Back to 2024 Abstracts
PREDICTORS OF POSTOPERATIVE BLEEDING AFTER ROBOTIC AND LAPAROSCOPIC BARIATRIC SURGERY
Alba Zevallos
*1, Jorge Cornejo
1, Joaquin Sarmiento
1, Christina Li
1, Gina Adrales
2, Michael Schweitzer
2, Raul Sebastian
2,11General Surgery, Northwest Hospital, Randallstown, MD; 2Johns Hopkins Medicine, Baltimore, MD
Background: Bariatric minimally invasive surgical approaches offer patients effective weight loss with fewer postoperative complications. However, although rare especially using the robotic approach, postoperative bleeding remains a concern as it can lead to significant morbidity and mortality. We assessed the predictor factors associated with postoperative bleeding after laparoscopic and robotic sleeve gastrectomy (SG) and Roux-en-Y gastric bypass (RYGB).
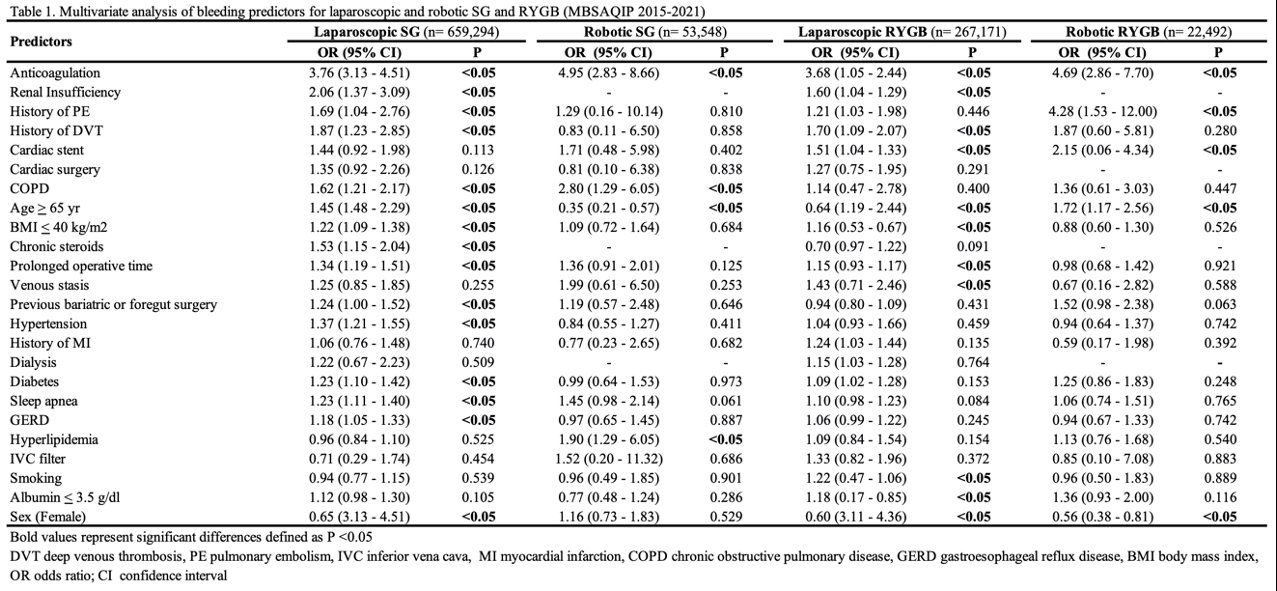
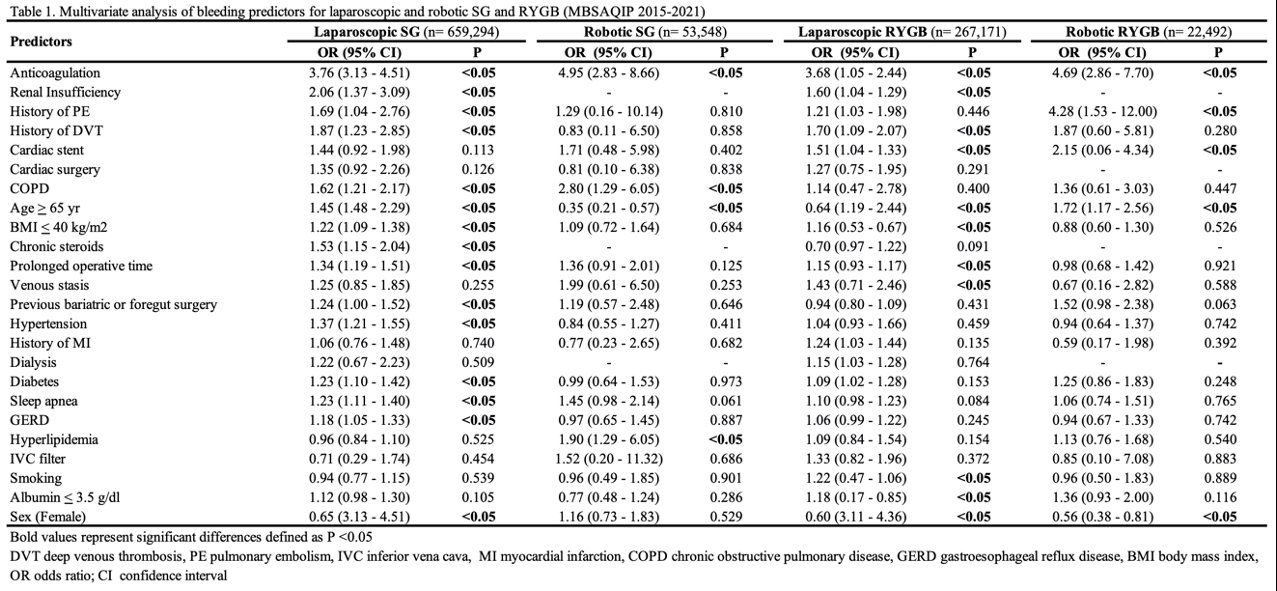
Methods: Patients who underwent SG and RYGB were included using the 2015–2021 MBSAQIP database. Four multivariate logistical regression analyses were performed between postoperative bleeding and the 24 independent factors for laparoscopic SG (lapSG), robotic SG (rSG), laparoscopic RYGB (lapRYGB), and robotic RYGB (rRYGB).
Results: A total of 1,002,505 patients were included (659,294 lapSG, 53,548 rSG, 267,171 lapRYGB, and 22,492 rRYGB). The incidence of postoperative bleeding was 0.2% for lapSG and rSG, and 0.6% for lapRYGB and rRYGB. Independent risk factors for postoperative bleeding are shown in Table 1. In lapSG the most important independent risk factors are anticoagulation (OR 3.76; 95% CI 3.13-4.51; P <0.05), renal insufficiency (OR 2.06; 95% CI 1.37-3.09; P <0.05), history of PE (OR 1.69; 95% CI 1.04-2.76; P <0.05), history of DVT (OR 1.87; 95% CI 1.23-2.85; P <0.05), COPD (OR 1.62; 95% CI 1.21-2.17; P <0.05), BMI
