Back to 2024 Abstracts
PROVIDERS' AND SURVIVORS' PERSPECTIVES ON THE AVAILABILITY AND ACCESSIBILITY OF SURGERY IN GASTROINTESTINAL CANCER CARE
Nathan C. English
*1,2, Nataliya Ivankova
2, Burke Smith
2, Bayley Jones
3,2, Ivan I. iherbey
2, Brendan Rosamond
4, Wendelyn Oslock
2, Yu-Mei Schoenberger
2, Maria Pisu
2, Daniel I. Chu
21University of Cape Town, Cape Town, Western Cape, South Africa; 2The University of Alabama at Birmingham, Birmingham, AL; 3The University of Texas Southwestern Medical Center, Dallas, TX; 4University of Houston, Houston, TX
Introduction Surgery is an essential component of the multidisciplinary approach to gastrointestinal (GI) cancer treatment. Many patients do not have access to the surgical care that optimizes cancer outcomes. Scarce availability and/or low accessibility of the appropriate medical resources may explain why, especially in economically disadvantaged areas of the US Deep South. This study aimed to investigate both providers' and GI cancer survivors' perspectives on barriers and facilitators related to the availability and accessibility of surgical care.
MethodsWe conducted semi-structured interviews with a purposively selected group of multidisciplinary GI cancer providers and survivors in Alabama and Mississippi, two states in the US Deep South. Survivors were within 3 years of diagnosis of stage I-III esophageal, pancreatic, or colorectal cancer. Interview guides, informed by surgical disparities and access to care conceptual frameworks, were developed to elucidate factors related to availability and accessibility of surgical care. Interviews were recorded, transcribed, and analyzed by three co-authors using inductive thematic and content analysis qualitative techniques with NVivo 12.6 Plus software. Intercoder agreement was reached at 90%.
