Back to 2024 Abstracts
ENDOSCOPIC STENTING VS. BILIODIGESTIVE BYPASS SURGERY FOR ADVANCED PANCREATIC CANCER
Lucas C. Stolzemburg, Francisco Tustumi
*, Thiago C. Ribeiro, Ricardo Jureidini, Mauricio P. Sorbello, Fauze Maluf-Filho, José Jukemura, Ulysses Ribeiro, Guilherme Naccache Namur
Universidade de Sao Paulo Faculdade de Medicina, Sao Paulo, São Paulo, Brazil
Introduction: The main treatment options for cholestasis in advanced pancreas cancer are endoscopic stenting (ES), transhepatic drainage, and biliary bypass surgery (BBS). The aim of the current study is to compare the safety and efficacy of BBS and ES.
Methods: This is a retrospective cohort of patients with cholestasis and unresectable or metastatic pancreas cancer treated with BBS or ES. The following outcomes were extracted: complications, in-hospital death, length of stay, post-procedure palliative chemotherapy, overall survival, and treatment failure. We considered treatment failure as the need for hospital readmission due to biliary complications. Uni and multivariate Cox regression were performed, and p-values>0.1 in univariate analyses were selected for multivariate analyses. A 0.05 level of significance was adopted. Propensity score matching (PSM) analysis 1:1 was used as sensitivity analysis, matching ASA score, direct bilirubin levels, albumin, and ECOG performance status scale.
Results: 93 patients were included (BBS=43; ES=50). ES group had patients with higher levels of bilirubin (p=0.04) and worse ECOG (p=0.012), while BBS had more frequent gastroduodenal outflow obstruction (25
vs. 6%; p=0.017). There was no significant difference in age, sex, BMI, albumin, CA19-9, distant metastasis, the presence of locally advanced tumors, or history of previous biliary drainage. BBS was associated with a higher demand for postoperative intensive care (37
vs. 10%; p=0.002), longer ICU stay (1.44±2.47
vs. 0.66±2.24 days; p=0.004), and longer length of hospital stay (7.95±2.99
vs. 4.29±5.5 days; p<0.001). BBS had a higher risk for procedure-related complications (23 vs. 8%; p=0.049). There was no significant difference in bleeding and in-hospital mortality. In the BBS group, patients were more likely to undergo palliative chemotherapy (74
vs. 52%; p=0.026). There was no difference in overall survival between BBS and ES (p=0.089)
. On multivariate Cox regression, gastroduodenal outflow obstruction, distant metastasis, and ASA score were associated with survival, while the biliary drainage procedure (BBS
vs. ES) was not. ES was independently associated with a higher risk for treatment failure than BBS (HR=3.97; p=0.009). After PSM, the main baseline covariables were balanced between groups (p>0.05). The demand for ICU, ICU stay, and length of hospital stay were significantly higher for the BBS group, while palliative chemotherapy was not. On multivariate analysis, serum albumin was associated with overall survival. ES (HR=3.19; p=0.03) and high bilirubin levels (HR=1.11; p=0.003) were independently associated with treatment failure.
Conclusion: BBS is associated with longer efficacy than ES for treating cholestasis in advanced pancreatic cancer. However, the BBS is associated with prolonged ICU and hospital stays and higher demand for intensive care.
