Back to 2024 Abstracts
PREOPERATIVE PSYCHOSOCIAL RISK BURDEN AMONG PATIENTS UNDEROING MAJOR THORACIC AND ABDOMINAL SURGERY
Emily Park, Kurt Schultz, Haddon Pantel, Anne Mongiu, Vikram Reddy, Ira Leeds
*Surgery, Yale School of Medicine, New Haven, CT
Background: Psychosocial risk factors (PSRFs) negatively impact surgical outcomes but their prevalence in surgical patient populations is not well described. The purpose of this study was to characterize differences in the PSRF burden in patients undergoing major surgery by patient demographic groups.
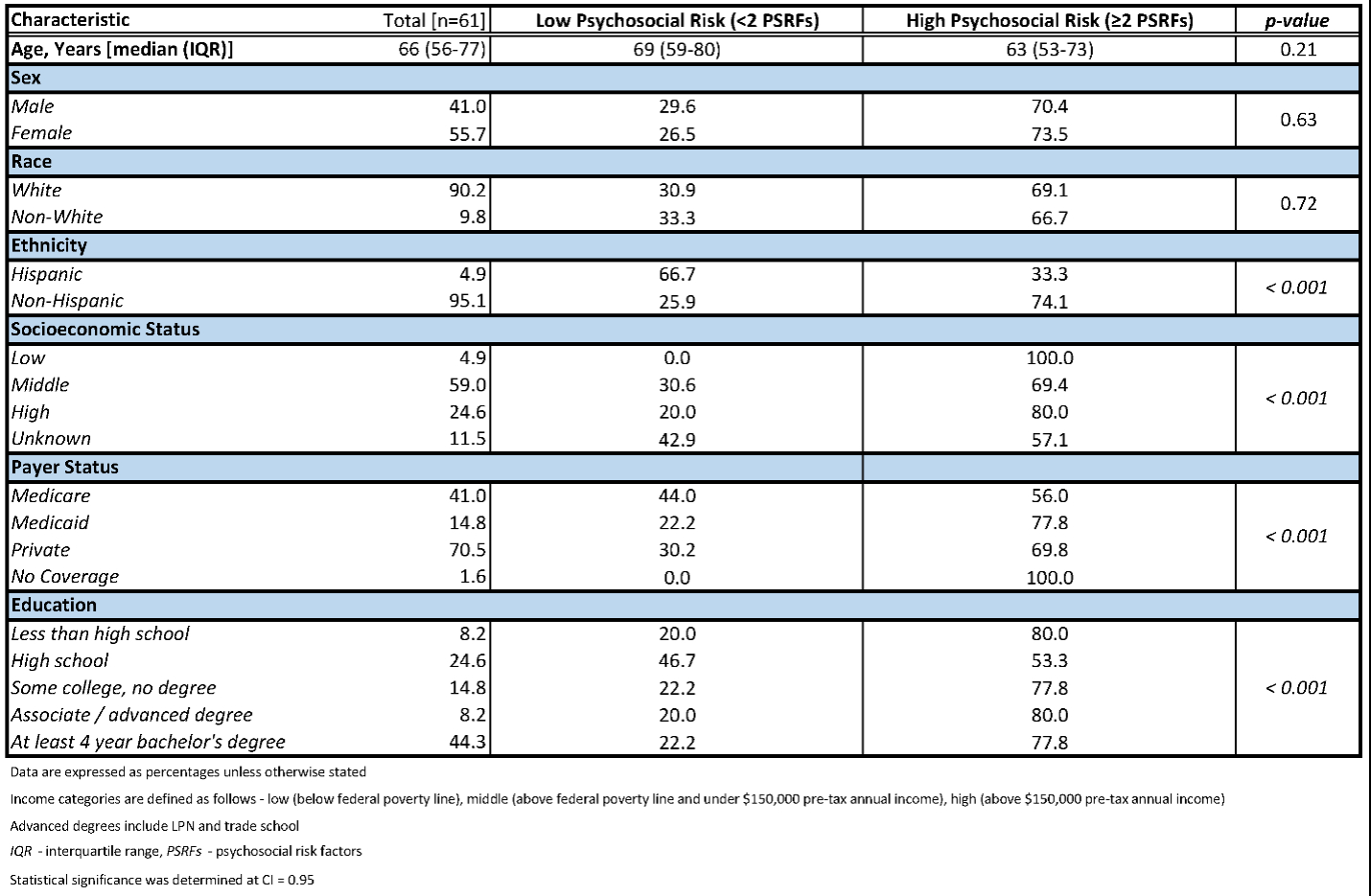
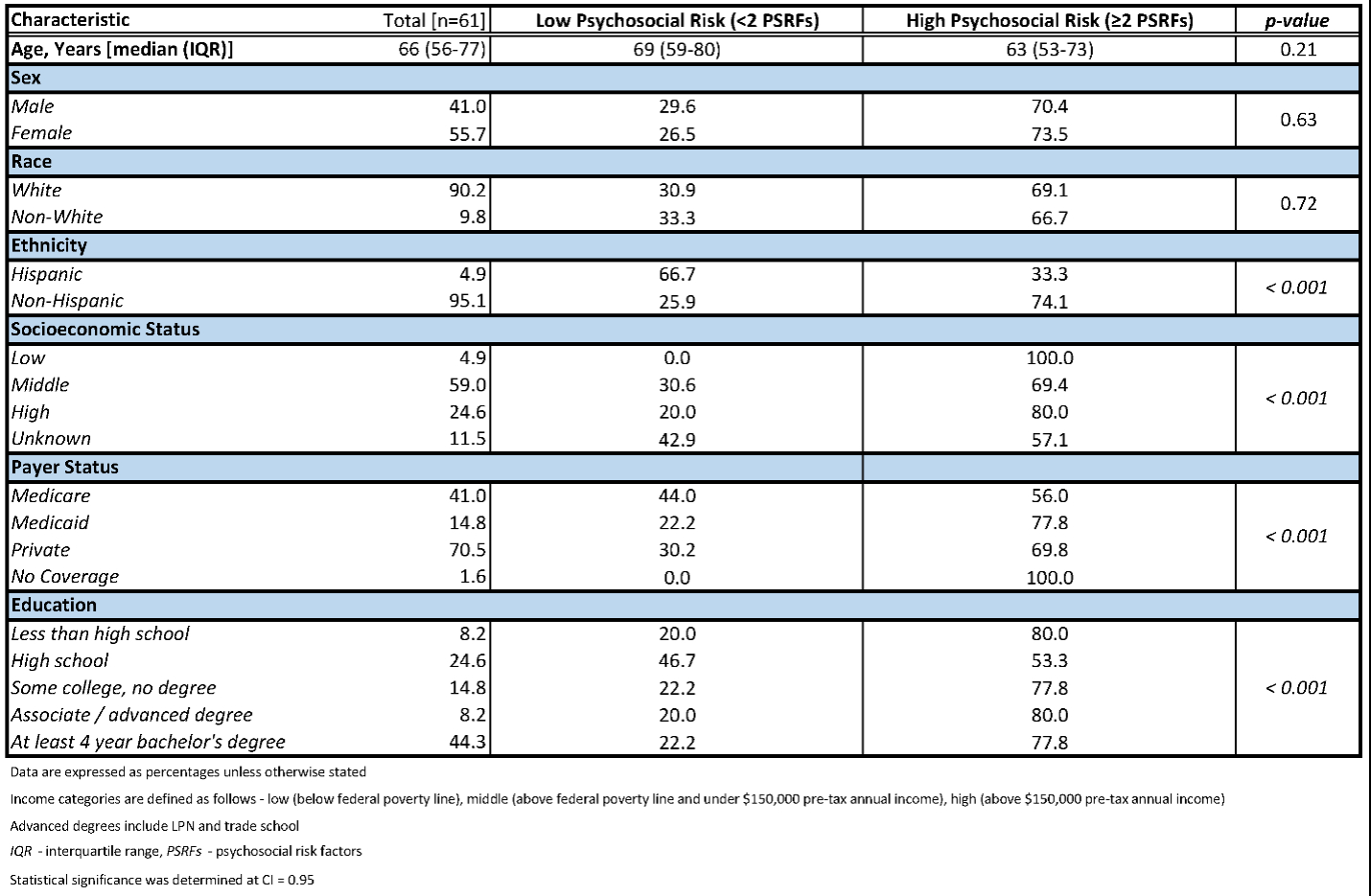
Methods: We conducted a prospective PSRF risk assessment of adult patients undergoing major thoracic and abdominal elective surgery at a multi-site, regional academic health system from July 2023 to November 2023. We used a telephone-delivered, comprehensive patient questionnaire, comprised of validated survey instruments for anxiety, depression, addiction, high-risk alcohol use, smoking history, resilience, self-efficacy, and social determinants of health. High psychosocial risk was defined as two or more PSRFs. Categorical variables were compared with a Chi-square test, and continuous variables were compared with two tailed t-test.
Results: Of 61 surgical patients interviewed preoperatively, 25 (41%) had anxiety, 27 (44.3%) had depression, 7 (11.5%) had addiction, 24 (39.3%) had high-risk alcohol use, 34 (55.7%) had a smoking history, 24 (39.3%) had low resilience, and 2 (3.3%) had low resourcefulness. Patients were majority white (90.2%), non-Hispanic (95.1%), privately insured (70.5%), college-educated (44.3%), of middle socioeconomic status (SES) (59.0%), and female (55.7%). 