Back to 2024 Abstracts
IMPACT OF PRIOR BARIATRIC SURGERY ON LABOR AND DELIVERY-RELATED OUTCOMES
Bhanu Siva Mohan Pinnam
*1, Shahroz Fatima
2, Violeta Popov
21Internal Medicine, John H Stroger Jr Hospital of Cook County, Chicago, IL; 2NYU Langone Health, New York, NY
AimObesity has become a widely prevalent comorbidity with far-reaching medical consequences. Consequently, bariatric surgical procedures are on the rise. There is limited literature on labor and delivery-related outcomes in patients with prior bariatric surgery. We assessed the impact of prior bariatric surgery on peripartum outcomes.
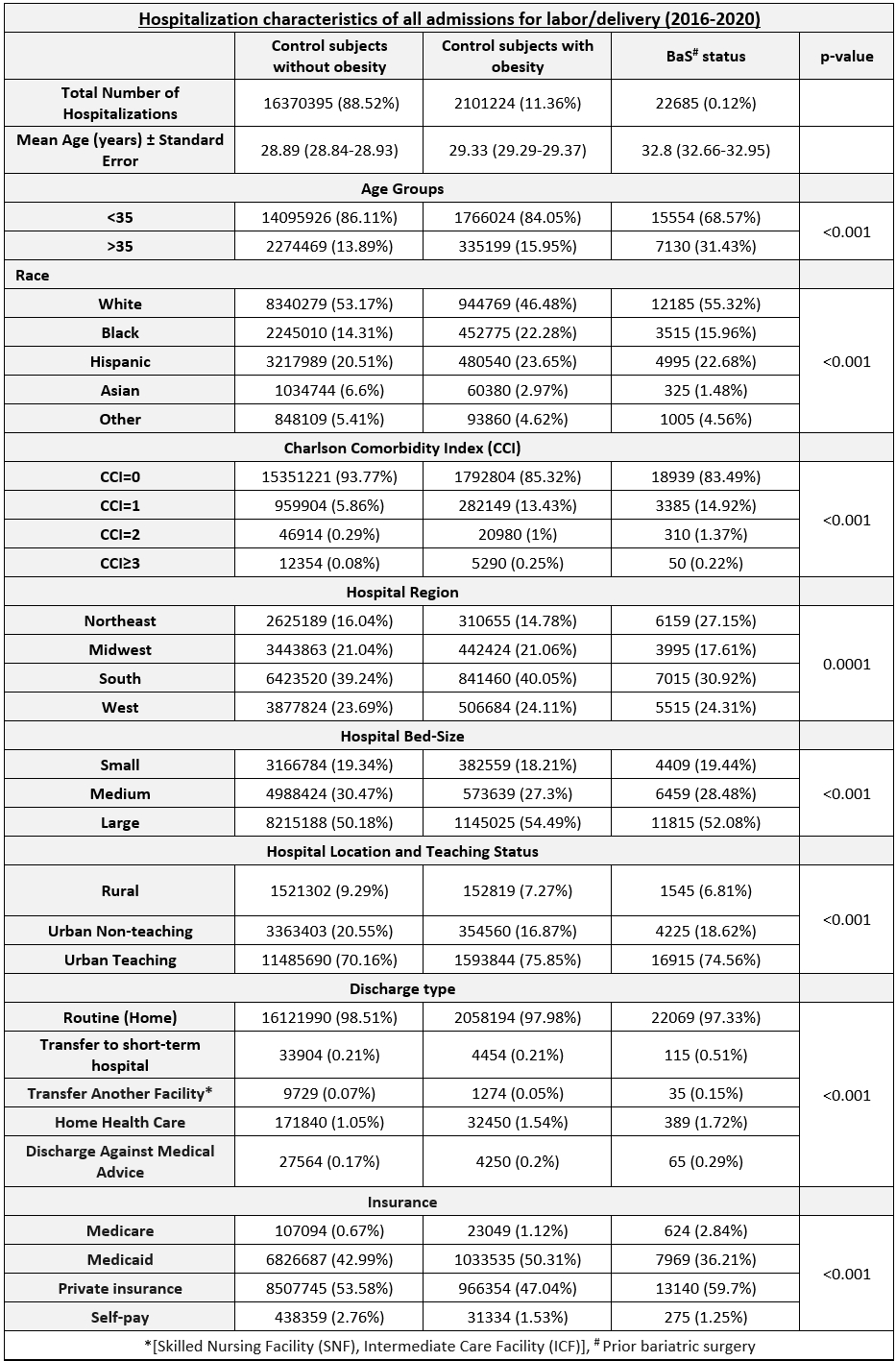
MethodsWe queried the National Inpatient Sample from 2016-2020 to identify admissions for labor and delivery and stratified them into three cohorts – cases with prior bariatric surgery (BaS), control subjects with obesity without prior bariatric surgery, and controls without obesity. We compared peripartum outcomes using a regression model, adjusting for potential confounders.
