Back to 2024 Abstracts
IMPACT OF PRE-TRANSPLANT MALIGNANCY ON INTESTINAL TRANSPLANT OUTCOMES: AN ANALYSIS OF THE UNITED NETWORK FOR ORGAN SHARING DATABASE
Sarpong Boateng
*1,2, Prince A. Ameyaw
1,2, Eugene Annor
3, Kymberly D. Watt
4, Bubu A. Banini
21Internal Medicine, Yale New Haven Health System, New Haven, CT; 2Yale School of Medicine, New Haven, CT; 3University of Illinois Hospital & Health Sciences System, Chicago, IL; 4Mayo Clinic Minnesota, Rochester, MN
Background:A key barrier to transplant consideration in patients with pre-transplant malignancy (pre-TM) is the potential amplification of post-transplant malignancy risk in the setting of immunosuppression, ultimately impacting post-transplant mortality. Despite increased transplantation rates in patients with pre-TM, malignancy outcomes particularly in intestinal transplant (IT) recipients remain underexplored. We aimed to compare post-transplant outcomes between IT recipients with and without pre-TM in order to gain insights into malignancy recurrence and mortality rates.
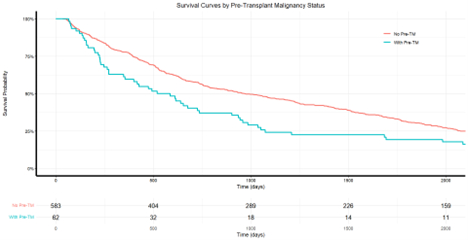
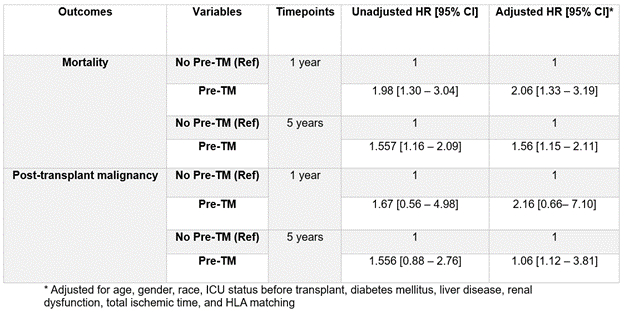
Methods:All adults in the United Network for Organ Sharing database who received IT from 1994 to 2017 were included in the study. We examined survival rates, demographic characteristics (including age, gender, and race), and clinical factors (such as ICU status before transplant, diabetes mellitus, liver disease, renal dysfunction, total ischemic time, and HLA matching) of IT recipients with pre-TM. We then compared post-transplant mortality and malignancy recurrence in IT recipients with and without pre-TM using multivariable Cox proportional analyses, with adjusted hazard ratios (HR) and 95% confidence intervals (CI).
Results:A total of 1,171 adults received IT between 1994 and 2017. Of these, 110 (9.4%) had pre-TM, while 186 (16%) developed post-transplant malignancy. From 1994 to 2017, the percentage of IT recipients with pre-TM increased from <1% to 17%. IT recipients with pre-TM had higher mortality at 1 year (22.72% vs. 12.40%, HR 2.06, 95% CI 1.33–3.19,
P=0.001) and 5 years post-transplant (45.45% vs. 38.22%, HR 1.56, 95% CI 1.15–2.11,
P=0.004). Post-transplant malignancy at 1 year did not differ significantly between the two groups (3.64% vs. 1.61%, HR 2.16, 95% CI 0.66–7.10,
P=0.2), but was higher in recipients with pre-TM at 5 years post-transplant (12.72% vs. 7.0%, HR 2.06, 95% CI 1.12–3.81,
P=0.021).
Conclusion:
The rising prevalence of pre-TM among IT recipients over the last two decades poses increased risks for post-transplant malignancy and mortality. These findings buttress the need for careful consideration of the risks and benefits of intestinal transplantation in patients with Pre-TM. Developing collaborative oncological care guidelines tailored to IT recipients could enhance post-transplant management and outcomes in this unique population.
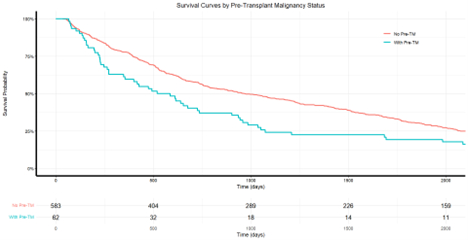 Survival Probabilities of Intestinal Transplant Recipients With and Without Pre-Transplant Malignancy
Survival Probabilities of Intestinal Transplant Recipients With and Without Pre-Transplant Malignancy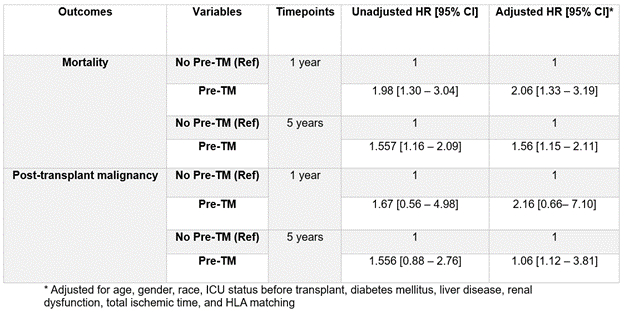 Table 1: Impact of Pre-Transplant Malignancy on Mortality and Post-transplant Malignancy
Table 1: Impact of Pre-Transplant Malignancy on Mortality and Post-transplant Malignancy
Back to 2024 Abstracts