Back to 2024 Abstracts
A NEGATIVE IMPACT OF SLEEVE GASTRECTOMY AND A POSITIVE IMPACT OF GASTRIC BYPASS ON ESOPHAGEAL ACID EXPOSURE, ESOPHAGEAL MOTILITY, AND ENDOSCOPIC FINDINGS: A SYSTEMATIC REVIEW AND META-ANALYSIS
Dirceu F. Valentini Jr
2, Guilherme S. Mazzini
*1, Gabriel L. da Silva
2, Arthur B. Simões
2, Vitória S. Gazzi
2, Julia B. O. Alves
2, Vinicius J. Campos
3, Richard R. Gurski
2,31Virginia Commonwealth University, Richmond, VA; 2Universidade Federal do Rio Grande do Sul, Porto Alegre, RS, Brazil; 3Hospital de Clinicas de Porto Alegre, Porto Alegre, RS, Brazil
Background: Current knowledge of the impact of bariatric surgery on esophageal outcomes is based mainly on reported symptoms. Baseline and follow-up objective measures of esophageal physiology and upper endoscopy (EGD) have been reported in retrospective or small prospective cohort studies. We aimed to assess the objective impact of Sleeve gastrectomy (SG) and Roux-en-Y Gastric Bypass (RYGB) on esophageal acid exposure, esophageal motility, and EGD.
