Back to 2024 Abstracts
DIABETES SEVERITY SCORES PREDICT LONG-TERM DIABETES REMISSION AFTER METABOLIC AND BARIATRIC SURGERIES
Wissam Ghusn
*, Karl Hage, Robert A. Vierkant, Khushboo Gala, Andrew C. Storm, Barham K. Abu Dayyeh, Andres Acosta, Omar M. Ghanem
Mayo Foundation for Medical Education and Research, Rochester, MN
Background: Obesity is considered a major risk factor for developing multiple complications and medical conditions including type-2 diabetes mellitus (T2DM). Multiple scores (i.e., Individualized Metabolic Surgery [IMS], DiaRem, advanced DiaRem, and Robert et Al. scores) have been developed using components including T2DM medications and duration, Hba1c, insulin use, and BMI to predict T2DM remission (DR) after metabolic and bariatric surgery (MBS). This is the first study to use a large cohort undergoing Roux-En-Y Gastric Bypass (RYGB) and Sleeve Gastrectomy (SG) surgeries to assess the applicability of these scores in predicting DR with long-term follow up (>5 years) after MBS.
Methods: We conducted a cohort study including patients with T2DM undergoing either RYGB or SG. We collected demographic data, pre-operative data needed to calculate each of the 4 scores, and post-operative information related to DR and total body weight loss at last follow up visit. Areas under the receiver operating characteristics (ROC) curve (AUC) were calculated to assess the discriminatory ability of the four models to detect DR. In addition, we performed 2 sample independent t-test for continuous variables and chi squared test for categorical variables.
Results: A total of 503 patients (67% females, mean age 53.5 [11] years, BMI 46.2 [8.8] kg/m
2) with T2DM were included with a mean follow-up of 7.0 (3.6) years (
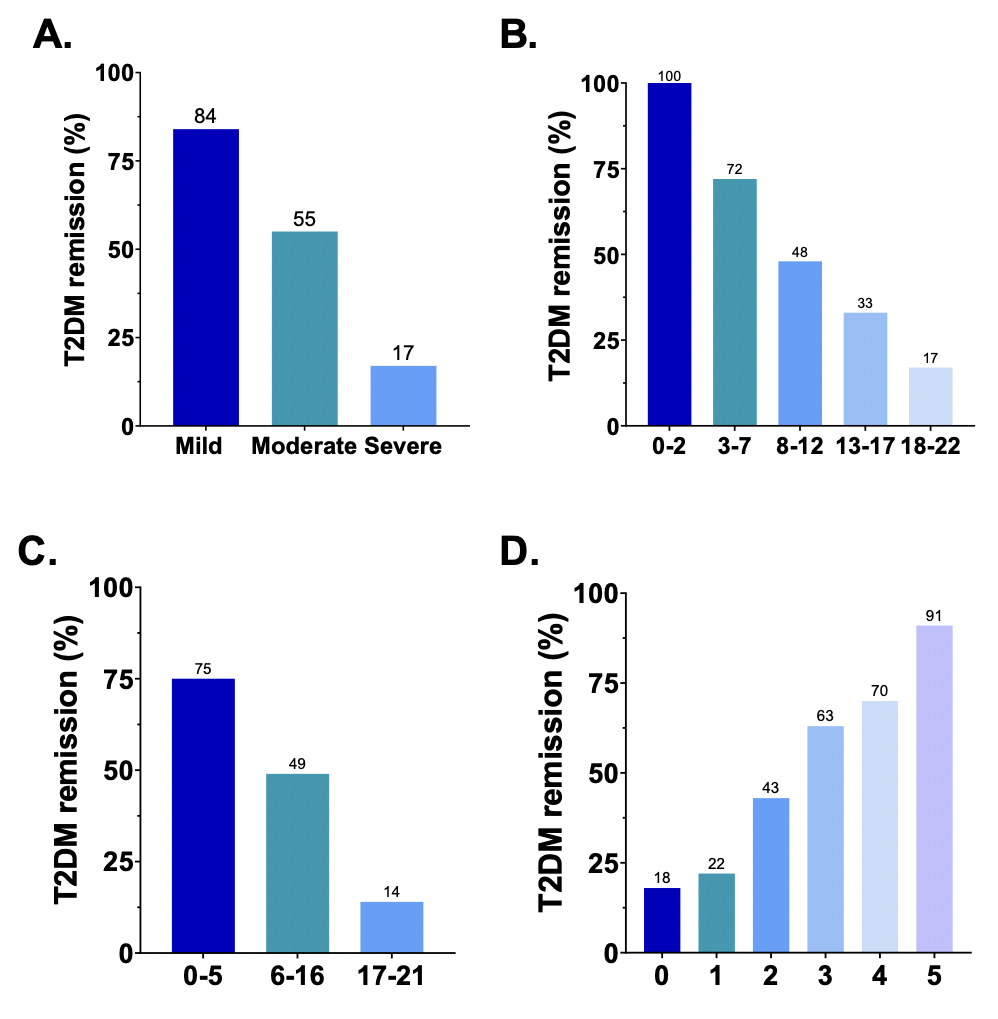
Table 1). All four scores predicted T2DM remission in our cohort with an ROC AUC of 0.79 for IMS, 0.78 for both DiaRem and advanced-DiaRem, and 0.75 for Robert et al. score. Specific subgroups for each of these scores demonstrated higher T2DM remission rates after RYGB compared to SG. A higher percentage of patients achieved DR in the mild category (84%) compared to 55% in the moderate category and 17% in the severe IMS category (p< 0.001) (
Figure 1A). The DR was also inversely proportional to the DiaRem score, decreasing from 100% in patients with a score of 0-2 to reach 17% in patients scoring 19-22 (p< 0.001;
