Back to 2024 Abstracts
DO PATIENT-REPORTED OUTCOMES DURING NEOADJUVANT THERAPY PREDICT POSTOPERATIVE COMPLICATIONS FOLLOWING SURGICAL RESECTION FOR GASTROINTESTINAL MALIGNANCIES?
Alexander H. Shannon
*, Samantha M. Ruff, Angela Sarna, Mary Dillhoff, Alex Kim, Emily Huang, Peter J. Kneuertz, Aslam Ejaz, Timothy M. Pawlik, Jordan Cloyd
Surgical Oncology, The Ohio State University Wexner Medical Center, Columbus, OH
Objectives: Neoadjuvant therapy (NT) is increasingly utilized prior to surgery for most gastrointestinal (GI) and hepatopancreatobiliary (HPB) malignancies. However, chemotherapy and radiation therapy can cause significant symptoms and a high incidence of adverse events. Whether patient-reported outcomes (PRO) or quality of life (QOL) during NT is predictive of postoperative complications following surgery is unknown.
Methods: A planned secondary analysis of a prospective cohort study of adult patients with GI (gastric, colorectal, esophageal) or HPB cancers who received NT and utilized a customized mobile phone application to measure in real-time patient-reported mood, symptoms, and free-text journaling as well as for monthly assessments of QOL using FACT-G (Functional Assessment of Cancer Therapy-General). Among patients who underwent surgery, the association between clinical, demographic, QOL, and PROs and postoperative Clavien-Dindo Grade ≥2 complications was analyzed using univariate analyses.
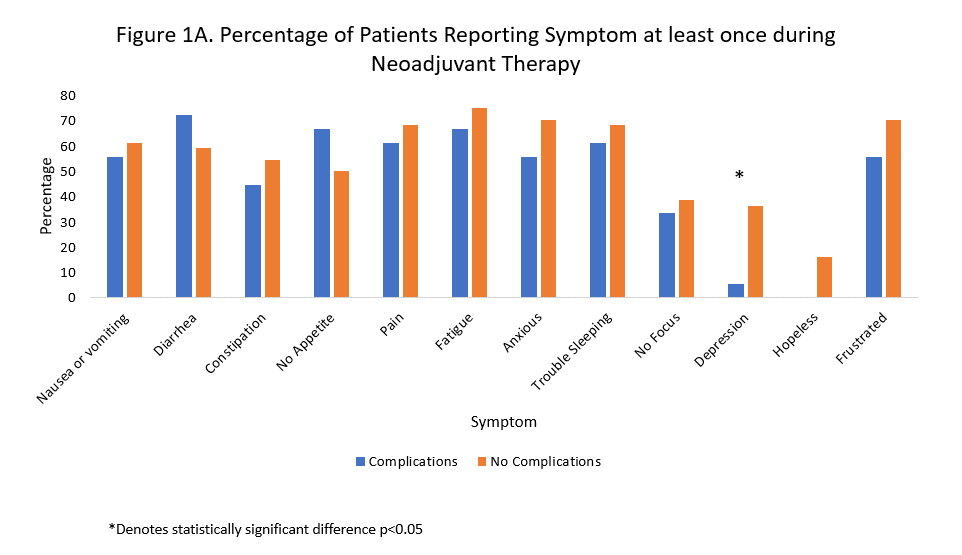
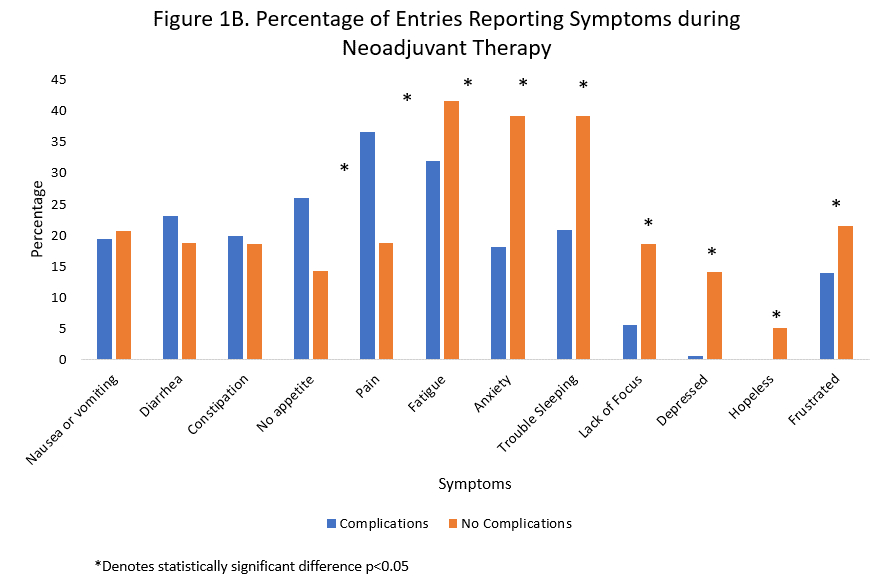
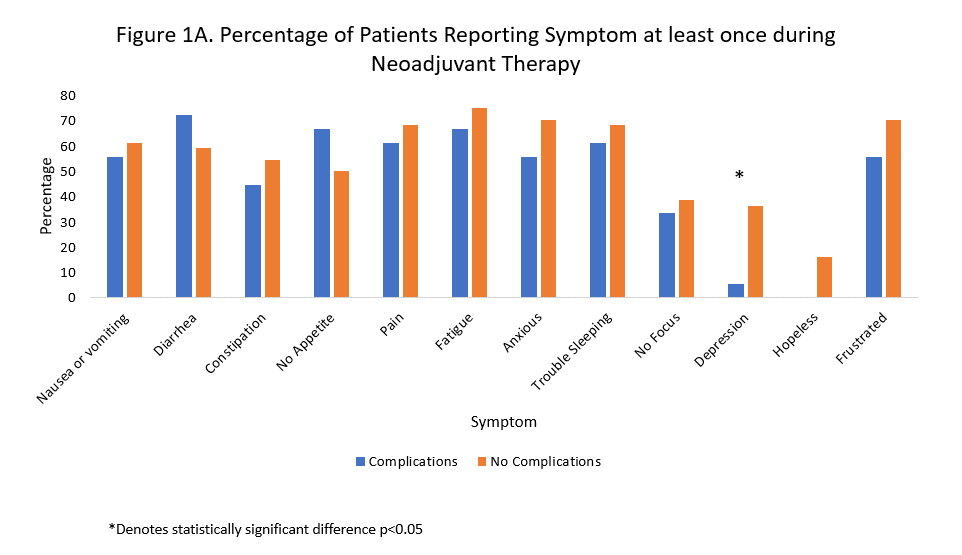
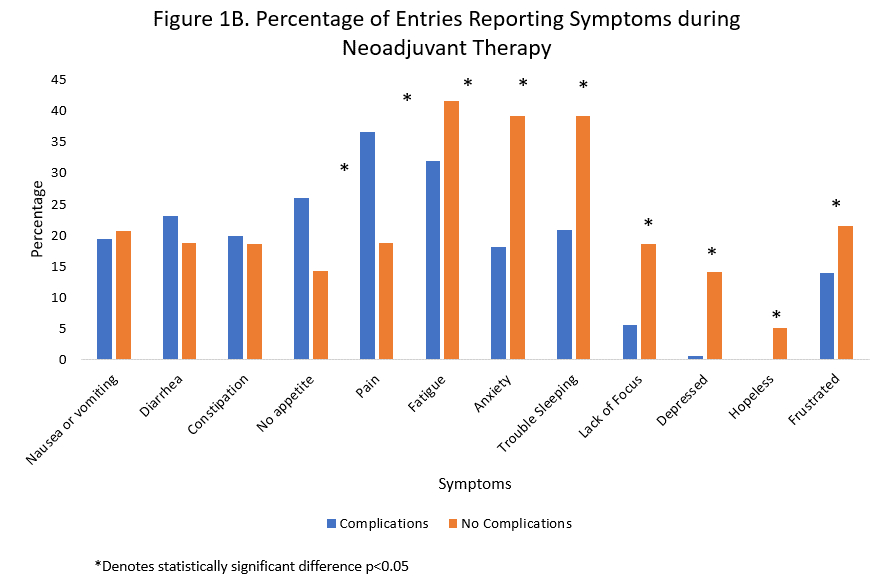
