Back to 2024 Abstracts
SYSTEMATIC REVIEW OF THE POSTOPERATIVE OUTCOMES ASSOCIATED WITH LIVER TRANSPLANTATION FOR WILSON DISEASE
Austine Wang
*1, Tyler Mckechnie
1, Clarissa Ngo
1, Noor Bakir
2, Felipe Rodriguez
1, Justin Kang
1, Pablo E. Serrano
11McMaster University Faculty of Health Sciences, Hamilton, ON, Canada; 2University of Toronto Temerty Faculty of Medicine, Toronto, ON, Canada
IntroductionWilson Disease results in the accumulation of copper in hepatocyte lysosomes. In the setting of Wilson's Disease, liver transplant is indicated in cases of acute hepatic failure, advanced cirrhosis, and disease refractory to chelation therapy. While there are several observational studies evaluating liver transplantation for Wilson's Disease, there is no prior evidence synthesis. This study aims to systematically review overall morbidity, hepatic, neuropsychiatric and survival data following liver transplantation for Wilson disease.
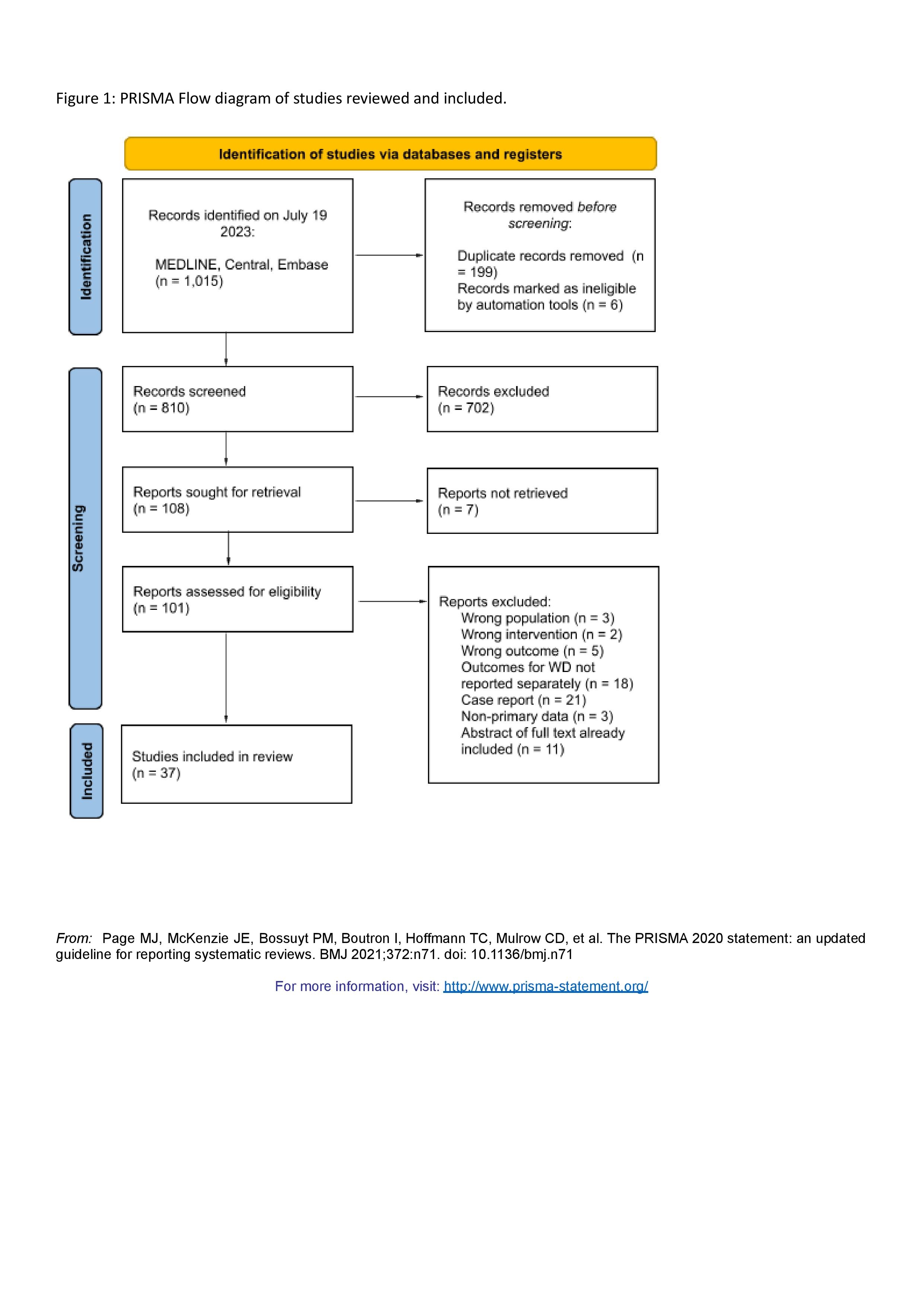
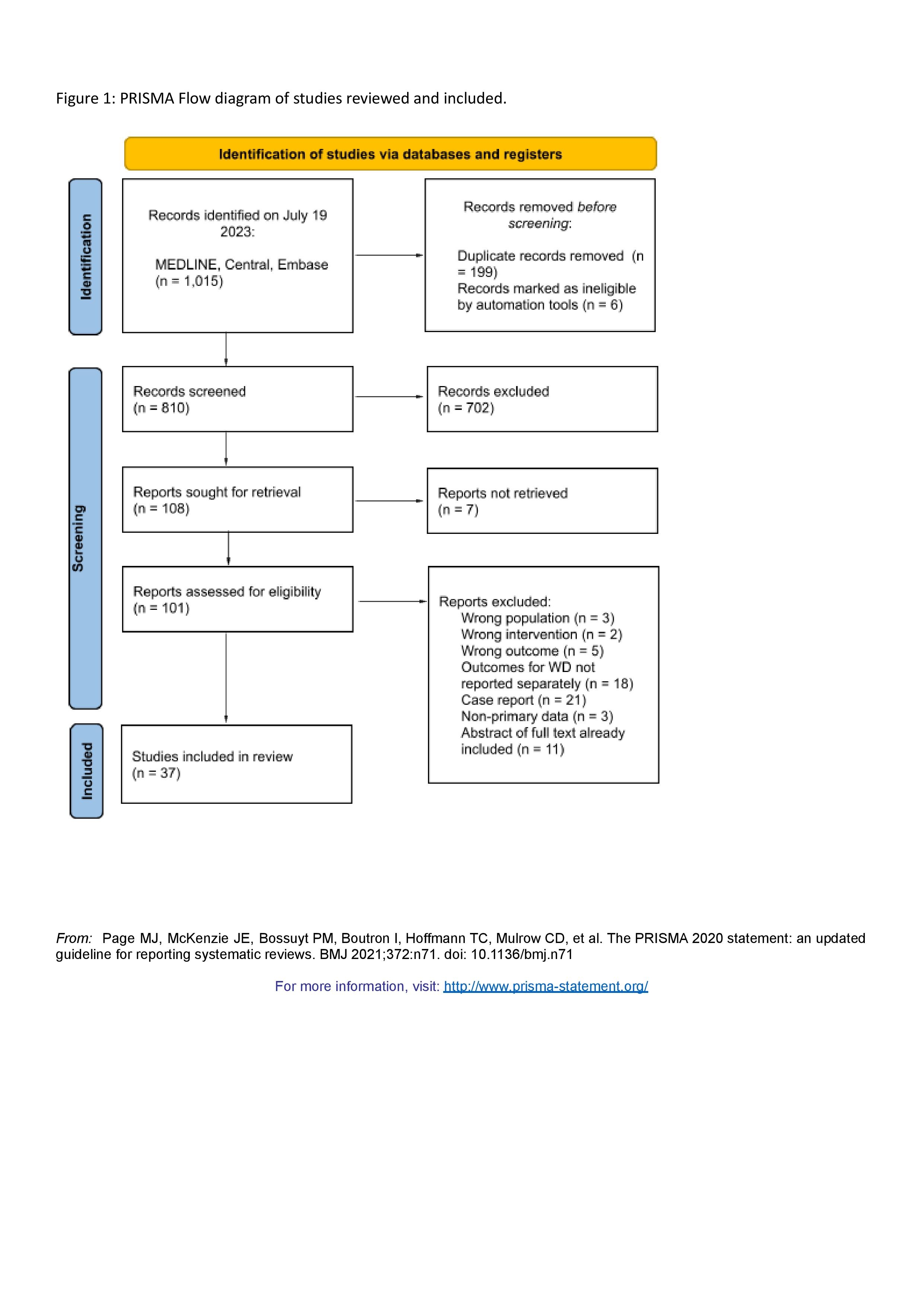
MethodsMEDLINE, Embase, Central were searched from inception to July 19 2023. Articles were eligible for inclusion if they evaluated patients undergoing any type of liver transplant for Wilson's Disease. The main outcomes were 30-day and 1-year mortality, postoperative outcomes including biopsy proven acute rejection, biliary strictures, hepatic artery thrombosis, intra-abdominal bleeding and infection; and neuropsychiatric changes. A systematic narrative summary was provided for each outcome. Risk of bias was assessed with the MINORS criteria.
