Back to 2024 Abstracts
WHAT IS THE APPROPIATE ENDOSCOPIC SURVEILLENCE FOR POST-GASTRIC BYPASS MARGINAL ULCERATION?
Alison Zhao
*, Heesoo Yoo, Alvin Kwon, Varun Aitharaju, Kristelle J. Imperio-Lagabon, Bailey Flora, Roma Patel, Stephen A. Firkins, Rehan Haidry, Roberto Simons-Linares
Gastroenterology, Cleveland Clinic, Cleveland, OH
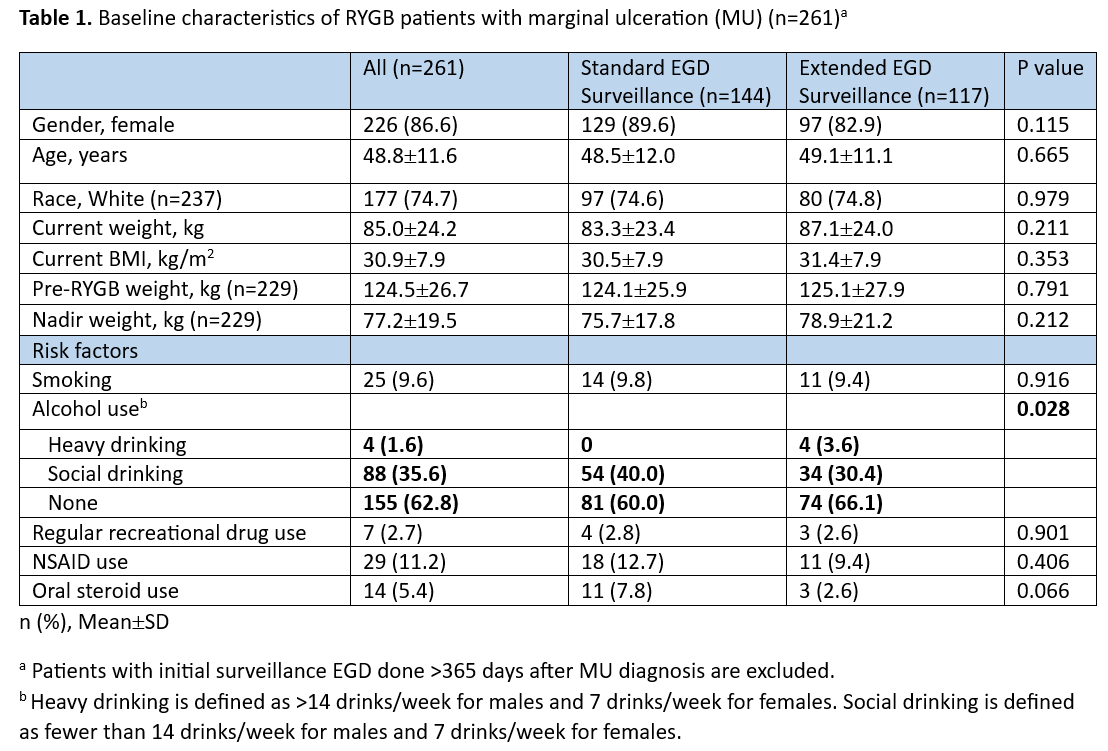
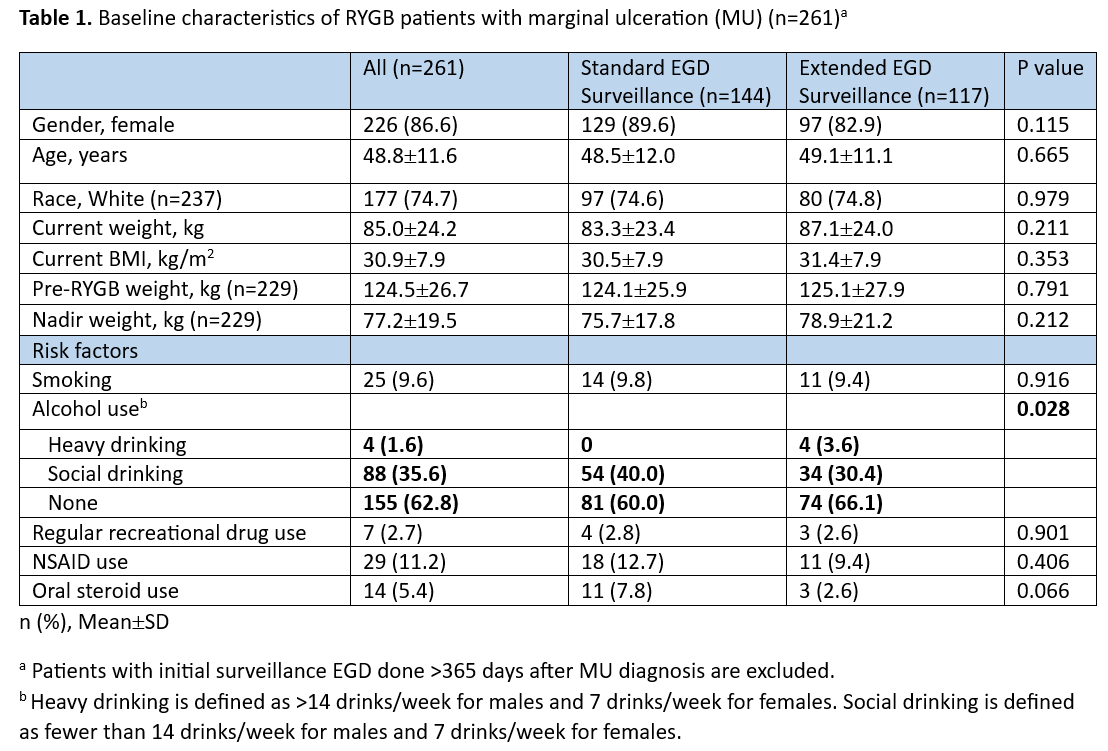
Background: Marginal ulceration (MU) following Roux-en-Y gastric bypass (RYGB) is not an uncommon complication and its prevalence ranges from 1-20%. There is limited evidence to support current common clinical practice involving surveillance esophagogastroduodenoscopy(sEGD) every three months to assess ulcer healing after initial diagnosis. This study aims to characterize MU healing and complications in patients who received
standard sEGD (≤100 days from diagnosis) versus
extended sEGD (>100 days).