< 40 (OR 1.22; 95% CI 1.09-1.38; P <0.05), age
> 65 (OR 1.45; 95% CI 1.48-2.29; P <0.05), prolonged operative time (OR 1.34; 95% CI 1.19-1.51; P <0.05), and previous bariatric or foregut surgery (OR 1.24; 95% CI 1.00-1.52; P <0.05). In the rSG group factors comprised anticoagulation (OR 4.95; 95% CI 2.83-8.66; P <0.05), COPD (OR 2.80; 95% CI 1.29-6.05; P <0.05), and hyperlipidemia (OR 1.90; 95% CI 1.29-6.05; P <0.05). For lapRYGB risk factors included anticoagulation (OR 3.68; 95% CI 1.05-2.44; P <0.05), renal insufficiency (OR 1.60; 95% CI 1.04-1.29; P <0.05), history of DVT (OR 1.70; 95% CI 1.09-2.07; P <0.05), cardiac stent (OR 1.51; 95% CI 1.04-1.33; P <0.05), BMI
< 40 (OR 1.16; 95% CI 0.53-0.67; P <0.05), prolonged operative time (OR 1.15; 95% CI 0.93-1.17; P <0.05), and venous stasis (OR 1.43; 95% CI 0.71-2.46; P <0.05). Lastly, risk factors in the rRYGB group included anticoagulation (OR 4.69; 95% CI 2.86-7.70; P <0.05), history of PE (OR 4.28; 95% CI 1.53-12.00; P <0.05), cardiac stent (OR 2.15; 95% CI 0.06-4.34; P <0.05), and age
> 65 (OR 1.72; 95% CI 1.17-2.56; P <0.05).
Conclusions: Preoperative anticoagulation, renal insufficiency, history of VTE (DVT and PE), previous cardiac stent, COPD, BMI
< 40, and age
> 65 were found to increase the risk of postoperative bleeding. The predictor factors either using the laparoscopic or robotic approach in SG or RYGB were similar.
Keywords: Bleeding; Sleeve gastrectomy; Gastric bypass; Minimally invasive surgery
Back to 2024 Abstracts