Back to 2024 Abstracts
EVALUATION OF PROPHYLACTIC ENDOLUMINAL VACUUM THERAPY IN STOMACH: AN EXPERIMENTAL ANIMAL MODEL STUDY
Francisco Tustumi
*, Flávio Henrique F. Galvão, Eric T. Nakamura, Marina A. Pereira, Leonardo Cardili, Sandra N. Sampietre, Cinthia Lanchotte, Rubens A. Sallum, Venancio Avancini Ferreira Alves, Ulysses Ribeiro
Universidade de Sao Paulo Faculdade de Medicina, Sao Paulo, São Paulo, Brazil
Introduction: Anastomotic leak is one of the major complications of esophagogastric surgery. Vacuum endoscopic treatment has been used as an effective strategy for treating leaks. Considering the effectiveness of vacuum therapy, some authors suggest its prophylactic use in risky anastomoses. The objective of this work is to evaluate, in an experimental model, the effects of prophylactic endoluminal vacuum therapy in the stomach.
Methods: 34 Wistar rats were submitted to a gastric incision, which was later evaluated in macroscopic and histopathological analysis. The animals were divided into four groups.
Group 1 (10 rats): Animals subjected only to the gastric incision.
Group 2 (10 rats): Animals subjected to a gastric incision and a gastrostomy without endoluminal vacuum therapy.
Group 3 (7 rats): Animals subjected to a gastric incision and a gastrostomy with endoluminal vacuum therapy at -100 mmHg.
Group 4 (7 rats): Animals subjected to a gastric incision and a gastrostomy with endoluminal vacuum therapy at -300 mmHg. The animals were kept restrained for 48 hours, and after that, they were sacrificed. The outcomes investigated were gastritis, hemorrhage, adhesions, leak, mucosal erosions, fibrosis, and angiogenesis, measured by scores. The overall healing score was measured by summing the scores for angiogenesis and fibrosis and subtracting the score points from the necrosis score. Pathologists were blinded for histological examination.
Results: No leak was found. Fibrosis in incisions was higher in the vacuum groups (Groups I/II/III/IV: 80/60/100/100%; p=0.016). The necrosis rate was lower in Groups III and IV (Groups I/II/III/IV: 80/100/42.9/28.6%; p=0.006). However, Groups III and IV were associated with a higher risk for moderate/severe gastritis (Groups I/II/III/IV: 10/0/100/100%; p<0.001) and mucosal erosion (Groups I/II/III/IV: 0/0/100/85.7%; p<0.001). The gastritis was more intense in Group IV than in Group III (p<0.001). No significant differences were found for adhesions and angiogenesis (p>0.05). The overall healing score was higher for Groups III and IV (median score for Groups I/II/III/IV: 0.5/2/3/4; p=0.019), and this score did not differ between Groups III and IV (p=0.502).
Conclusion: This is the first experimental study evaluating the influence of vacuum therapy at different negative pressures in a gastrointestinal surgical animal model. Vacuum therapy promotes healing by reducing the incidence of necrosis and enhances fibrosis. Strong negative pressure as low as -300 mmHg is associated with a high risk for severe gastritis and mucosal erosion and has similar overall healing to vacuum therapy with -100 mmHg pressure.