Figure 1B). Similarly, there was a significant association between the score ranges and DR with 75% remission rate for scores between 0-5, 49% remission for 6-16, and only 14% for scores 17-21 in the advanced DiaRem (p<0.001;
Figure 1C). As for Robert et Al., the majority of patients (91%) with a score of 5 achieved remission compared to only 18% in patients with a score of 0 (
Figure 1D).
Conclusion: In this study, we validated the IMS, DiaRem, advanced-DiaRem and Robert et Al. scores in terms of predicting T2DM remission in patients who have undergone RYGB or SG. DR rates were demonstrated to be significantly associated with diabetes severity scores. Hence, a multidisciplinary approach must guide the treatment of T2DM in patients with obesity especially with a higher degree of severe diabetes.
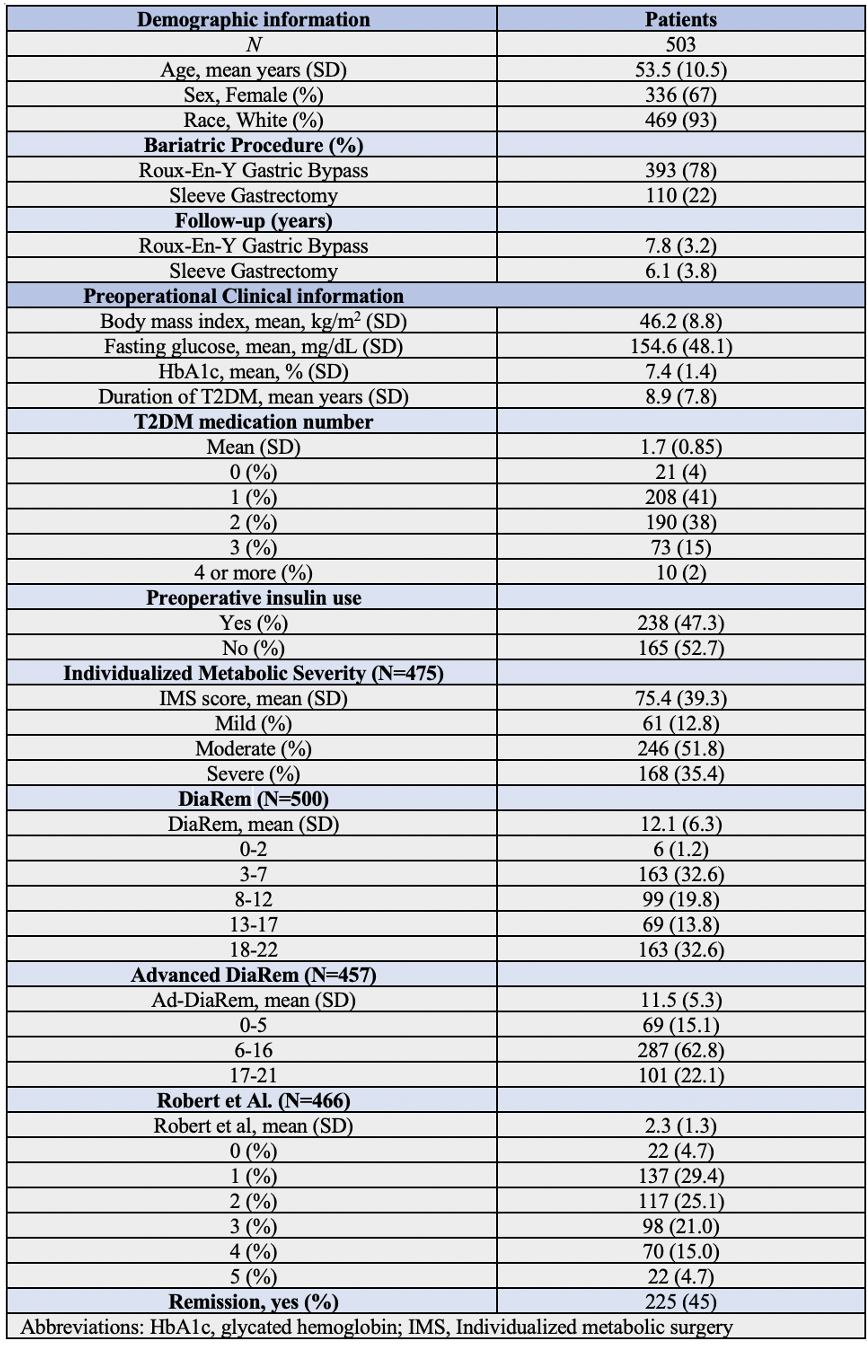
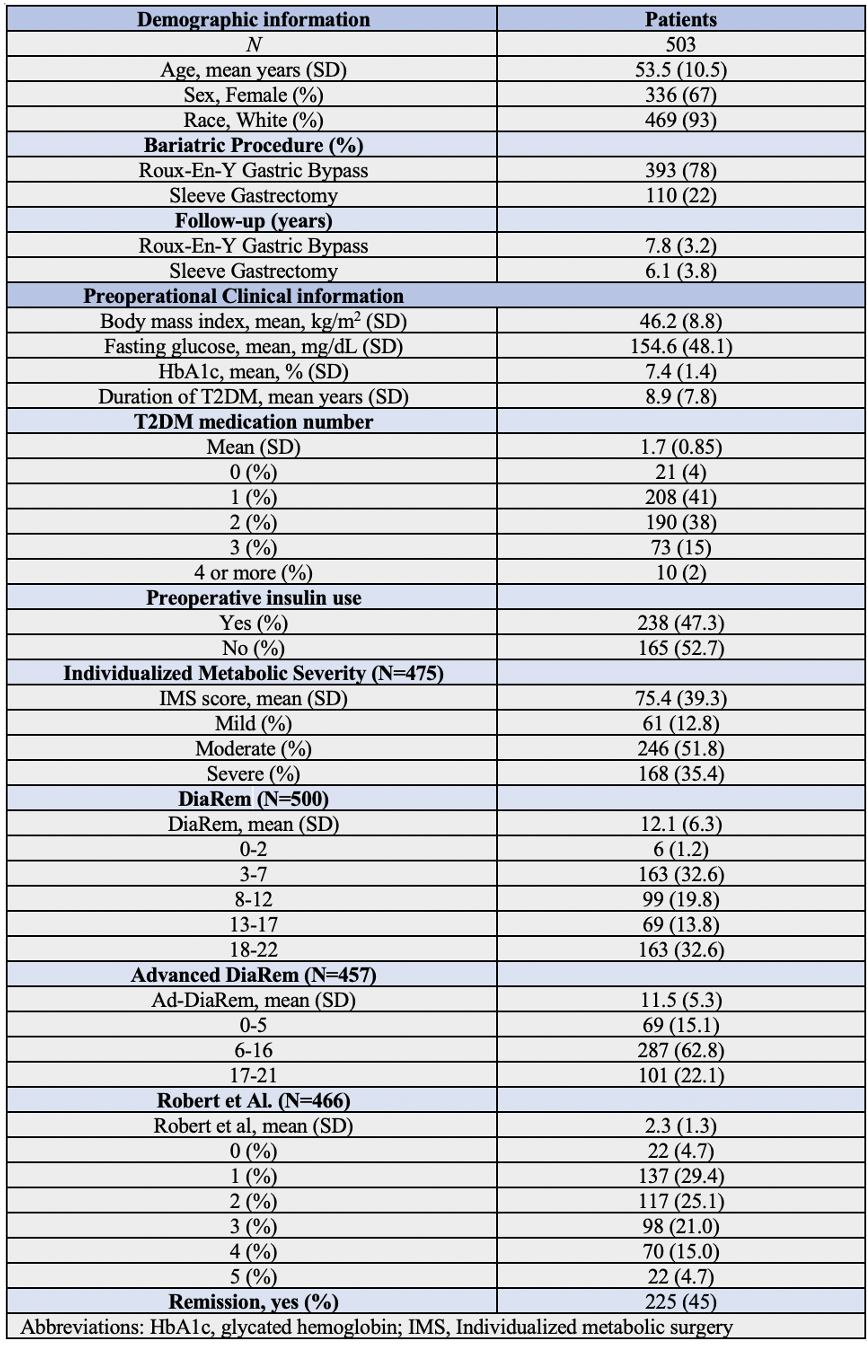 Table 1:
Table 1: Baseline demographic and clinical information. Data are presented as mean and standard deviation for continuous variables, and as frequency and percentage for categorical variables.
