Back to 2024 Abstracts
THE ASSOCIATION OF SOCIAL VULNERABILITY INDEX AND COLORECTAL CANCER SCREENING RATE IN THE US
Alfonsus Adrian H. Harsono
*1, Lauren Wood
1, Bayley Jones
1,2, Wendelyn Oslock
1,6, Nathan C. English
1,3, Joshua Richman
1, Chandler McLeod
1, Patricia Ajayi-Fox
4, Ayesiga Herman
5, Daniel I. Chu
11Department of Surgery, Div. of Gastrointestinal Surgery, The University of Alabama at Birmingham Department of Surgery, Birmingham, AL; 2The University of Texas Southwestern Medical Center Department of Surgery, Dallas, TX; 3University of Cape Town Department of Surgery, Cape Town, Western Cape, South Africa; 4The University of Alabama at Birmingham Department of Medicine, Birmingham, AL; 5Kilimanjaro Christian Medical Centre, Moshi, Kilimanjaro, Tanzania, United Republic of; 6Birmingham Veterans Affair Medical Center, Birmingham, AL
Introduction Despite advancements in colorectal cancer (CRC) treatment modalities, screening remains pivotal in prevention, improving patient outcomes, and reducing burdens of the disease. However, screening rates remain below target. Many factors contribute to this, including the socioecological determinants of health (SEDOHs). Therefore, we aimed to study the association of SEDOHs with CRC screening rates in the United States using the multi-dimensional measure of social vulnerability index (SVI)
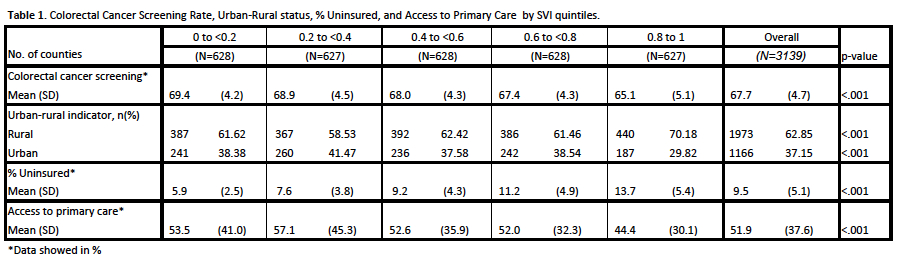
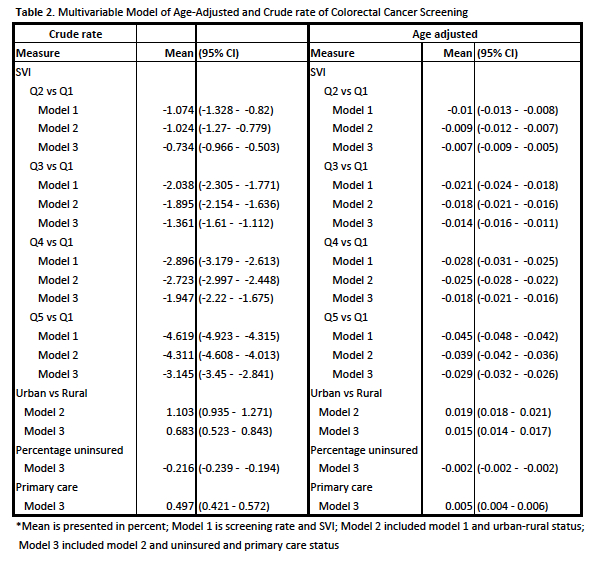
Methods This is a cross-sectional study using county-based national data retrieved from the Centers for Disease Control and Prevention (CDC) SVI, CDC PLACES, and Health Resource & Service Administration (HRSA) Area Health Resource Files (AHRF) databases. SVI values range from 0-1 (least to most vulnerable) and are categorized into quintiles (Q1-Q5). CDC Places provides 29 chronic diseases health data for small areas across the country, which includes CRC screening rate. HRSA AHRF database provides covariates analyzed: urban-rural indicators, percentage of uninsured people, and access to primary care. The outcome was the CRC screening rate among adults aged 50-75 years. Bivariate analysis was conducted using the Chi-square and Kruskal-Wallis rank sum tests. Linear regression modeling was performed adjusting for urban-rural, insurance, and primary care status in order to find the predictive value of SVI on CRC screening rate.
Results A total of 3139 counties were analyzed, of which 1973 (62.9%) were classified as rural. The mean county-level CRC screening rate was 67.7% and ranged from 50.l% to 83.1%. CRC screening rates decreased with increasing SVI (69.4% vs 65.1% for Q1 and Q5 respectively, p<0.001). Regression results found SVI quintiles to be significantly associated with both crude and age-adjusted CRC screening rates. These associations remained significant after adjusting for rurality, insurance status, and primary care access.
Conclusion Higher SVI is associated with lower CRC screening rates nationally even after controlling for rurality, access to primary care, and insurance coverage. This points to additional barriers within vulnerable communities that must be overcome to increase CRC screening and thus improve outcomes.
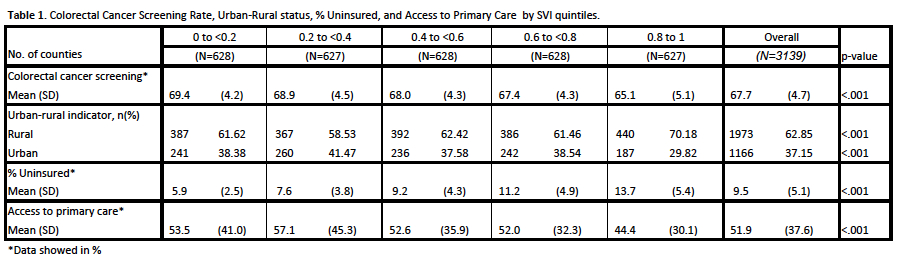
Table 1. Colorectal Cancer Screening Rate, Urban-Rural status, % Uninsured, and Access to Primary Care by SVI quintiles.
*Data showed in %
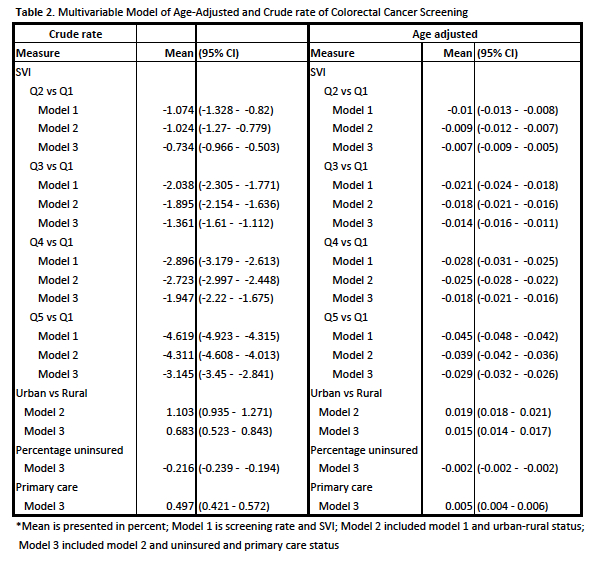
Table 2. Multivariable Model of Age-Adjusted and Crude rate of Colorectal Cancer Screening.
*Mean is presented in percent; Model 1 is screening rate and SVI; Model 2 included model 1 and urban-rural status; Model 3 included model 2 and uninsured and primary care status
Back to 2024 Abstracts