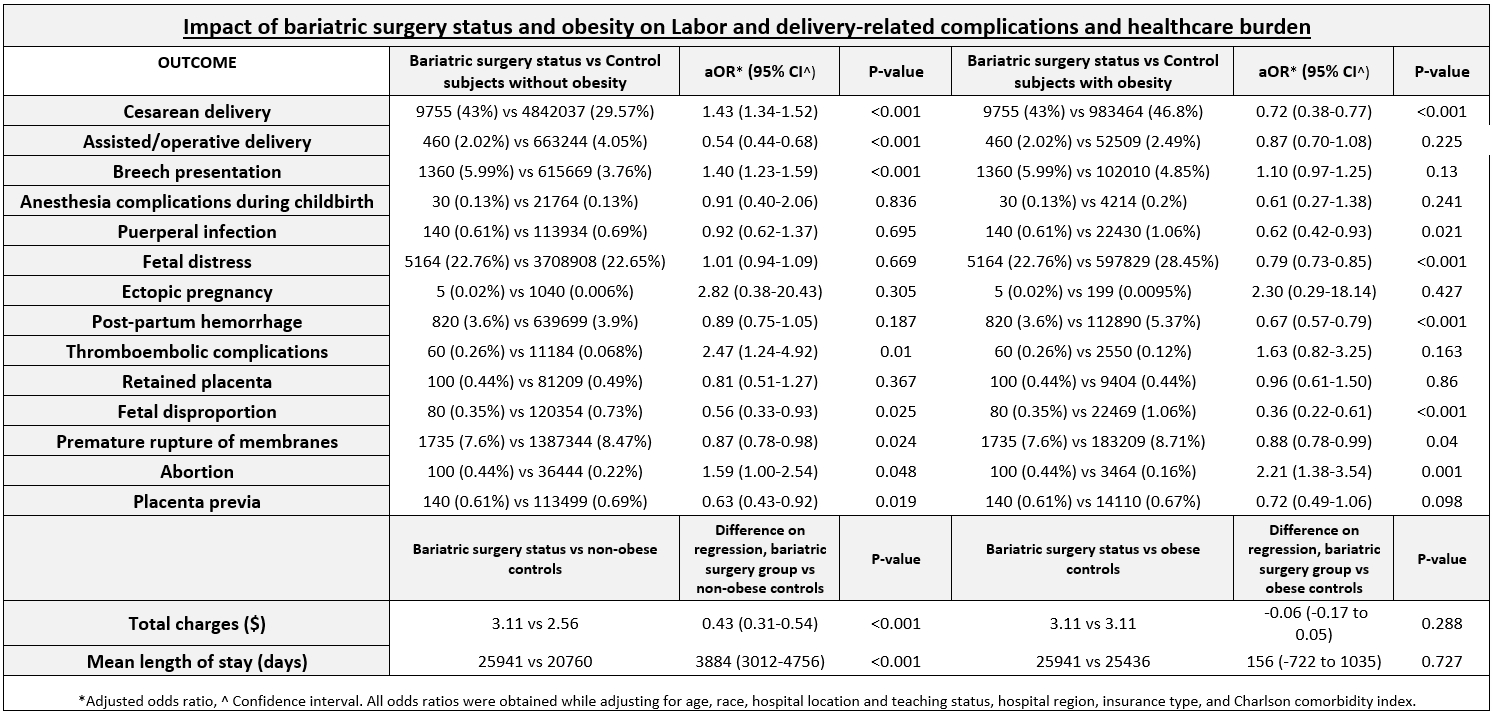
ResultsWe identified 22,685 cases in the BaS cohort, 2.1 million pregnant controls with obesity, and 16.37 million pregnant controls without obesity. Compared to controls with obesity, the BaS cohort had a lower rate of cesarean delivery (43% vs 46.8%, OR [odds ratio] 0.72, 95% CI [confidence interval] 0.38-0.77, P<0.001), fetal distress (22.7% vs 28.45%, OR 0.79, 95% CI 0.73-0.85, P<0.001), post-partum hemorrhage [PPH] (3.6% vs 5.37%, OR 0.67, 95% CI 0.57-0.79, P<0.001), fetal disproportion (0.35% vs 1.06%, OR 0.36, 95% CI 0.22-0.61, P<0.001), premature rupture of membranes [PROM] (7.6% vs 8.71%, OR 0.88, 95% CI 0.78-0.99, P=0.04), and a higher rate of pregnancy termination (0.44% vs 0.16%, OR 2.21, 95% CI 1.38-3.54, P=0.001). Compared to controls without obesity, the BaS group had a higher rate of cesarean delivery (43% vs 29.57%, OR 1.43, 95% CI 1.34-1.52, P<0.001), breech presentation (5.99% vs 3.76%, OR 1.4, 95% CI 1.23-1.59, P<0.001), thromboembolic events (0.26% vs. 0.068%, OR 2.47, 95% CI 1.24-4.92, P=0.01), and pregnancy termination (0.44% vs. 0.22%, OR 1.59, 95% CI 1.0-2.54, P=0.048) and a lower rate of assisted delivery (2.02% vs 4.05%, OR 0.54, 95% CI 0.44-0.68, P<0.001), fetal disproportion (0.35% vs 0.73%, OR 0.56, 95% CI 0.33-0.93, P=0.025), PROM (7.6% vs 8.47%, OR 0.87, 95% CI 0.78-0.98, P=0.024), and placenta previa (0.61% vs 0.69%, OR 0.63, 95% CI 0.43-0.92, P=0.019). Compared to controls without obesity, the BaS group experienced longer hospitalizations (3.11 vs 2.56 days, difference = 0.43, 95% CI 0.31-0.54, P<0.001) and higher hospitalization charges ($25941 vs $20760, difference = $3884, 95% CI $3012-$4756, P<0.001) but these outcomes were not significantly different when compared to controls with obesity.
