Back to 2024 Abstracts
NEOADJUVANT THERAPY REDUCES NODE POSITIVITY BUT DOES NOT CONFER SURVIVAL BENEFIT VERSUS UP-FRONT RESECTION FOR RESECTABLE INTRAHEPATIC CHOLANGIOCARCINOMA: A PROPENSITY-MATCHED ANALYSIS
Chase J. Wehrle
*, Jenny H. Chang, Kimberly P. Woo, Abby Gross, Robert Naples, Kathryn A. Stackhouse, Jaekeun J. Kim, Toms Augustin, Robert Simon, Daniel Joyce, Choon Hyuck David Kwon, R Matthew Walsh, Federico Aucejo, Samer A. Naffouje
Cleveland Clinic, Cleveland, OH
BackgroundIntrahepatic Cholangiocarcinoma (iCCA) is rare but deadly. Neoadjuvant systemic therapy (NAST) is frequently employed, though its' impact on short-term oncologic outcomes and/or survival remains relatively unknown.
MethodsThe National Cancer Database (NCDB) was queried for intrahepatic biliary malignancies between 2004 and 2019 was queried for patients with reportedly resectable (Stage I-IIIB) iCCA who received curative-intent resection with lymphadenectomy. Propensity matching was performed between groups based on the use of NAST and groups were compared on overall survival (OS) and oncologic outcomes such as nodal harvest, rate of node positivity, rate of positive margins, and completion of adjuvant therapy.
ResultsIn total, 2,596 patients met inclusion criteria; 1763 (68%) received NAST versus 364 (14%) up-front resection. After PSM, 364 pairs of patients were matched between NAST and no NAST. There were no differences after matching in age (p=0.358), sex (0.635), race (0.426), Charlson score (p=0.810), tumor size (0.582), CA19-9 at resection (p=0.442), T- (p=0.829) or N-stage (p=0.932), neoadjuvant radiation (p=0.398) or extent of hepatectomy (p=0.398).
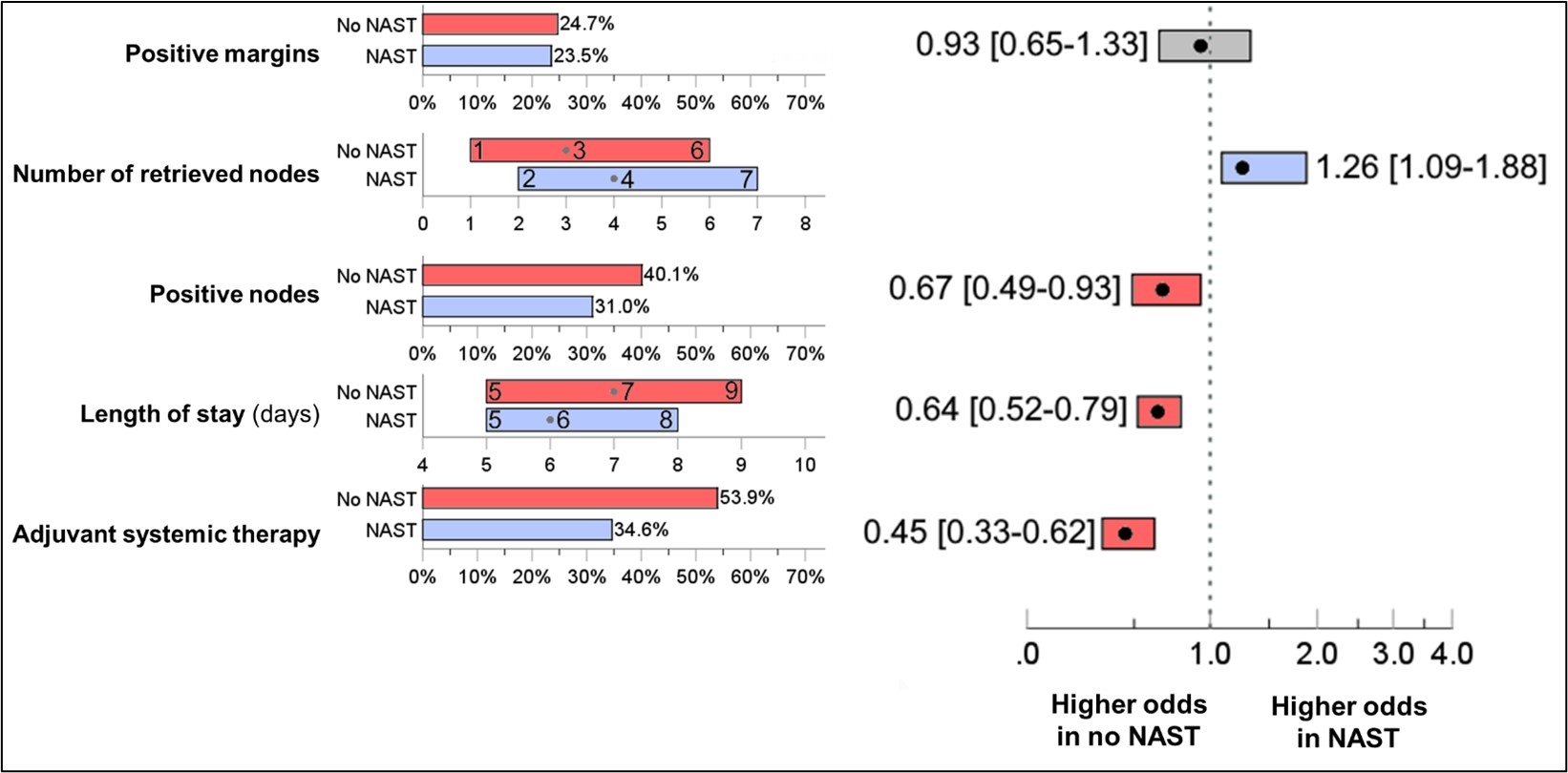
