Back to 2024 Abstracts
HIGH RISK RURAL SURGICAL PATIENTS AND POOR ACCESS TO ELECTIVE COLORECTAL CANCER SURGERY: INSIGHT FOR MULTI-LEVEL INTERVENTION FOR RURAL AMERICA
Yanick Tade
*1, Jillian Timperley
1, Danielle B. Dilsaver
1, Emily Brown
1, Nicole deRosa
1, Waddah Al-Refaie
1,21Surgery, Creighton University School of Medicine, Omaha, NE; 2CHI Health, Omaha, NE
Introduction:Cancer mortality is one of the leading causes of death in rural America, in part, due to poor access to screening. Rural dwellers are large and heterogeneous; yet patient-related drivers of long-standing inequities in surgical access are under-studied. Undergoing elective colorectal cancer (CRC) surgery is crucial to reduce risks of operative complications and mortality. This US population-based study aims to identify patient-level factors associated of poor access to elective CRC surgery among rural dwellers in America.
Methods: A rigorous evaluation of the Policy Map and Census Bureau was performed to identify factors associated with poor surgical access in the top 20 states by rural population. To assess whether these factors were associated with poor access to elective CRC surgery, hospitalization data on rural patients undergoing CRC surgery were abstracted from the 2007-2020 National Inpatient Sample. Rural was defined as patients residing in counties with a population < 250,000. Multivariable logistic regression models were estimated to assess whether the identified patient- and hospital-level factors were associated with receipt of elective CRC surgery. Patient- and hospital-level factor interactions were specified a priori.
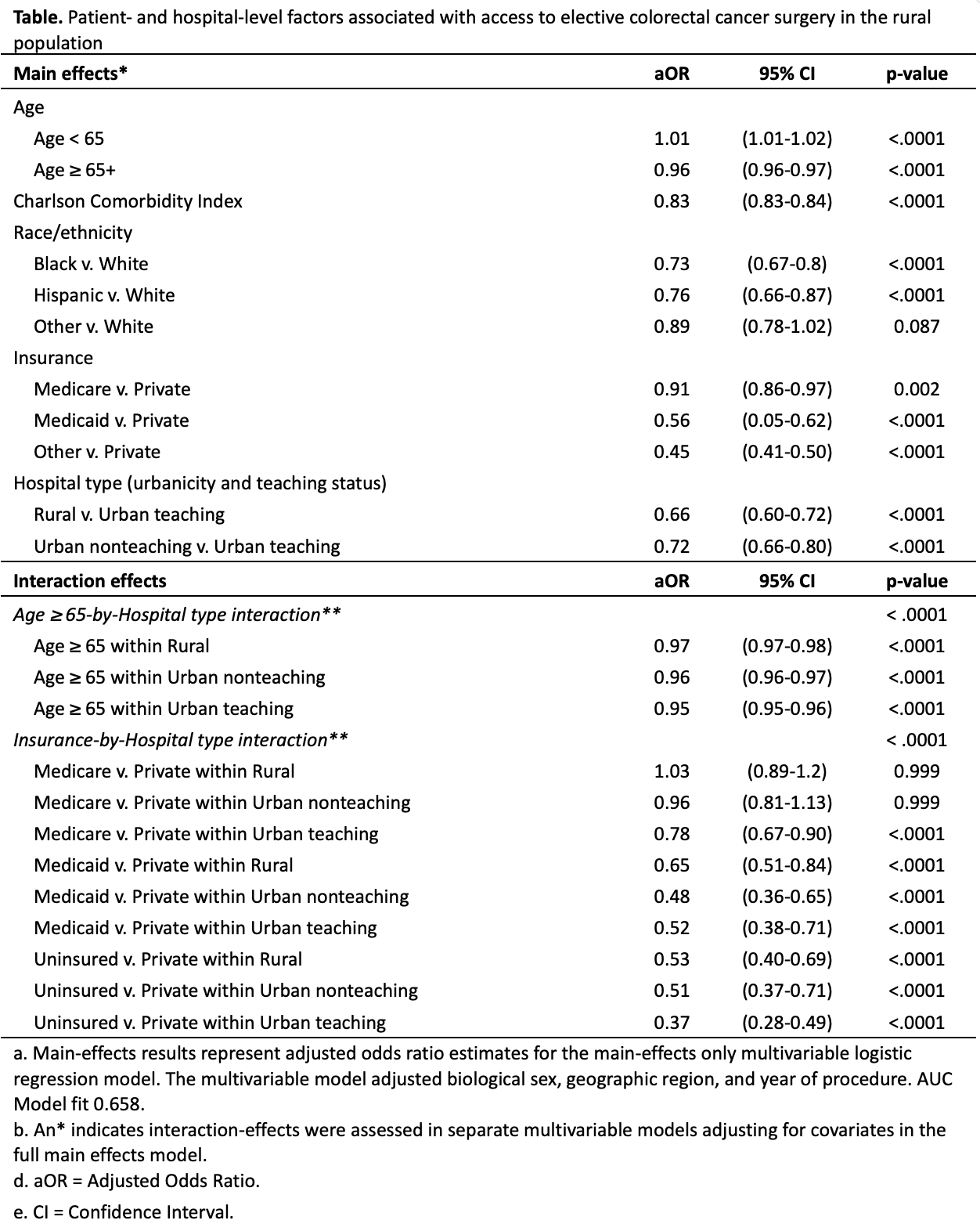