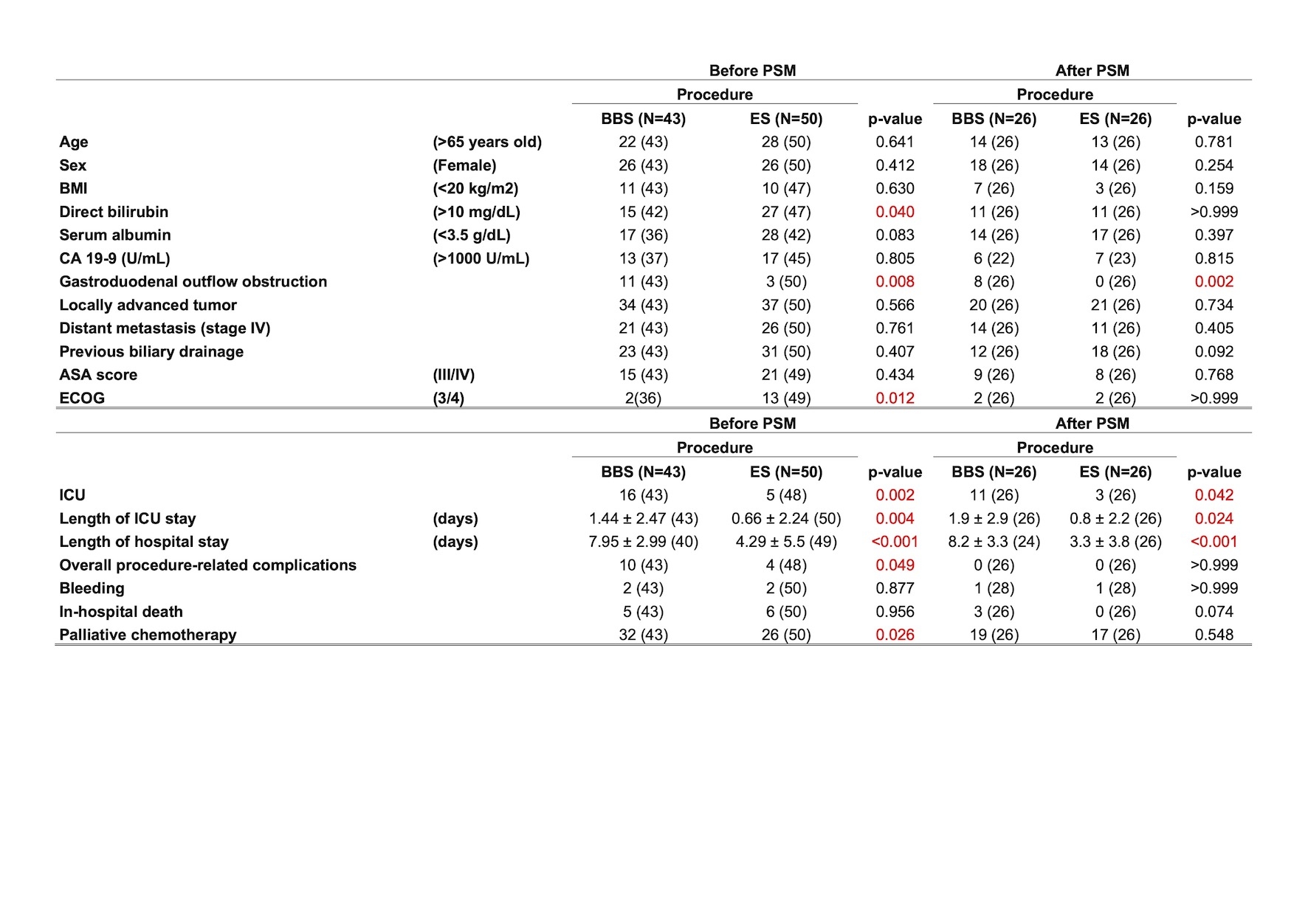
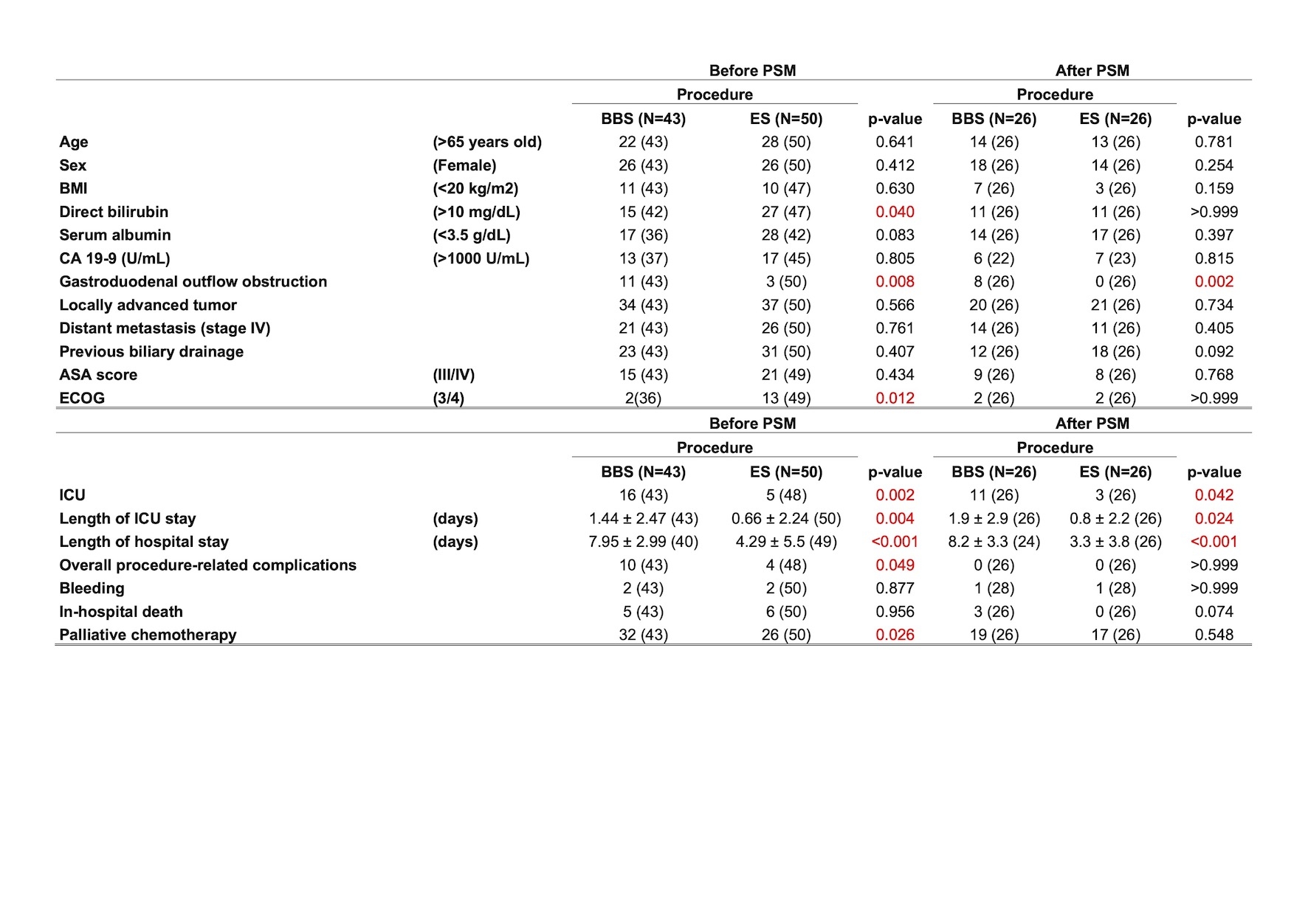
Comparison between the outcomes of the procedures bypass biliary surgery (BBS) and endoscopic stenting (ES) for cholestasis in pancreatic