Methods: We conducted a systematic review of the literature and selected studies that reported at least one objective measure of esophageal physiology and/or EGD, both at baseline and after either SG or RYGB. The meta-analysis summarizes the changes in pH-test, esophageal manometry, and EGD findings as mean differences (MD) and 95% confidence interval (95%CI). We also calculated weighted avarages for all objective parameters.
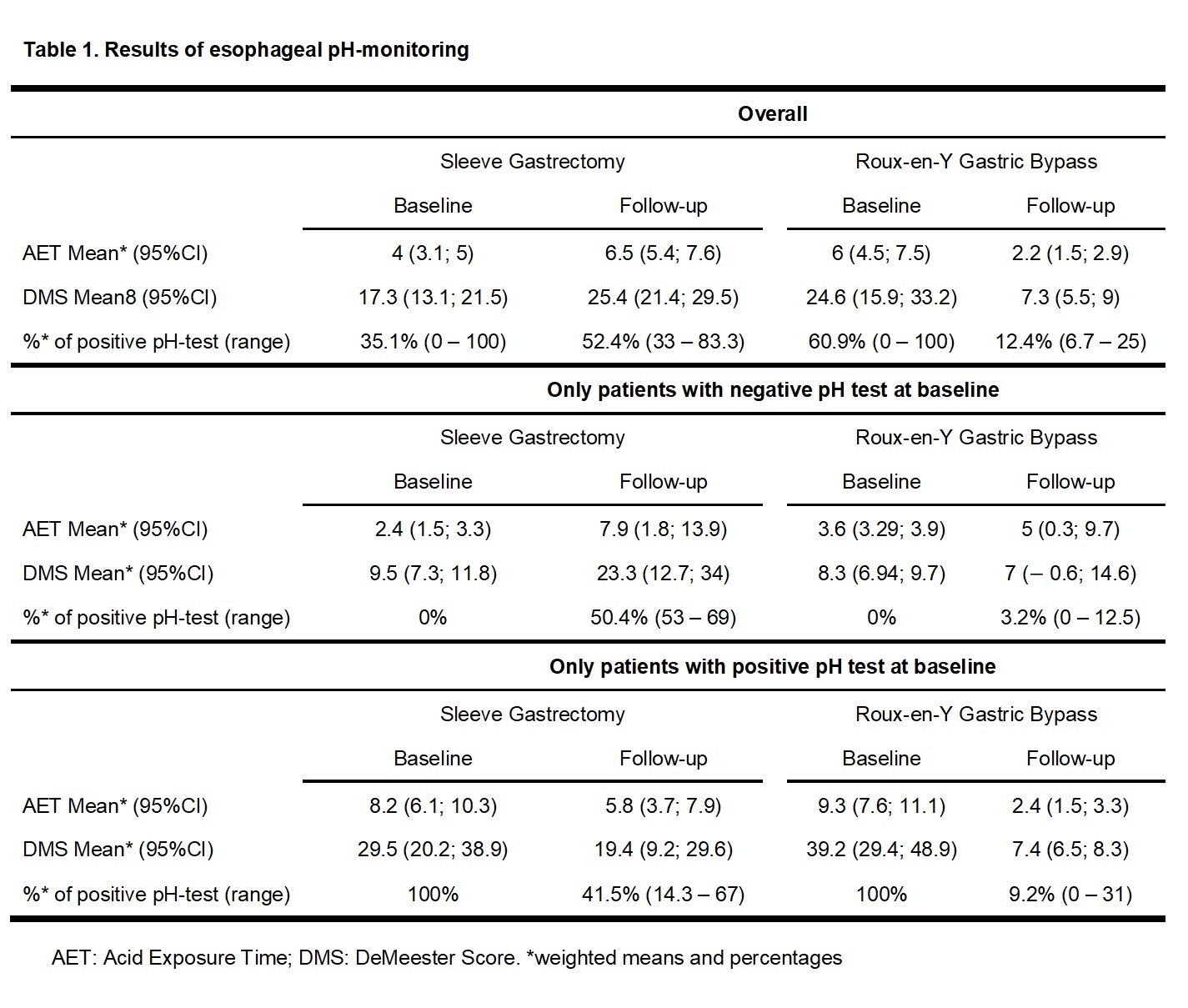
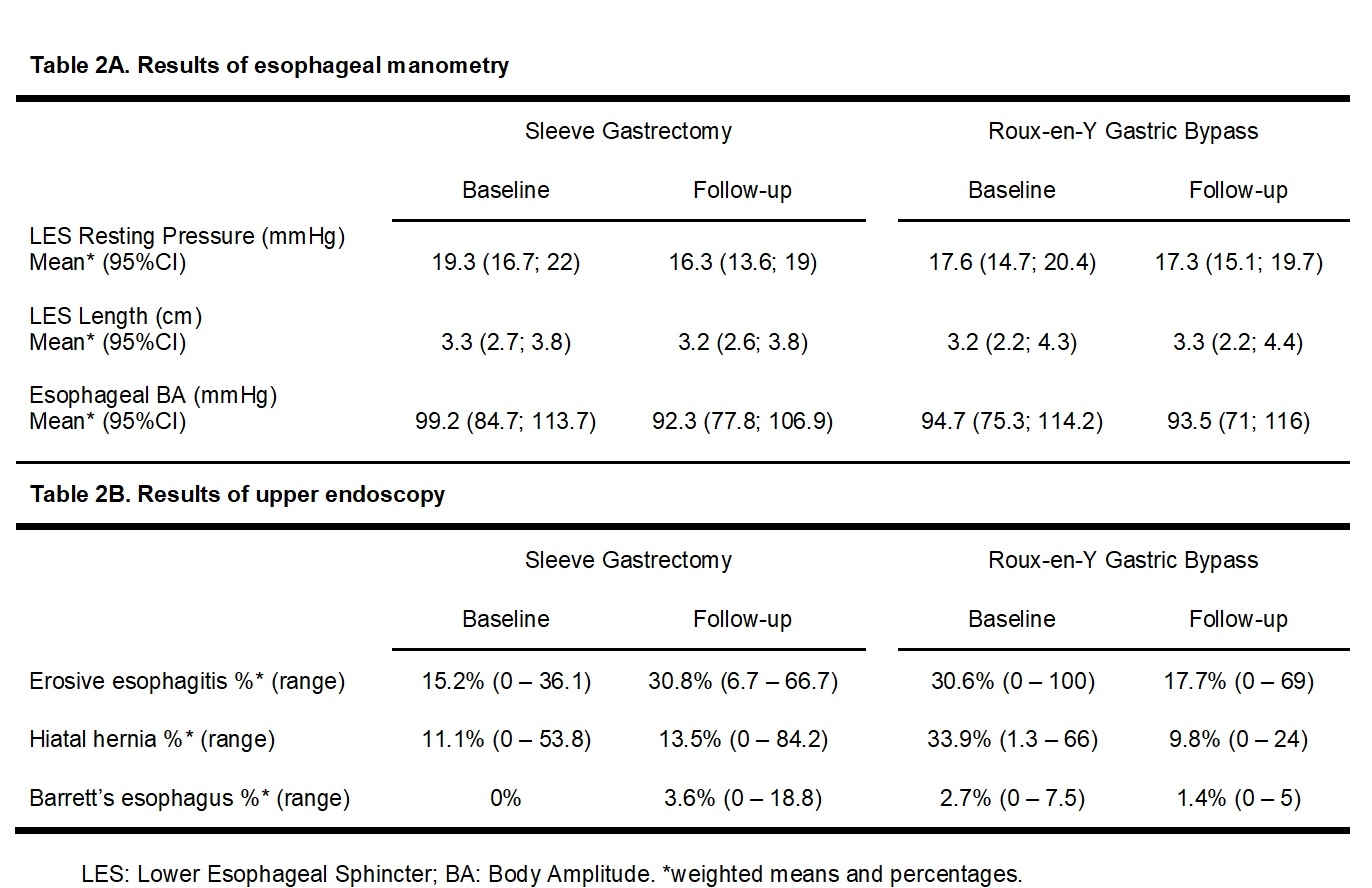
Results: Thirty-eight studies (2539 subjects) reported data on SG, while 17 studies (651 subjects) reported outcomes of RYGB. After SG there was a significant increase in acid exposure time (AET): MD 2.1 (95%CI 0.3 to 3.9) and in DeMeester Score (DMS): MD 8.6 (95%CI 2 to 15.2). After RYGB both AET and DMS significantly decreased: MD - 4.2 (95%CI -6.1 to -2.3) and MD - 16.6 (95%CI -25.4 to -7.8), respectively. Overall, the pooled weighted prevalence of a positive pH-test increased from 35% to 52% after SG and decreased from 61% to 12% after RYGB. The rates of a de novo positive pH-test were 50% after SG and 3% after RYGB (Table 1). Among patients with a positive pH-test at baseline, RYGB resulted in a significant improvement on both AET and DMS while no significant changes were observed after SG. The lower esophageal sphincter (LES) resting pressure and length significantly decrease following SG: MD - 2.8 (95%CI - 4.6 to - 1.1) and MD - 0.1 (95%CI - 0.2 to - 0.02), respectively (Table 2A). No significant manometric changes were observed after RYGB. The relative risk (RR) of erosive esophagitis was significantly increased after SG (RR: 2.3, 95%CI 1.5 to 3.5) and decreased after RYGB (RR: 0.4, 95%CI 0.2 – 0.8). The pooled weighted prevalence of Barrett's esophagus was 0% before and 3.6% after SG, while it decreased from 2.7% to 1.4% after RYGB (Table 2B).
Conclusion: We presented a comprehensive analysis of the impact of SG and RYGB on esophageal physiology and EGD. Overall, SG showed worsening of all parameters, while RYGB showed improvement in AET, DMS and EGD. Prospective studies are necessary to determine predictive factors associated with those changes, aiding in surgical choice regarding the expect reflux outcomes.