ResultsAfter reviewing 1,015 relevant citations, 37 observational studies were included. The majority of studies were conducted in Asia (n=15) and Europe (n=15). Most patients presented with a hepatic or mixed hepatic and neurological form of Wilson disease. The most common indications for liver transplant include fulminant hepatic failure, and chronic liver failure, including decompensated cirrhosis. The 30-day mortality rate ranged between 0.00% to 71.4% in 21 studies reporting on this outcome, with all but 1 study reporting a <16.0% 30 day mortality rate mortality rate. The 1-year mortality rate ranged between 0.00% to 85.7%. The most commonly reported morbidity outcomes by studies include biopsy proven acute rejection (n=13), biliary strictures (n=13), primary nonfunction (n=12), hepatic artery thrombosis (n=16), intra abdominal bleeding (n=7), and infection (n=18). The incidences of these outcomes are described in Table 1. 29 studies reported on neurological or psychiatric outcomes after hepatic transplant. A high degree of heterogeneity in the outcomes reported and the extent to which they were reported was found. Two studies used objective measures, including the MMSE and UWDRS to report on changes. The mean MINORS score for risk of bias for all studies was 8.19 (2.12).
ConclusionThe current body of literature pertaining to hepatic transplantation for Wilson's Disease is limited to relatively small, observational studies. These studies, while demonstrating acceptable postoperative morbidity and mortality, are heterogenous and at high risk of bias. Adherence to high-quality observational methodology and homogenous reporting will be necessary for advances in the field, as Wilson Disease is a rare indication for liver transplant precluding interventional trials.
Back to 2024 Abstracts