44 (72.1%) patients had high psychosocial risk, with increased prevalence in non-white (80.0% vs 71.4%, p<0.001) and low SES (p<0.001) individuals. Anxiety was most prevalent in those who were non-white (60% vs 39.3%, p<0.001), high school-educated (p<0.001), and of low SES (p<0.001). Similarly, non-white (80.0% vs 41.1%, p<0.001) patients and those of low SES (p<0.05) were more likely to have depression. High risk alcohol use was significantly more prevalent in white (41.1% vs 20.0%, p<0.001), college-educated (p<0.05), and high SES (p<0.001) patients. Non-white (39.2% vs 45.7%, p<0.001) and low SES (p<0.001) patients were more likely to have a history of smoking. History of addiction was associated with being nonwhite (20.0% vs 10.7%, p=0.05). Low resilience was most prevalent in individuals with low SES (p<0.001). Demographic groups were not statistically different in self-efficacy.
Conclusion: More than two-thirds of patients undergoing major surgery at a tertiary academic center have multiple PSRFs. Most PSRFs were disproportionally present in traditionally vulnerable populations undergoing major surgery, although high risk alcohol use was more common in high SES patients. Next steps include investigating whether comprehensive PSRF assessments better explain disparities in surgical outcomes compared to conventional proxies for psychosocial risk, such as payer status and race.
Back to 2024 Abstracts