Patients receiving NAST had a greater nodal harvest (HR=1.26, 95%CI=1.09-1.88, p<0.001), but a lower rate of node positivity (HR=0.67, 0.49-0.63, p<0.001). Patients without NAST were more likely to complete adjuvant systemic therapy (HR=0.45, 0.33-0.62, p<0.001) [
Fig1].
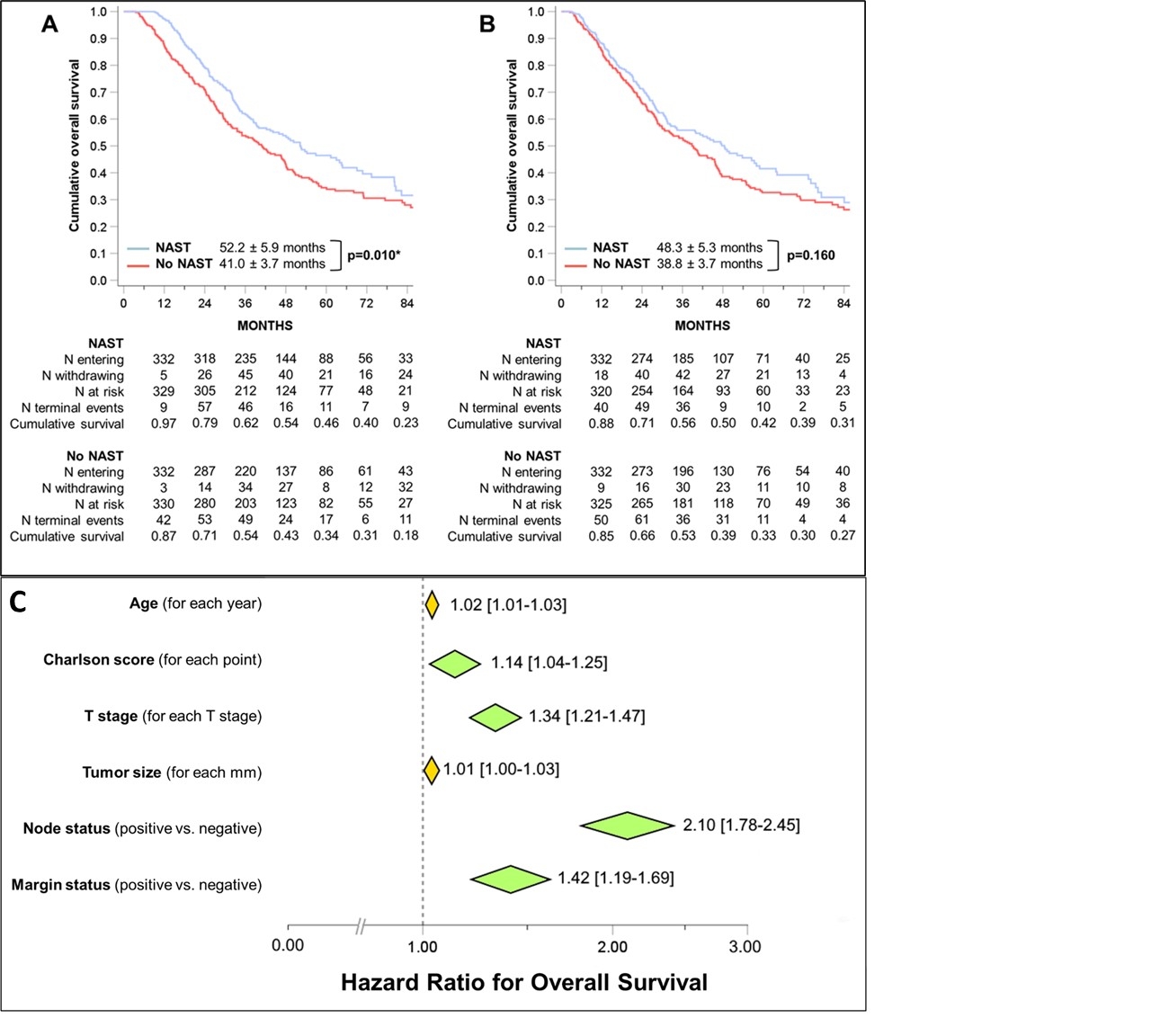
Patients receiving NAST had no survival benefit after resection versus those receiving NAST (Median OS=48.3vs28.8 months, p=0.160) [
Fig2]. Node-positive disease (HR=2.10, 1.78-2.45, p<0.001) conferred the greatest risk for reduced survival followed by R1-resection (HR=1.42, 1.21-1.47, p<0.001) and increasing T-stage (HR=1.34, 1.21-1.47, p<0.001).
DiscussionCurrent neoadjuvant systemic therapy for iCCA may help sterilize lymph nodes, but did not improve margin status or confer a survival benefit versus up-front resection. This may be due to greater completion of adjuvant systemic therapy in the no NAST group, indicating both groups were able to complete proper systemic treatment.