Results: Among 104 patients who enrolled in the prospective cohort study, 69 (66%) underwent surgery following NT of whom 20 (28.9%) experienced 30-day complications. There were no differences in baseline demographics, duration of NT, type of surgery performed, or cancer type between patients who did and did not have complications (all p>0.05). Patients who experienced postoperative complications were less engaged with the app during NT, submitting fewer PRO entries per person (mean 11.4 vs 19.6 entries). While few differences were observed in the proportion of patients who reported a symptom at least once during NT (Fig 1A), the proportion of all PRO entries positive for symptoms significantly differed between patients who did and did not experience complications (Fig 1B). For example, PRO entries of those who experienced complications were more likely to report pain and lack of appetite in real-time but less likely fatigue, anxiety, depression, and frustration. Baseline QOL scores at the start of NT (mean FACT-G 76.1 vs 75.2) and changes in QOL during NT did not differ between the two cohorts.
Conclusion: In this prospective cohort study measuring real-time PROs during NT for GI/HPB malignancies, both engagement with the smartphone app and specific patient-reported symptoms were associated with postoperative complications among those who underwent surgery. Further research is needed as to whether preoperative PROs can guide the need for patient-centered interventions aimed at mitigating postoperative complications following major cancer surgery.
Back to 2024 Abstracts