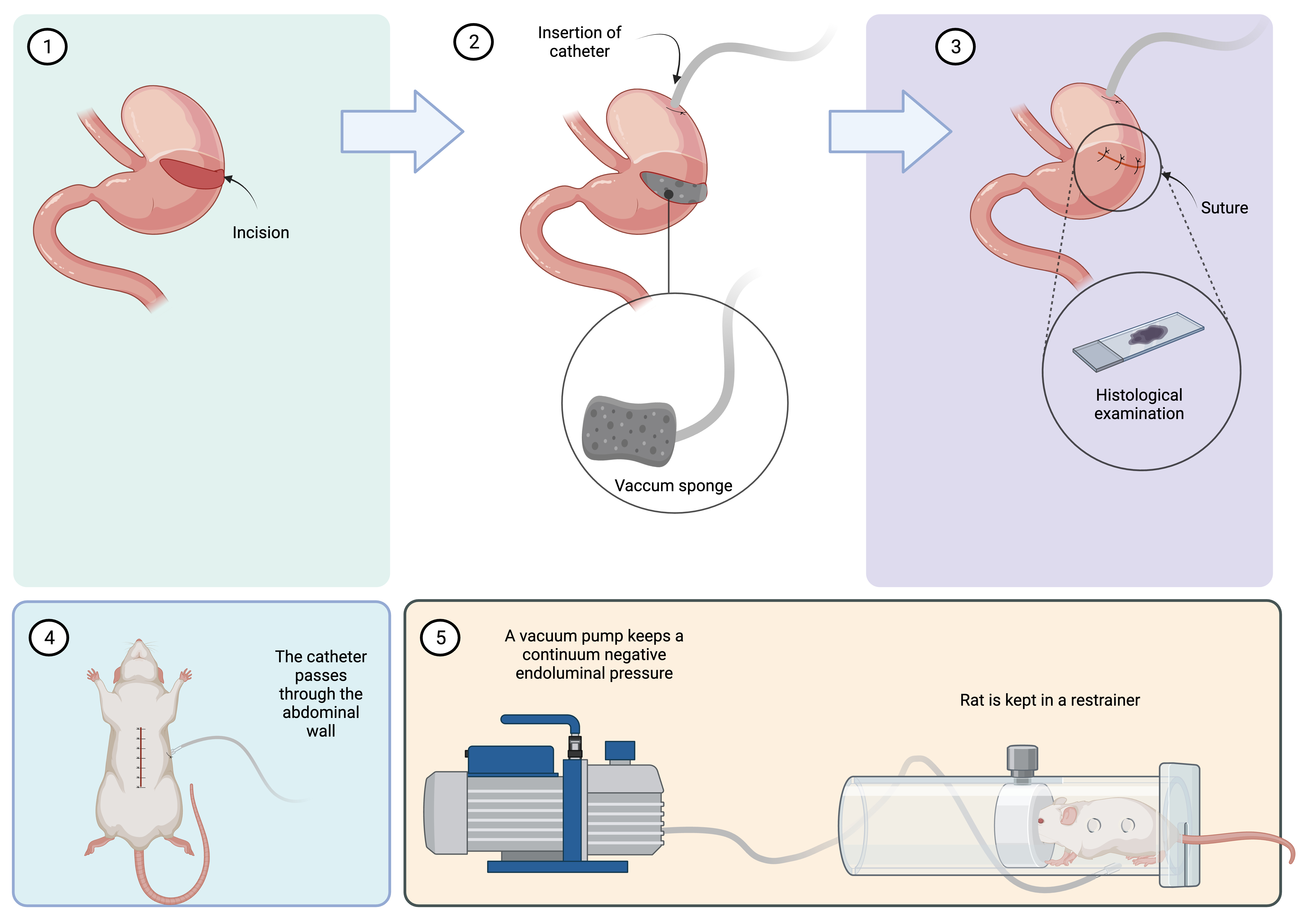
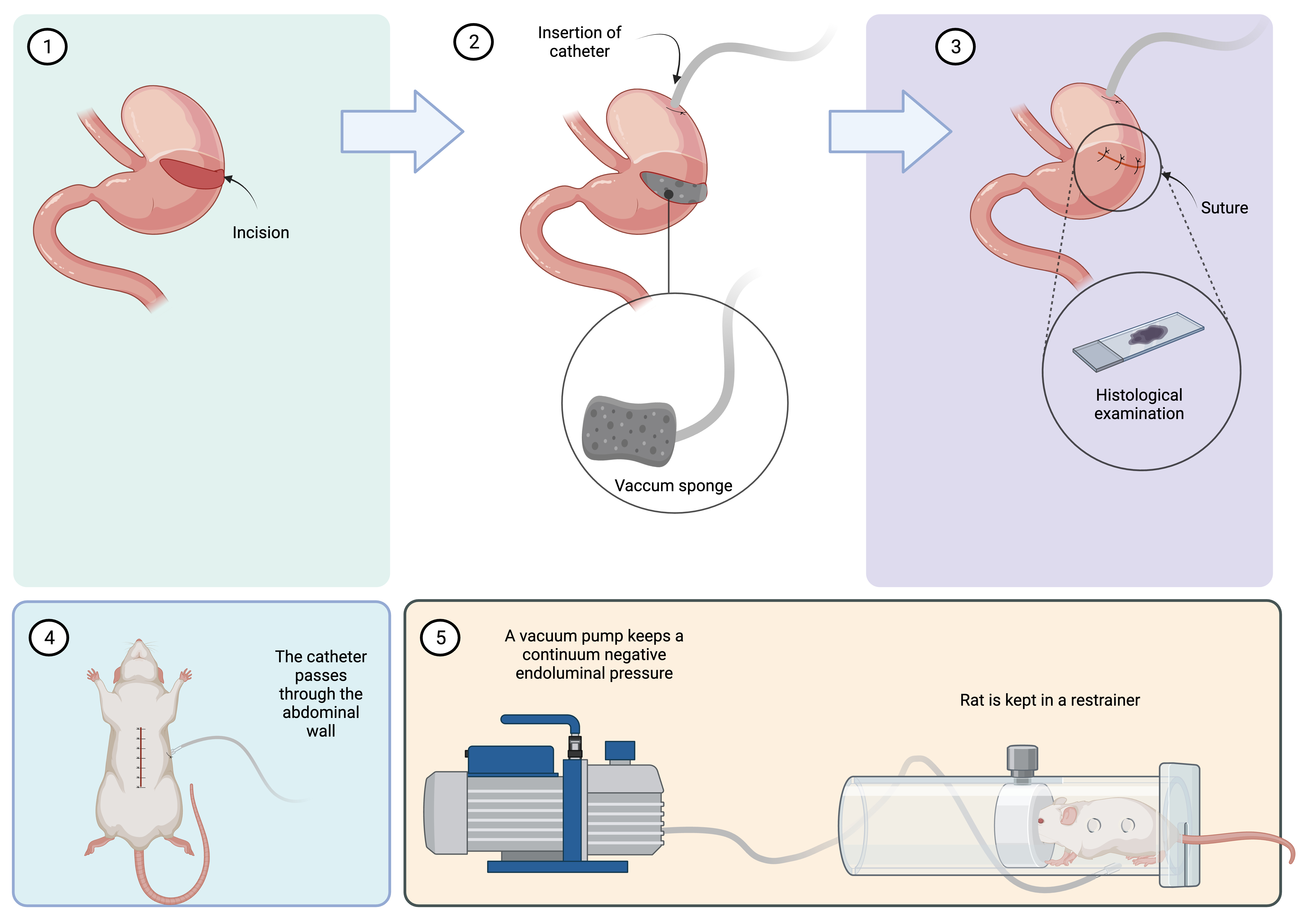 Figure 1.
Figure 1. The rat model was created by performing an incision in the stomach greater curvature (1). In Groups II, III, and IV, a gastrostomy catheter was inserted. A vacuum sponge was fixed on the tip of the catheter (2). The sponge was kept inside the gastric lumen, and the incision was closed (3). The gastrostomy catheter passed through the abdominal wall (4), and the rat was kept restrained for 48 hours (5). In Group II, no negative pressure was applied, while in Groups III and IV, a continuous negative pressure was applied (-100 and -300 mmHg, respectively). After 48 hours, the rat was euthanized, and the gastric incision was analyzed.