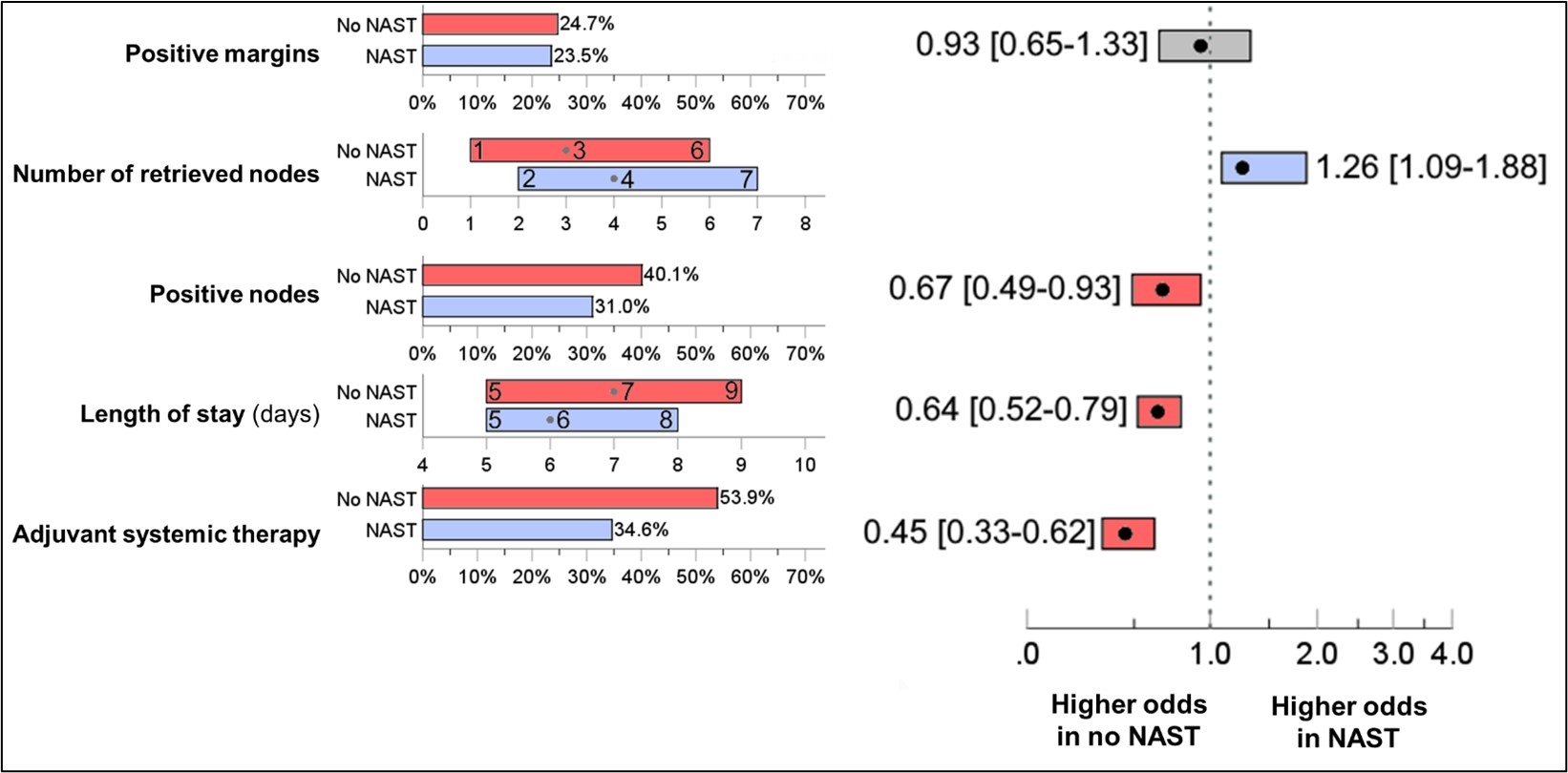 Figure 1
Figure 1: Short-term outcomes of intrahepatic cholangiocarcinoma patients who underwent NAST followed by surgical resection vs. upfront surgical resection in the matched groups.