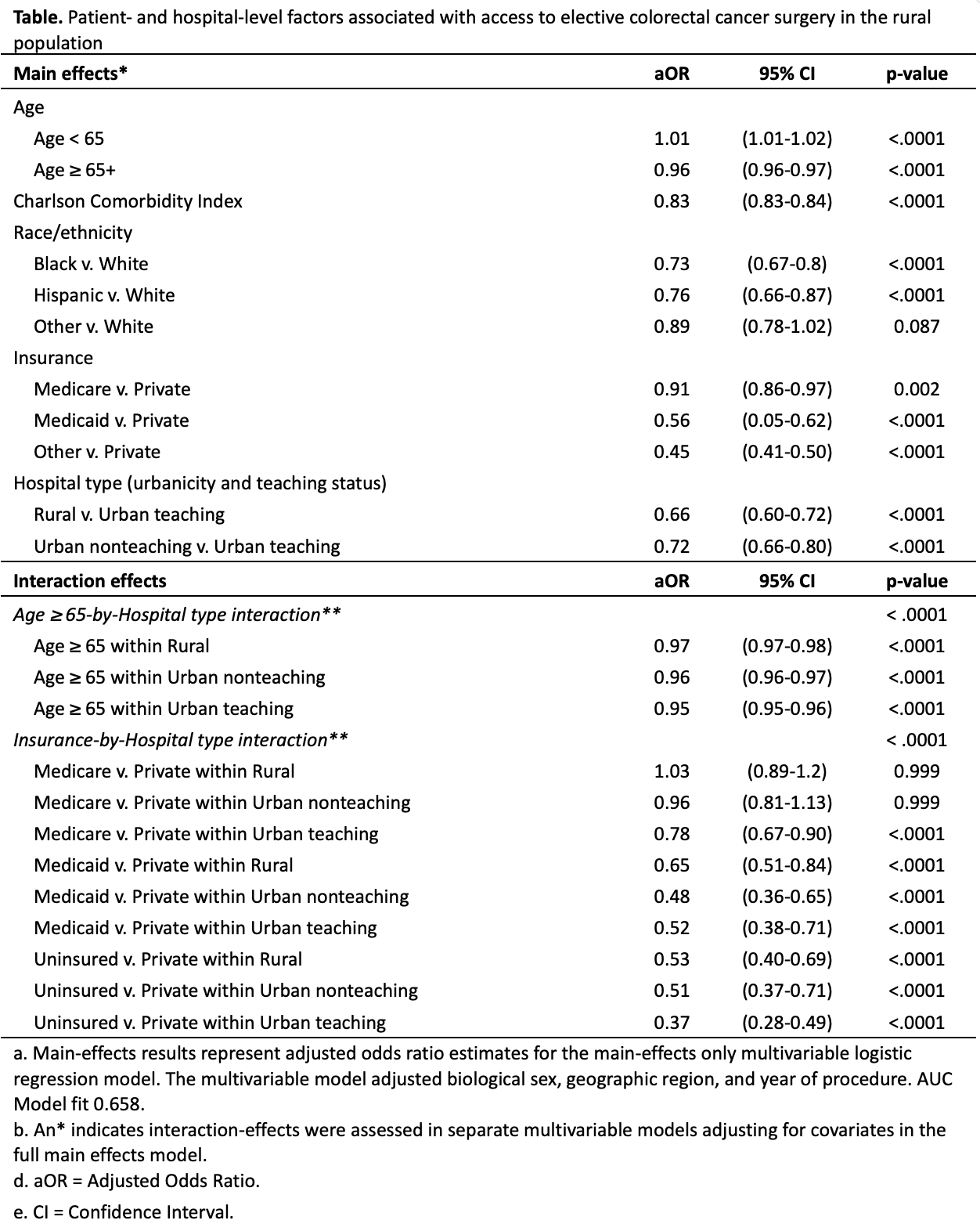
Results:Evaluation of the US Census Bureau and Policy map demonstrated that high risk rural populations were older adults (16%), Black (16%) or Hispanic (12%), and insured by Medicaid (20%) or uninsured (9%). In the US from 2007-2020, there were 69,212 hospitalizations of rural patients undergoing CRC surgery; of these, 62% were older (65+), 7% Black and 3% Hispanic, and 6% insured by Medicaid. At the facility-level, 44% of treating facilities were in the South and 34% were rural. Notably, over 72% of hospitalizations of rural patients were elective. However, unadjusted comparisons revealed that ethno-racial minorities, elders, uninsured, Medicaid beneficiaries, and rural hospitals were associated with lower odds of elective CRC surgery (for all, p-value < 0.05). Multivariate regression analysis demonstrated that older age, multimorbidity, Black race, Latino-Hispanic ethnicity, Medicaid insurance, and rural hospitals predicted lower odds of elective CRC. On interaction analyses, these estimates further dropped when elders, Medicaid beneficiaries, or the uninsured received their CRC surgery at urban hospitals (Table).
Conclusion:In this large study of rural dwellers, ethno-racial minorities, elders, and Medicaid beneficiaries had profoundly less access to elective CRC surgery especially when care received in urban settings. Future studies should focus on exploring actionable social drivers of health in these rural populations. Findings underscores the need for multi-level interventions to enhance rural access to equitable and quality surgical cancer care.
Back to 2024 Abstracts