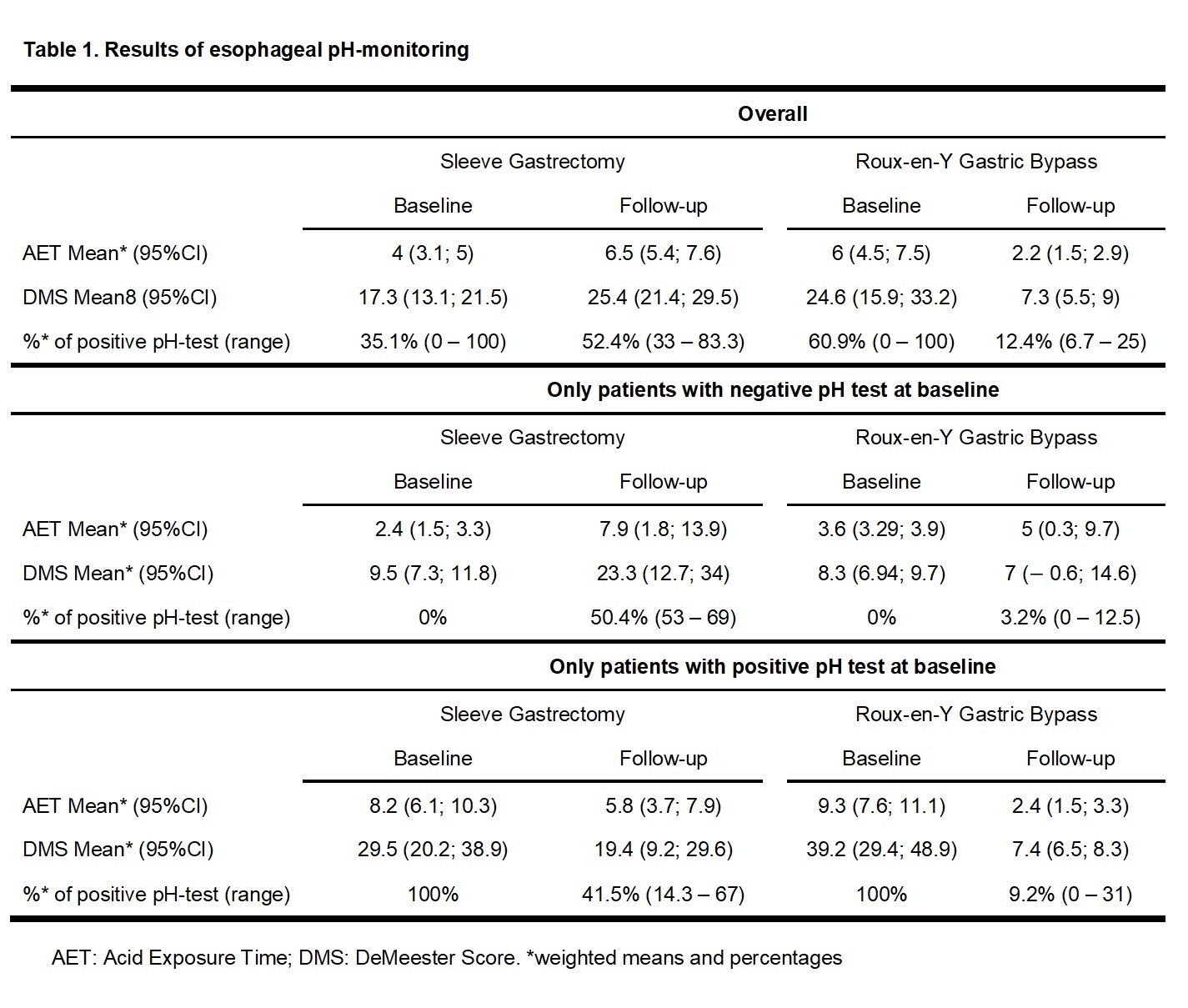 Table 1. Results of esophageal pH-monitoring
Table 1. Results of esophageal pH-monitoring 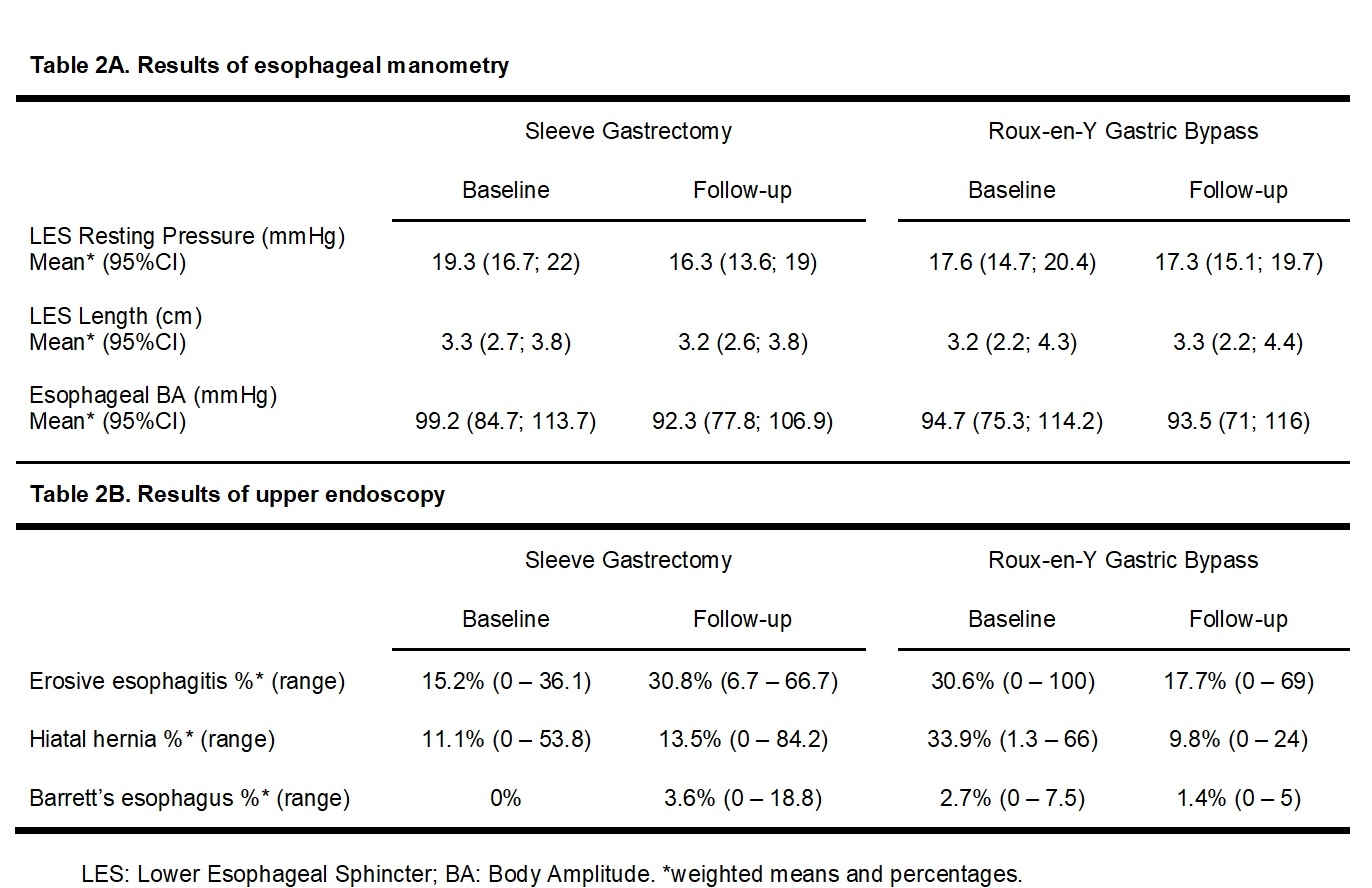 Table 2. Results of esophageal manometry and upper endoscopy
Table 2. Results of esophageal manometry and upper endoscopy
Back to 2024 Abstracts