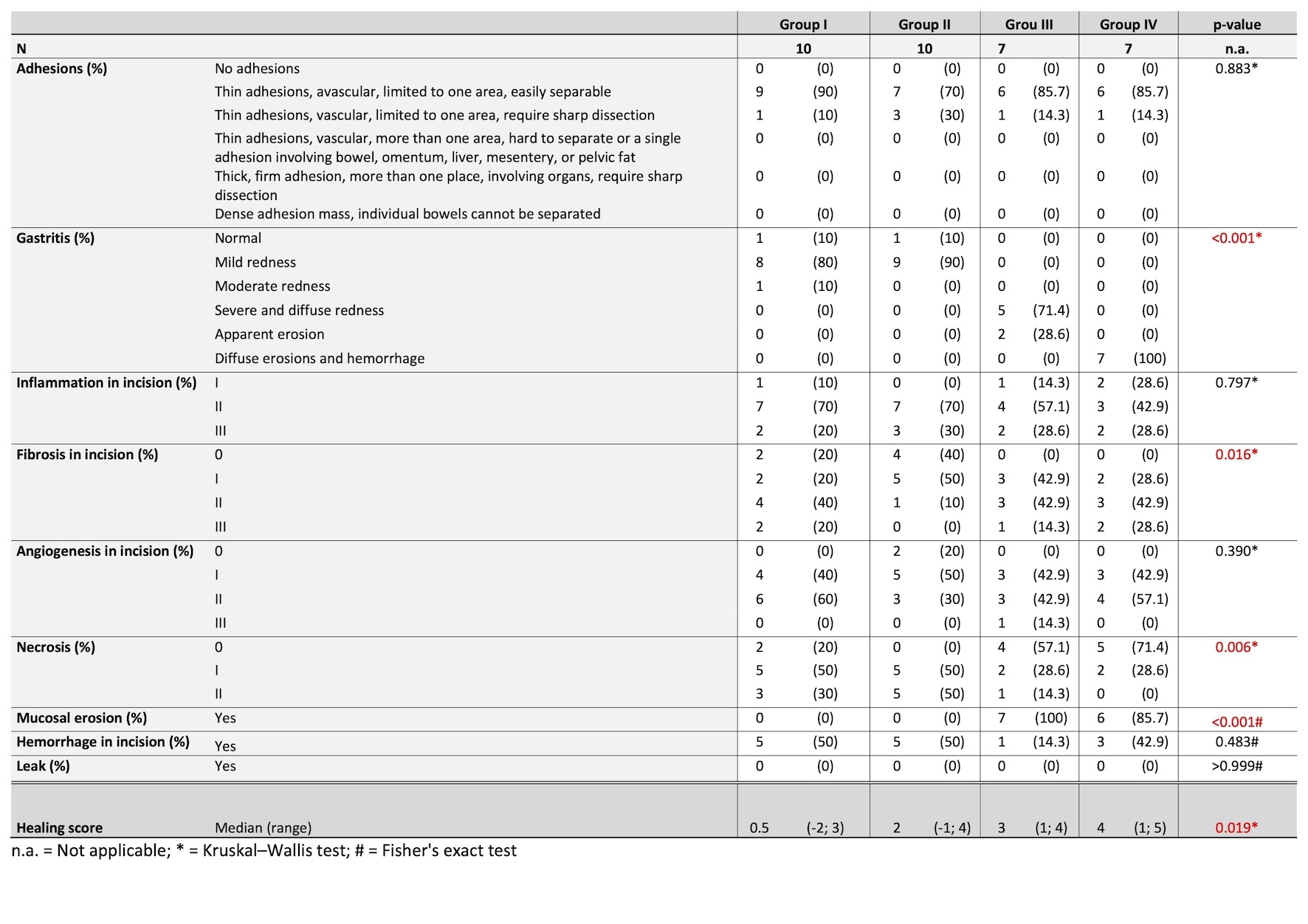
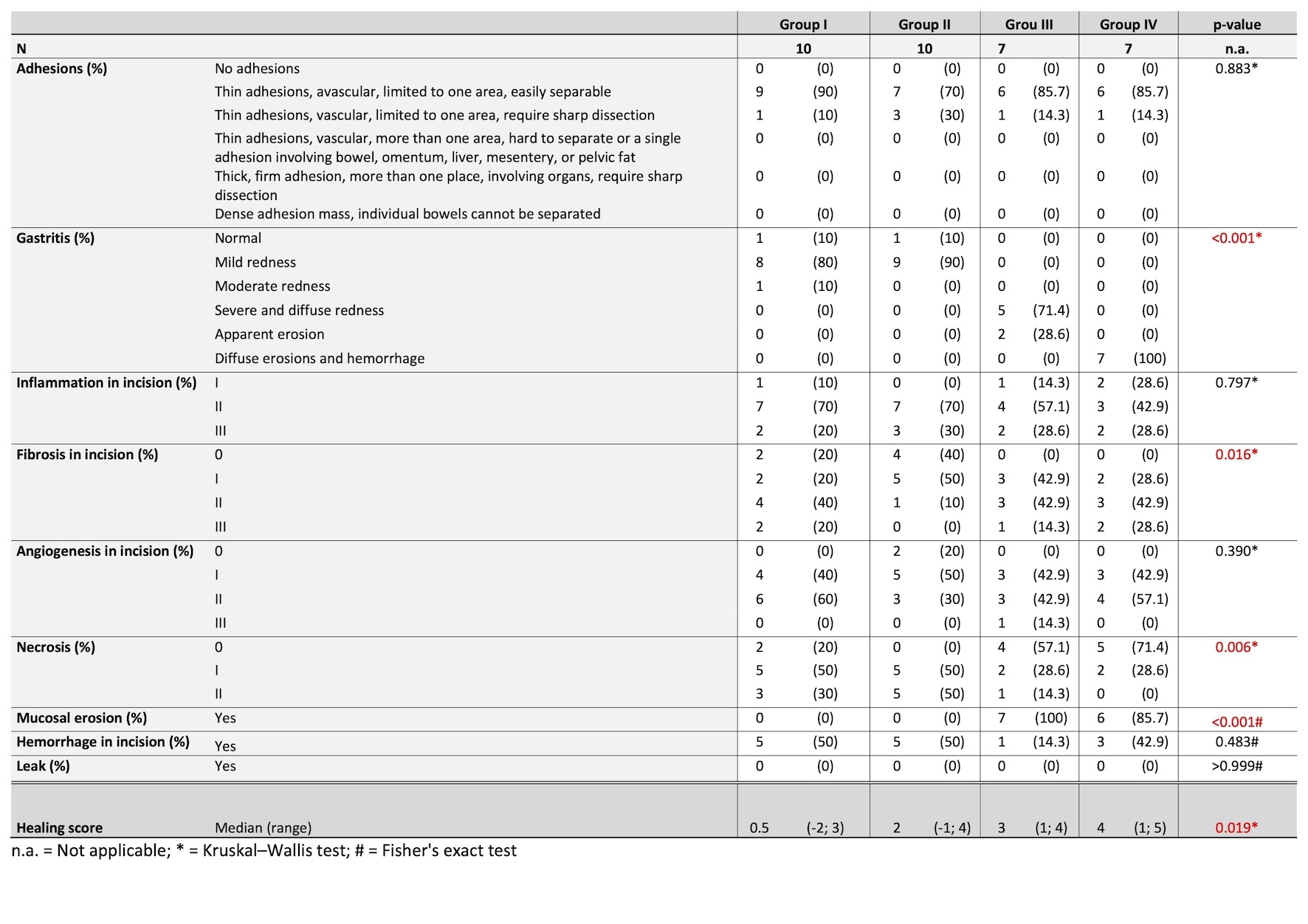 Figure 2.
Figure 2. Comparison among the studied groups. The outcomes were graded by scores. Red p-values show significant findings (p<0.05).
Back to 2024 Abstracts