cancer patients. Results were presented before and after propensity score analysis (PSM). Red p-values show significant results (p<0.05)
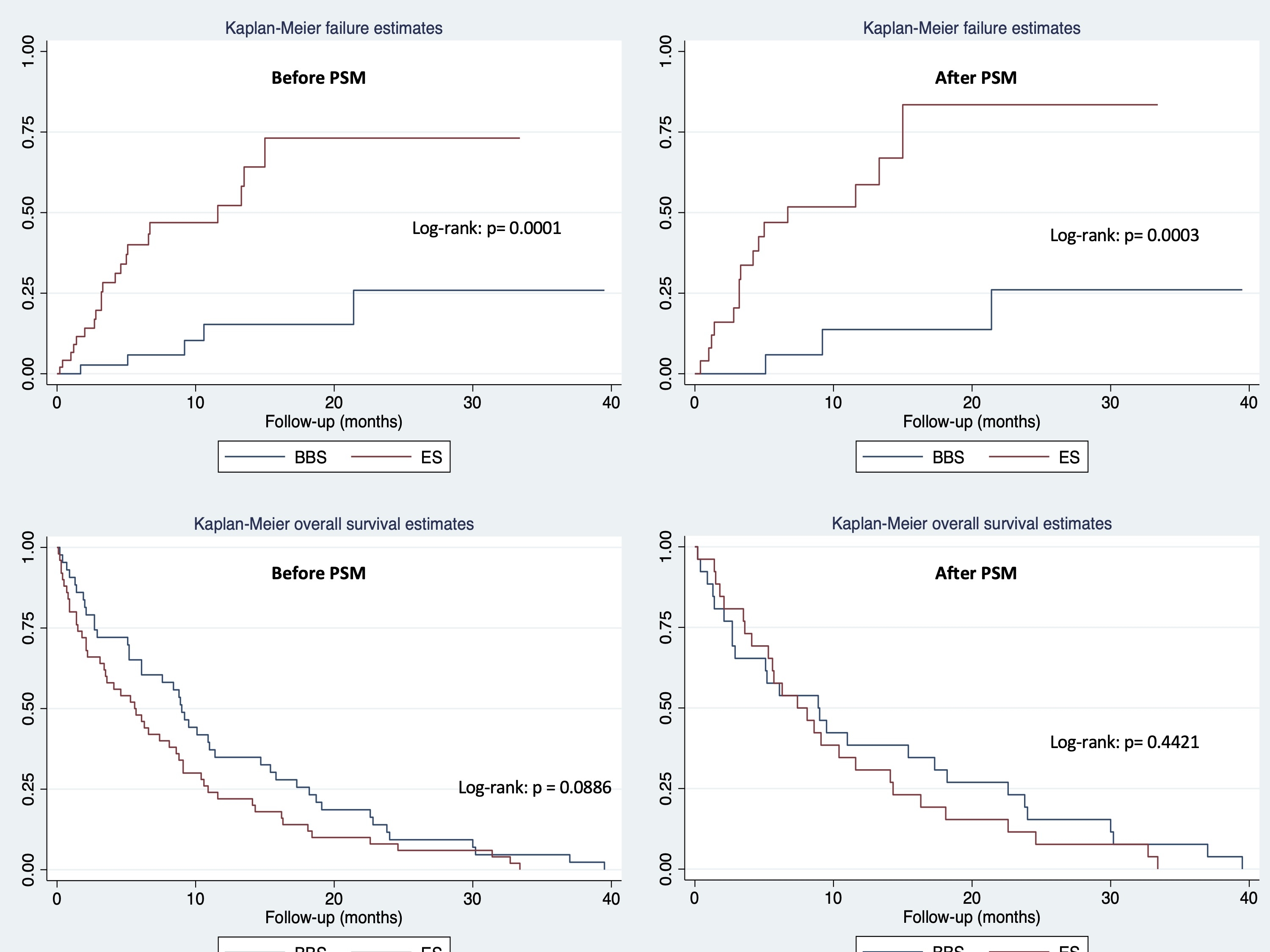
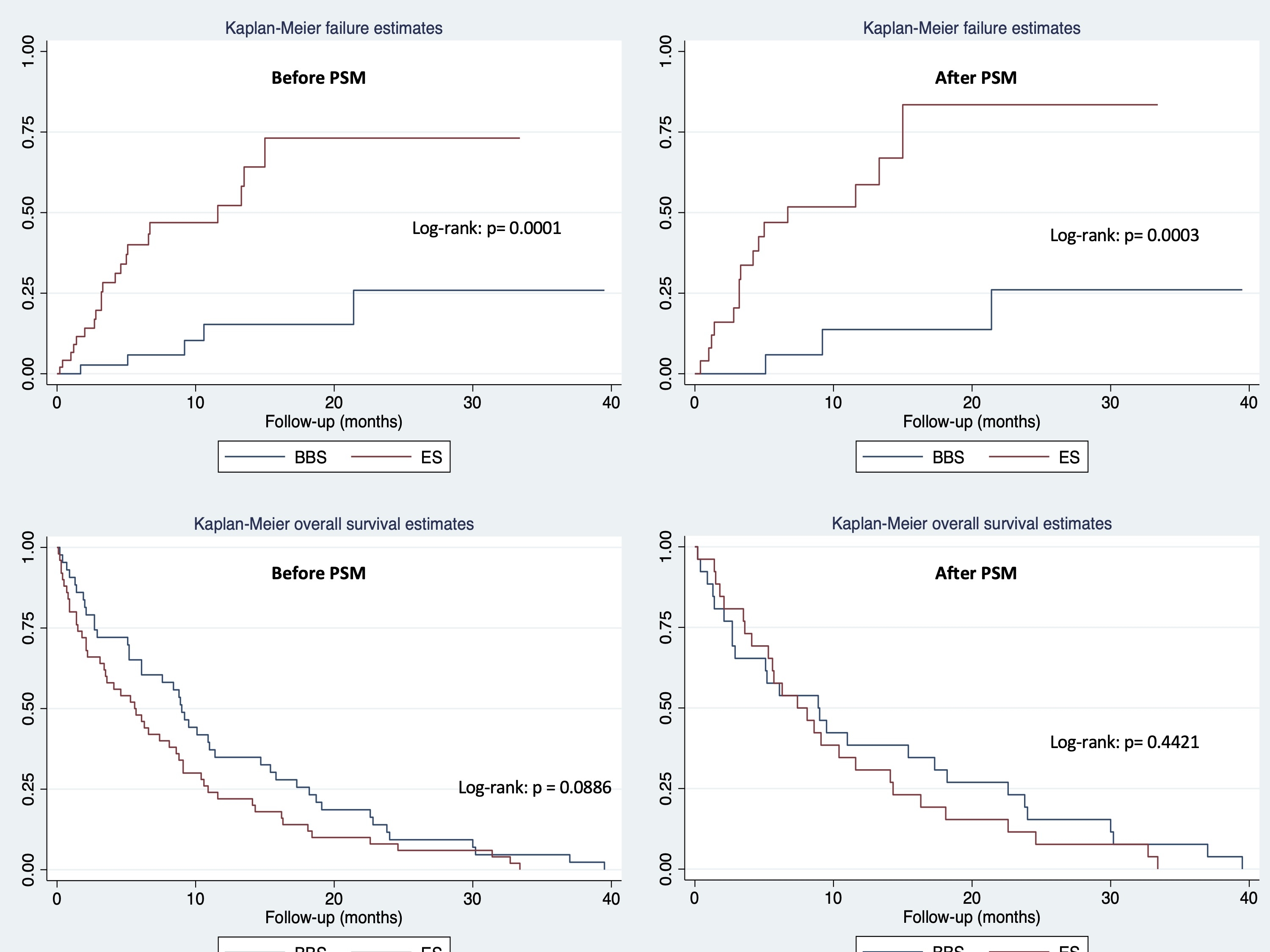
The upper graphs show the treatment failure for biliary bypass surgery (BBS) and endoscopic stenting (ES) before and after propensity score matching. We considered treatment failure as the need for hospital readmission due to biliary complications, such as cholestasis, cholangitis, and treatment of biliary complications. The bottom graphs show the overall survival Kaplan-Meier curves before and after propensity score matching.
Back to 2024 Abstracts