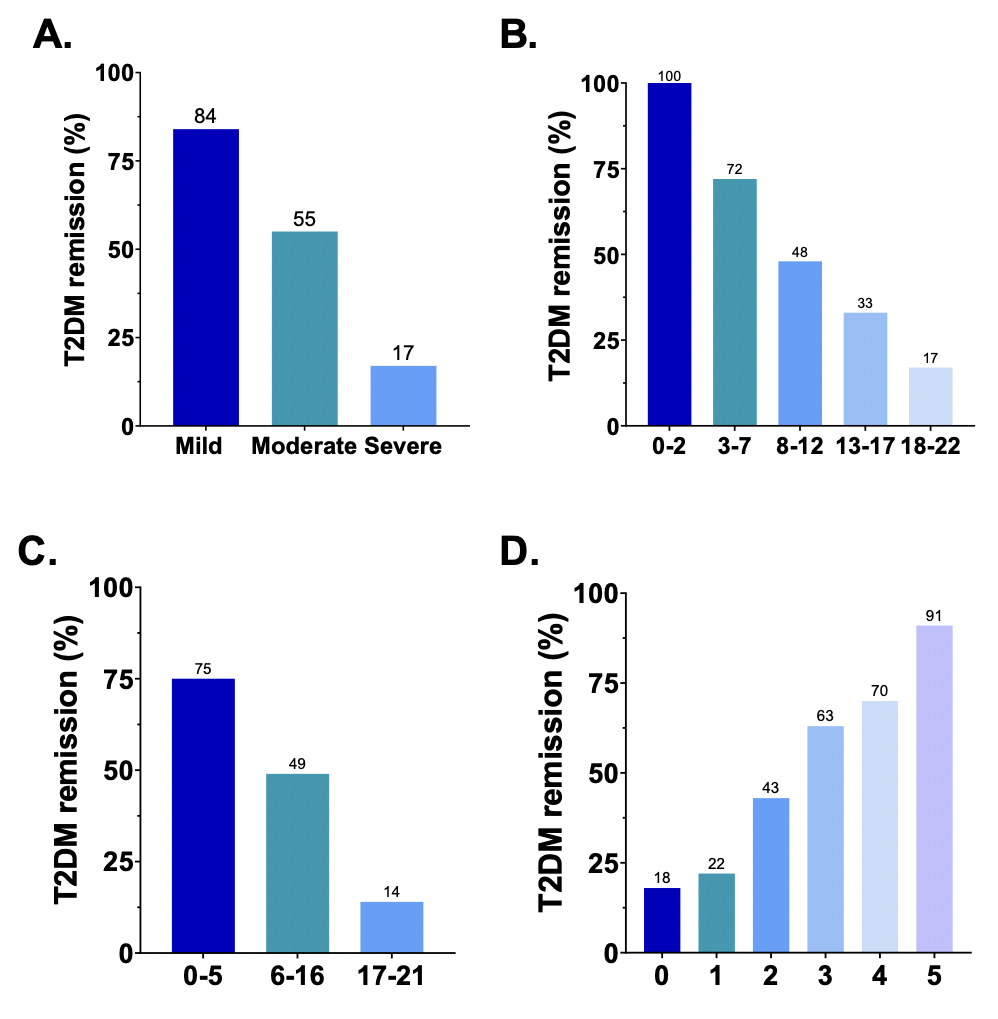 Figure 1:
Figure 1: T2DM remission percentage with IMS (A), DiaRem (B), advanced-DiaRem (C), and Robert et Al. (D) scores.
Back to 2024 Abstracts