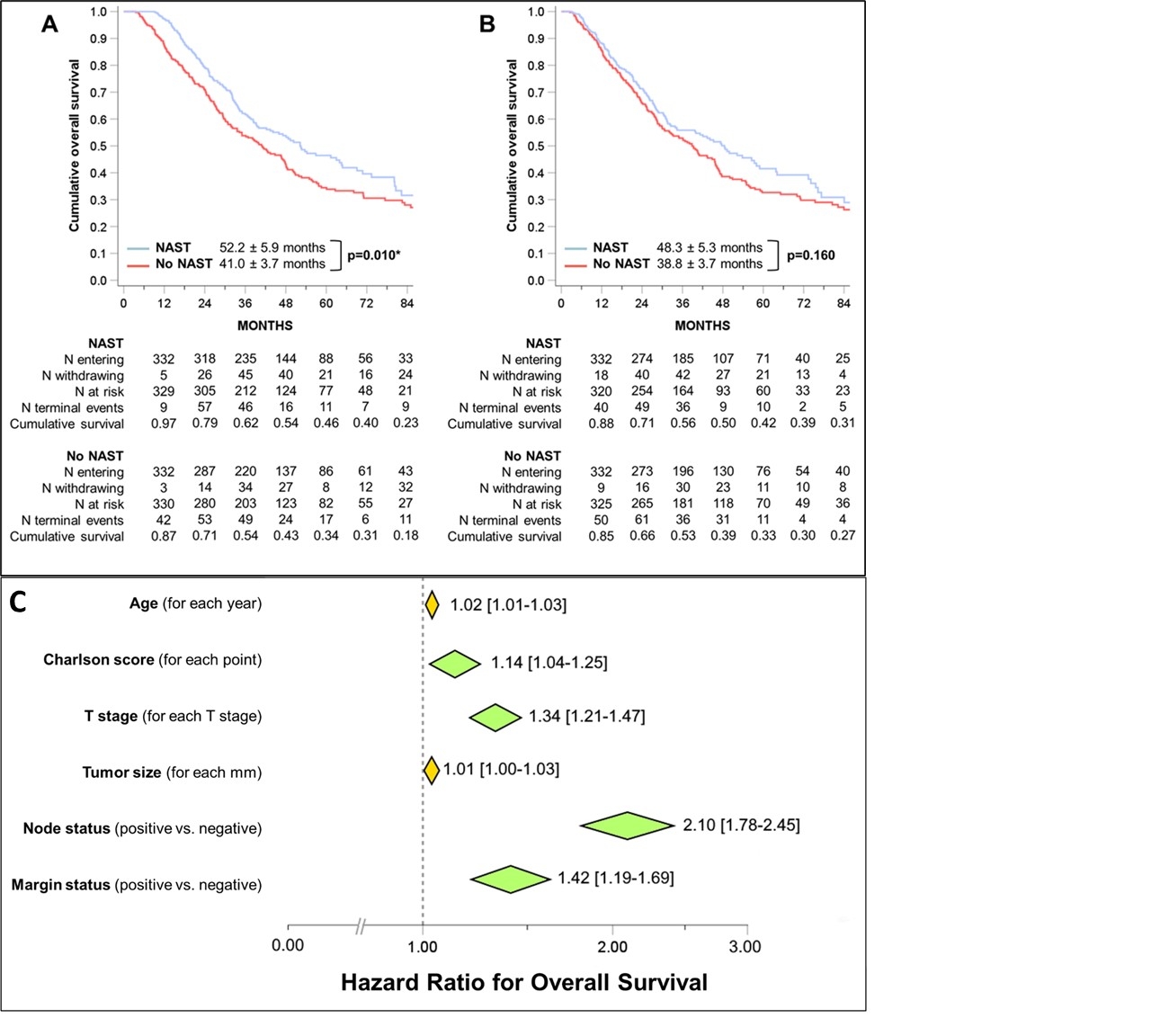 Figure 2
Figure 2:
A-B Kaplan Meier analysis comparing overall survival between intrahepatic cholangiocarcinoma patients who received NAST vs. those who received upfront surgical resection in the matched dataset. A) Overall survival as reported by NCDB from time of diagnosis. B) Overall survival after adjustment to time of definitive surgery.
C. Final block of the conditional backward Cox regression analysis for predictors of overall survival in the selected patient population.
Back to 2024 Abstracts