Methods: A single-center, retrospective study of patients with RYGB diagnosed with MU on endoscopy from August 1, 2016 to April 3, 2022 was conducted. Patients without confirmed MU diagnosis and those who received initial EGD surveillance more than one year after MU diagnosis were excluded. Patient demographics and history, ulcer details and complications, and endoscopic surveillance timing were collected. The primary outcome was time to ulcer healing, and secondary outcome was complications related to MU. Logistic regression analysis was performed to evaluate associations between
standard sEGD versus
extended sEGD and predefined key variables.
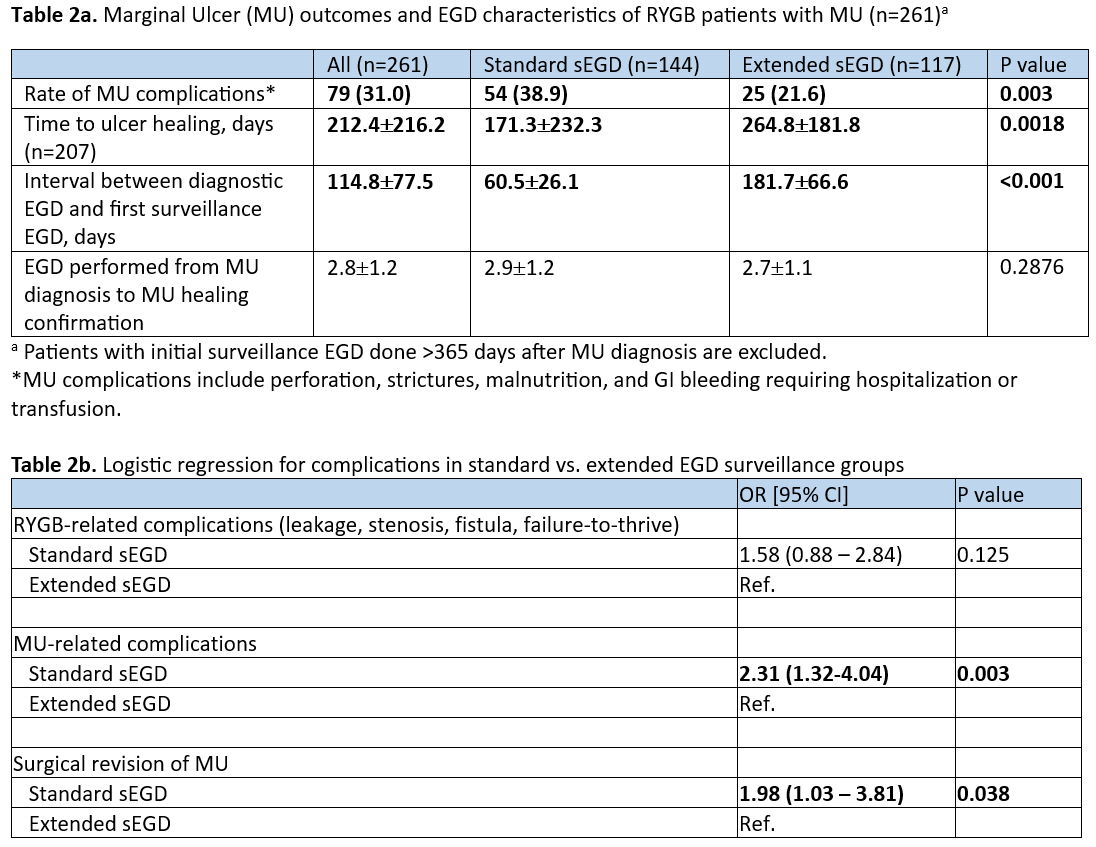
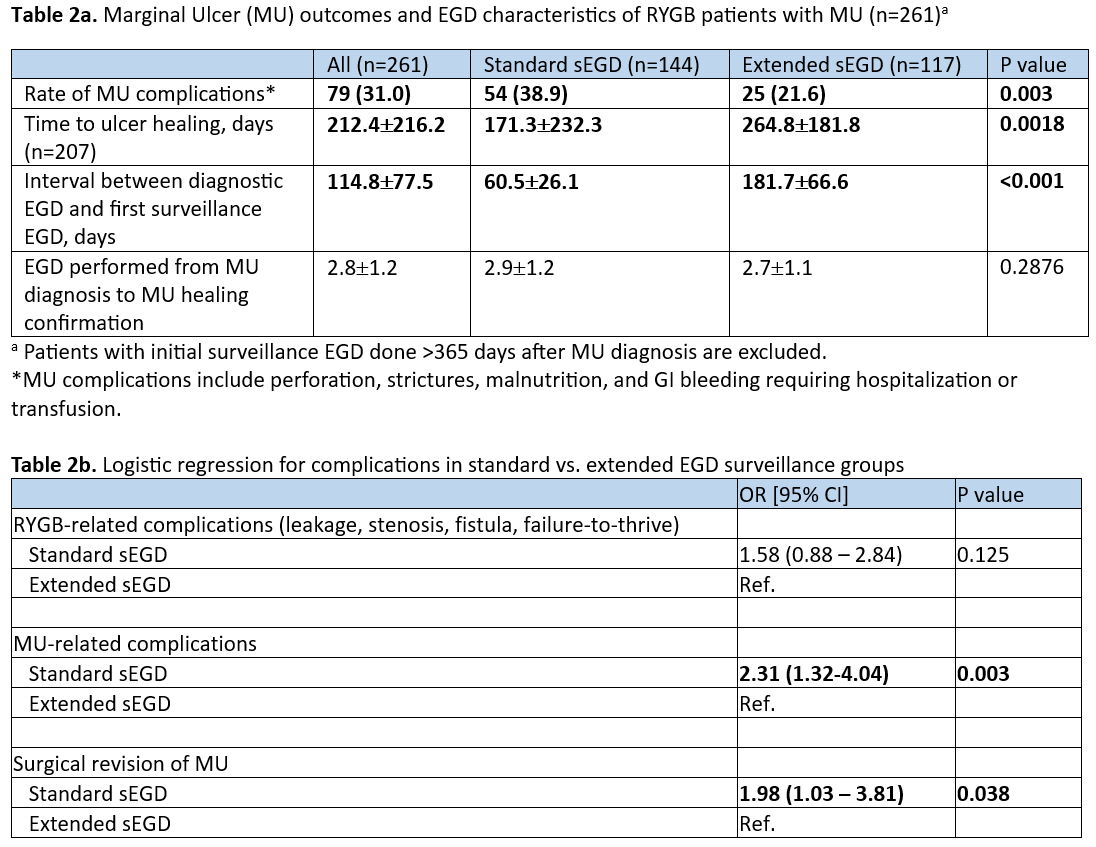
Results: A total of 355 RYGB patients with confirmed MU were included. Of these, 261 patients had at least one sEGD within one year after MU diagnosis, with 55.2% receiving
standard sEGD, and 44.8% receiving
extended sEGD. There was no significant difference in demographics or MU risk factors between groups except alcohol use. Time to ulcer healing was significantly shorter with
standard sEGD (171.3 days vs. 264.8 days
, P = 0.0018). Rate of MU-related complications was significantly higher in the
standard sEGD group (38.9% vs. 21.6%,
P = 0.003). There were increased odds of MU-related complications (odds ratio [OR] 2.31; 95% CI 1.32 – 4.04,
P = 0.003) and MU-related surgical revision (OR 1.98; 95% CI 1.03 -3.81;
P = 0.038) in the
standard sEGD group compared to
extended sEGD.
Conclusion: Based on our study, s
tandard surveillance EGD (<100 days after MU diagnosis) detects more complications but is associated with faster time to MU healing. This is likely due to earlier detection of MU complications leading to earlier optimization of MU management. This study provides pioneering evidence to support current clinical practice of surveillance EGD for MU. Our group proposes an interval of EGD surveillance every 3 months for optimal management of MU.
Back to 2024 Abstracts