ConclusionPrior history of bariatric surgery is associated with an increased risk of thromboembolic events, cesarean and assisted delivery, breech presentation, and abortion and, hence, should be treated as a high-risk pregnancy. It is helpful to note that these individuals have a lower risk of fetal distress, PPH, fetal disproportion, and PROM compared to subjects with obesity without a prior history of bariatric surgery.
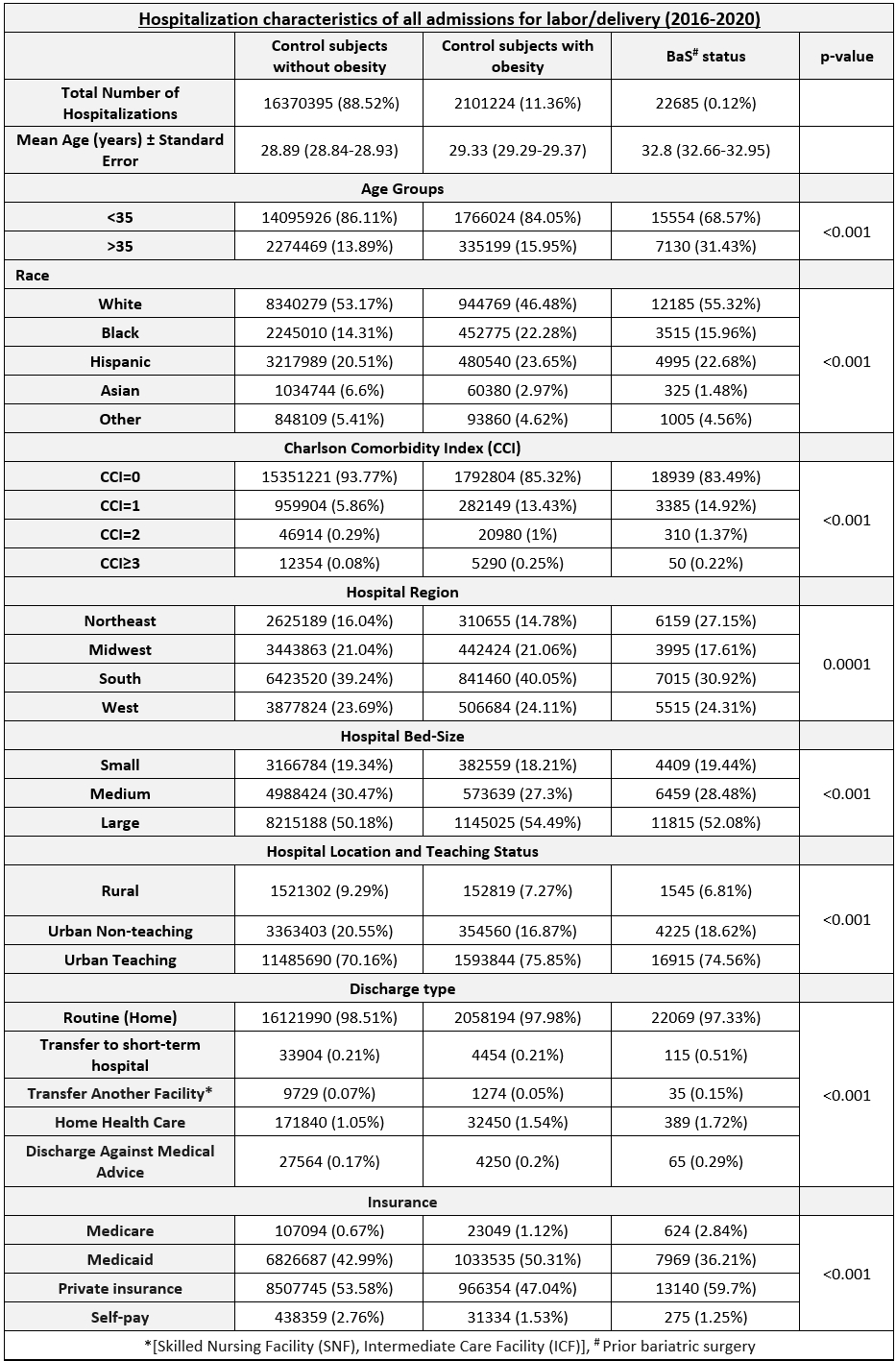
Table 1: Hospitalization characteristics of all labor and delivery-related admissions (2016-2020)
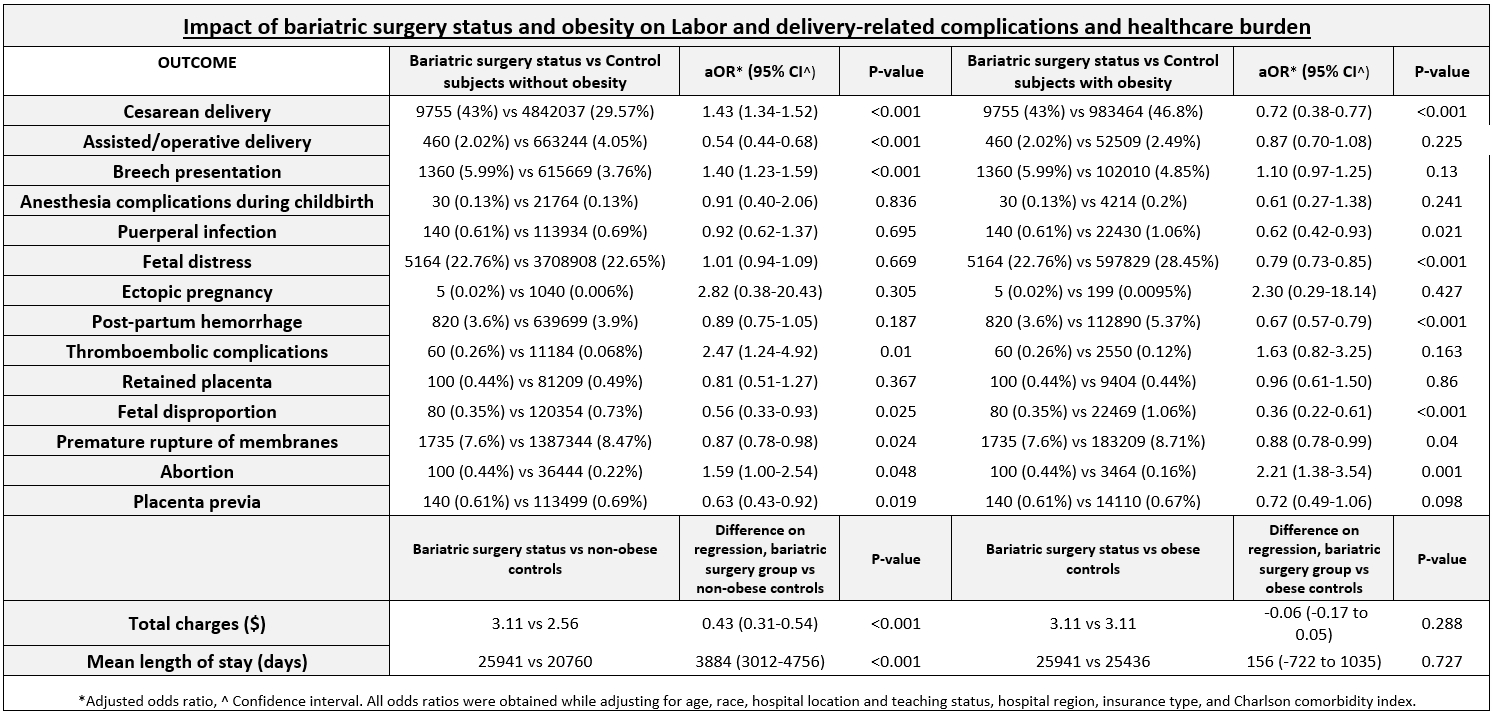
Table 2: Comparison of labor and delivery-related outcomes between patients with a prior history of bariatric surgery and control subjects with and without obesity.
Back to 2024 Abstracts