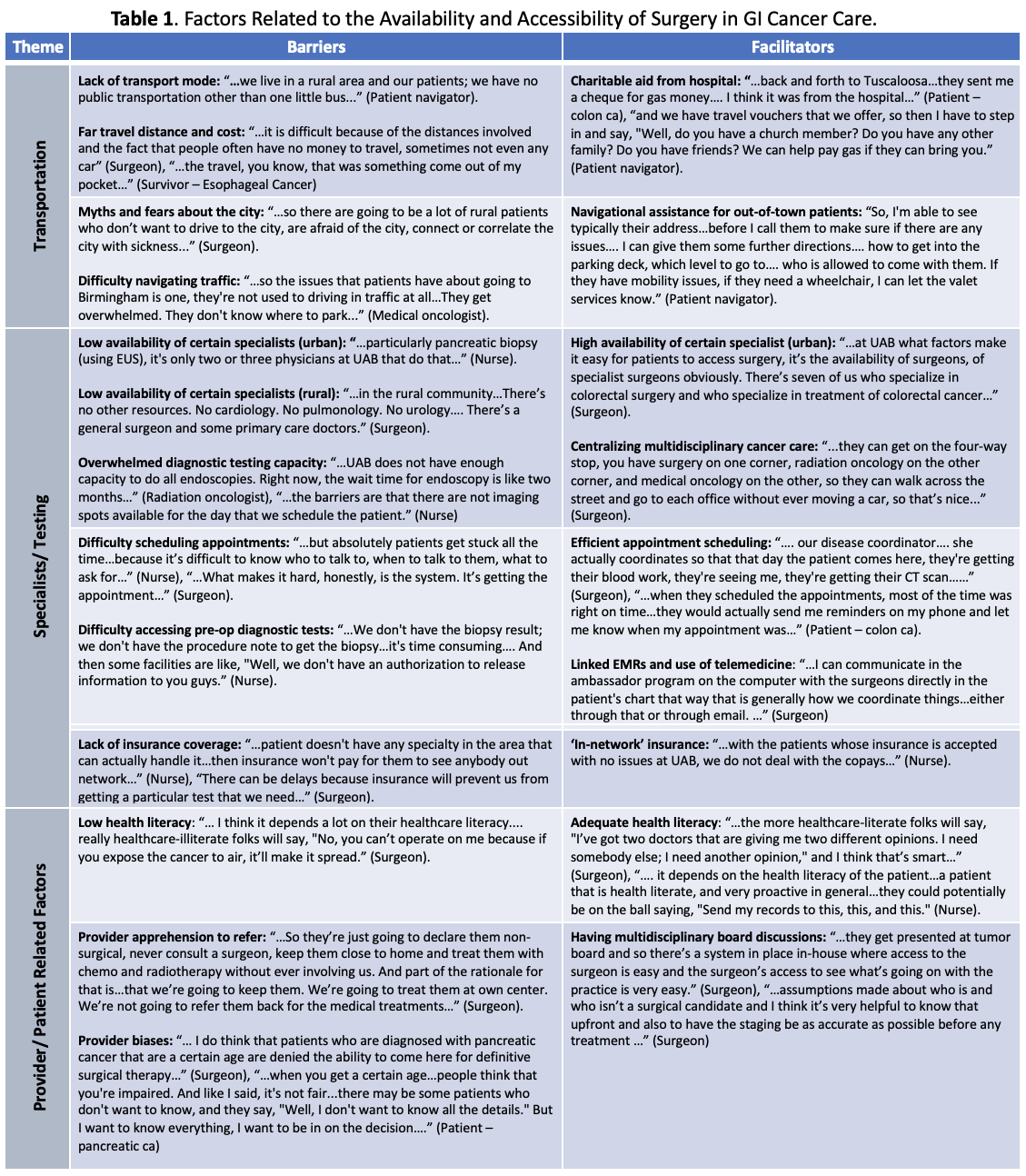
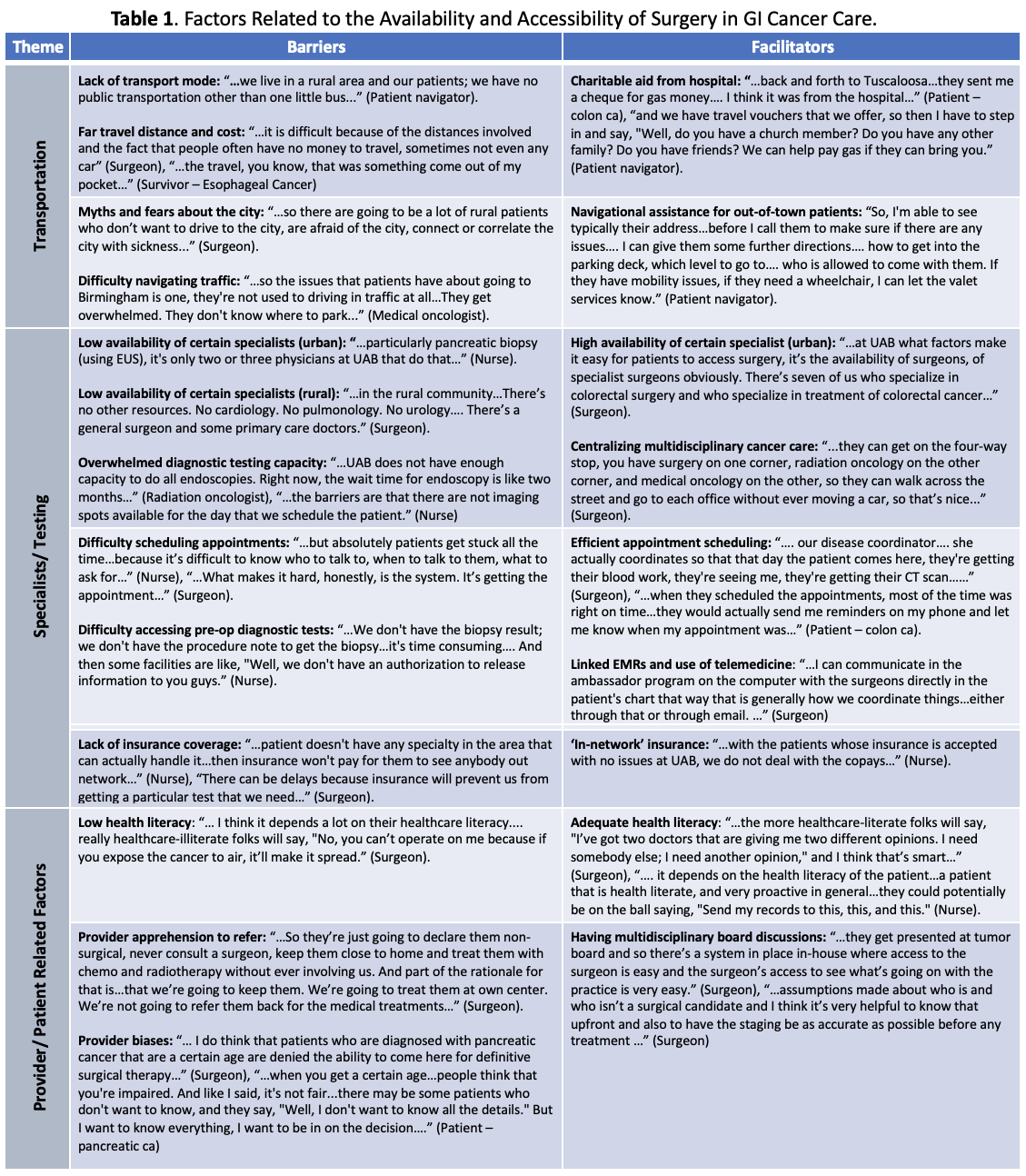
Results The 27 providers included surgeons (n=11), medical oncologists (n=2), radiation oncologists (n=2), a primary care physician (n=1), nurses (n=8) and patient navigators (n=3). Of 36 survivors, 21 (58.3%) were male, 30.6% identified as Black race, and ages ranged from 44-87 years. Identified barriers and facilitators were categorized into three main themes: transportation, specialists/testing, and provider/patient related factors
(Table 1). Barriers to availability and accessibility in surgery included a lack and cost of transportation, or reluctance to travel due to uneasiness with urban centers, low availability of specialized care in both urban and rural settings, overburdened referral centers, provider biases regarding referral for surgery, and low health literacy. Facilitators to surgical care included availability of charitable aid, centralizing multidisciplinary care, and adopting efficient appointment scheduling practices.
Conclusions In the Deep South, barriers and facilitators related to availability and accessibility of GI surgical cancer care were identified at the health system, provider, and patient level especially for patients from rural areas. These data suggest targets for improving availability and accessibility of surgery in GI cancer care.
Back to 2024 Abstracts