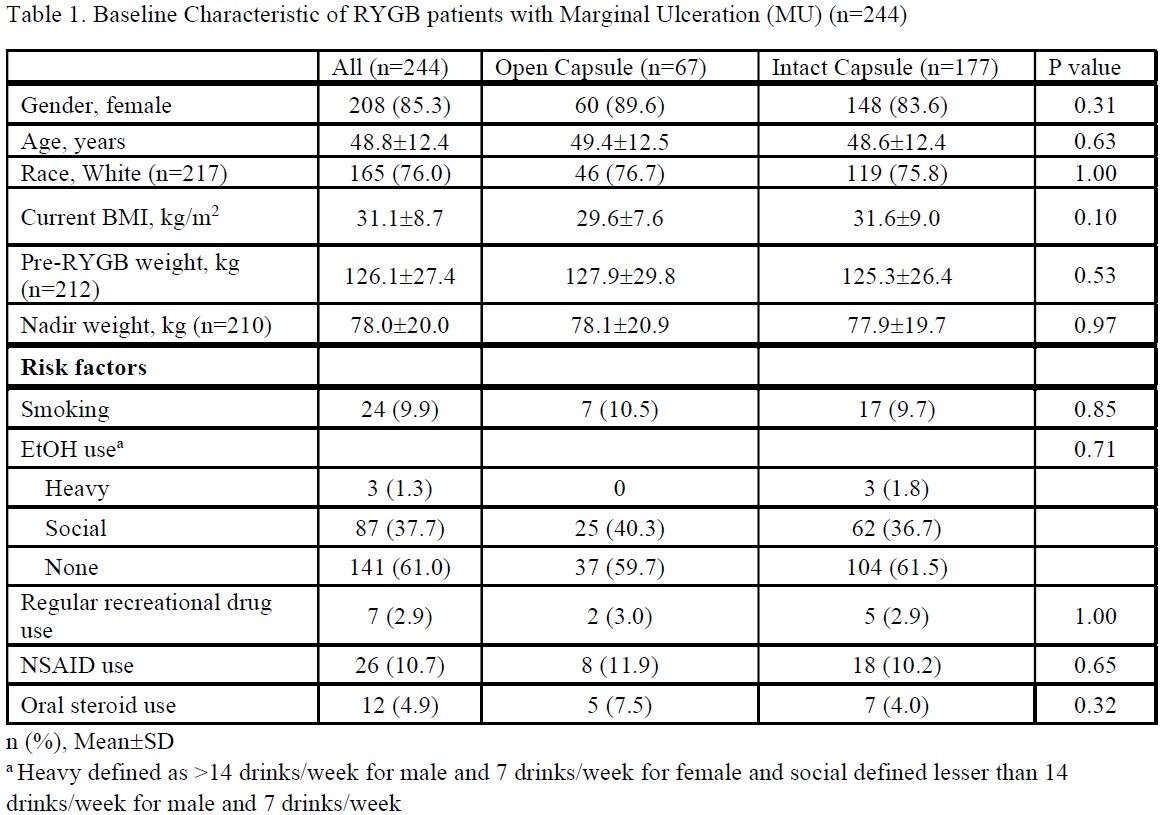
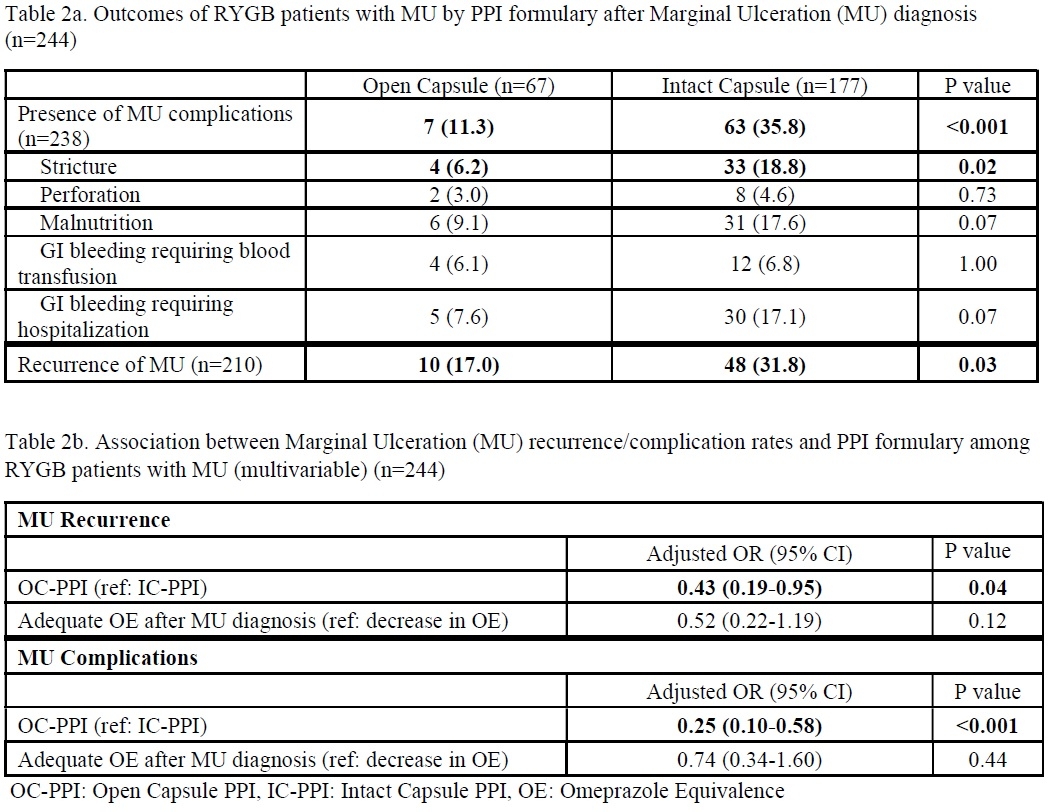
Results: A total of 355 RYGB patients with MU, 67 patients in the OC-PPI group, and 177 in the IC-PPI group were included. There was no difference in gender, age, race, current BMI, other known risk factors for MU, or the use of non-steroidal anti-inflammatories (NSAIDs) and/or steroids. 7 patients in OC-PPI group (11.3%) and 63 patients in the IC-PPI group (35.8%) developed complications (p < 0.001). Many patients had multiple complications, accounting for the duplicate number of cases shown in Table 2a. The most frequent complication in the OC-PPI group was malnutrition (6/7 patients) while stricture was the most common in the IC-PPI group. Compared to IC-PPI, OC-PPI resulted in lower recurrence (17% vs. 31.8%,
p=0.03). Prescribed PPI potencies were standardized using daily Omeprazole Equivalence (OE). The odds ratio was calculated and adjusted for adequacy of OE potency-adequacy defined by stable or higher OE after MU diagnosis. When adjusted for PPI potency, the association between MU recurrence in OC-PPI compared to IC-PPI decreased by 57% (adjusted OR, 0.43; 95% CI, 0.19-0.95). Furthermore, there was a decreased association between MU complication rate in OC-PPI group compared to IC-PPI group by 75% (adjusted OR, 0.25; 95% CI, 0.10-0.58).
Conclusion: OC-PPI is significantly associated with fewer MU complications and lower recurrence of MU after RYGB compared to IC-PPI. These results support the ongoing paradigm shift towards utilizing OC-PPI in patients with altered foregut anatomy and absorption to reduce the overall personal and healthcare burden of marginal ulceration.
Back to 2024 Abstracts