Back to 2024 Abstracts
DISPARITIES IN ESOPHAGEAL CANCER CARE IN A BRAZILIAN POPULATION-BASED STUDY
Francisco Tustumi
*, Ricardo Y. Eri, Klaus W. Wende, Eric T. Nakamura, Daniel J. Szor
Sociedade Beneficente Israelita Brasileira Albert Einstein, Sao Paulo, São Paulo, Brazil
INTRODUCTIONHealthcare is heterogeneous throughout the world, especially in developing countries. Some patients receive cutting-edge treatment, while others have limited access to health resources. Vulnerable populations potentially have a worse prognosis for neoplasms that require highly complex treatment, such as esophageal cancer. The aim of the present study was to identify individual and municipal characteristics of access to health, including education, use of health plans, GDP per capita (GDPpc), and urban aspects, which could impact the survival of patients with esophageal cancer.
METHODSInformation on urban concentration (low, medium, or high), administrative hierarchy (local center, zone, center sub-regional center, regional capital, and metropolis), and GDPpc were extracted from Instituto Brasileiro de Geografia e Estatística/IBGE. Individual patient characteristics and access to healthcare data were obtained from Fundação Oncocentro/FOSP. Municipalities in the state of São Paulo/Brazil that provided healthcare to patients with esophageal cancer during the period 2013-2022 were included. Only patients with adenocarcinoma or squamous cell carcinoma (SCC) were selected, and those with other neoplasms or without information were excluded. Cox regressions were evaluated for overall survival (OS), investigating the independent variables GDPpc, urban concentration, municipal administrative hierarchy, health plan, education, and individual cancer and patient characteristics. Variables considered significant in the univariate model were selected for multivariate analysis.
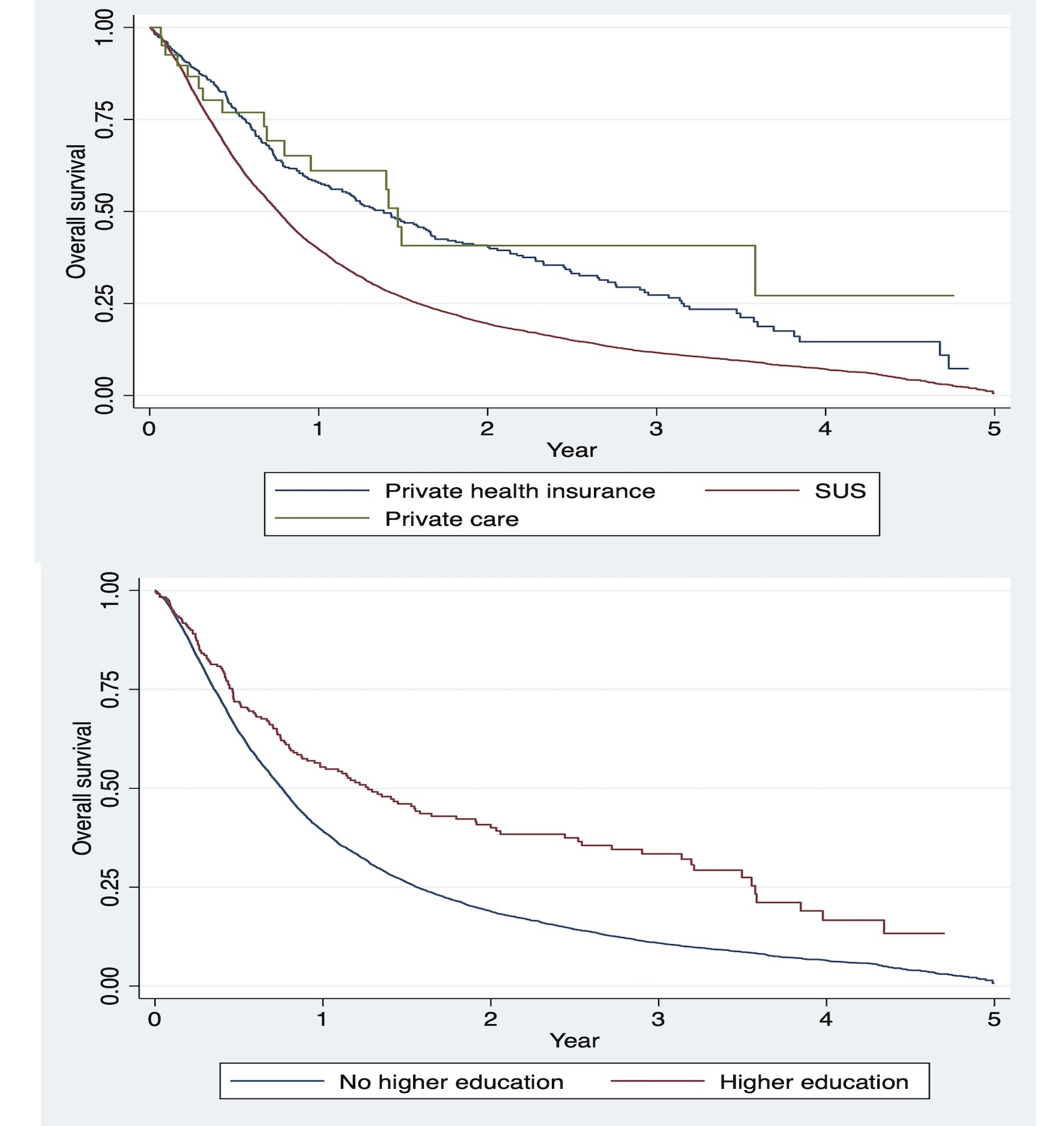
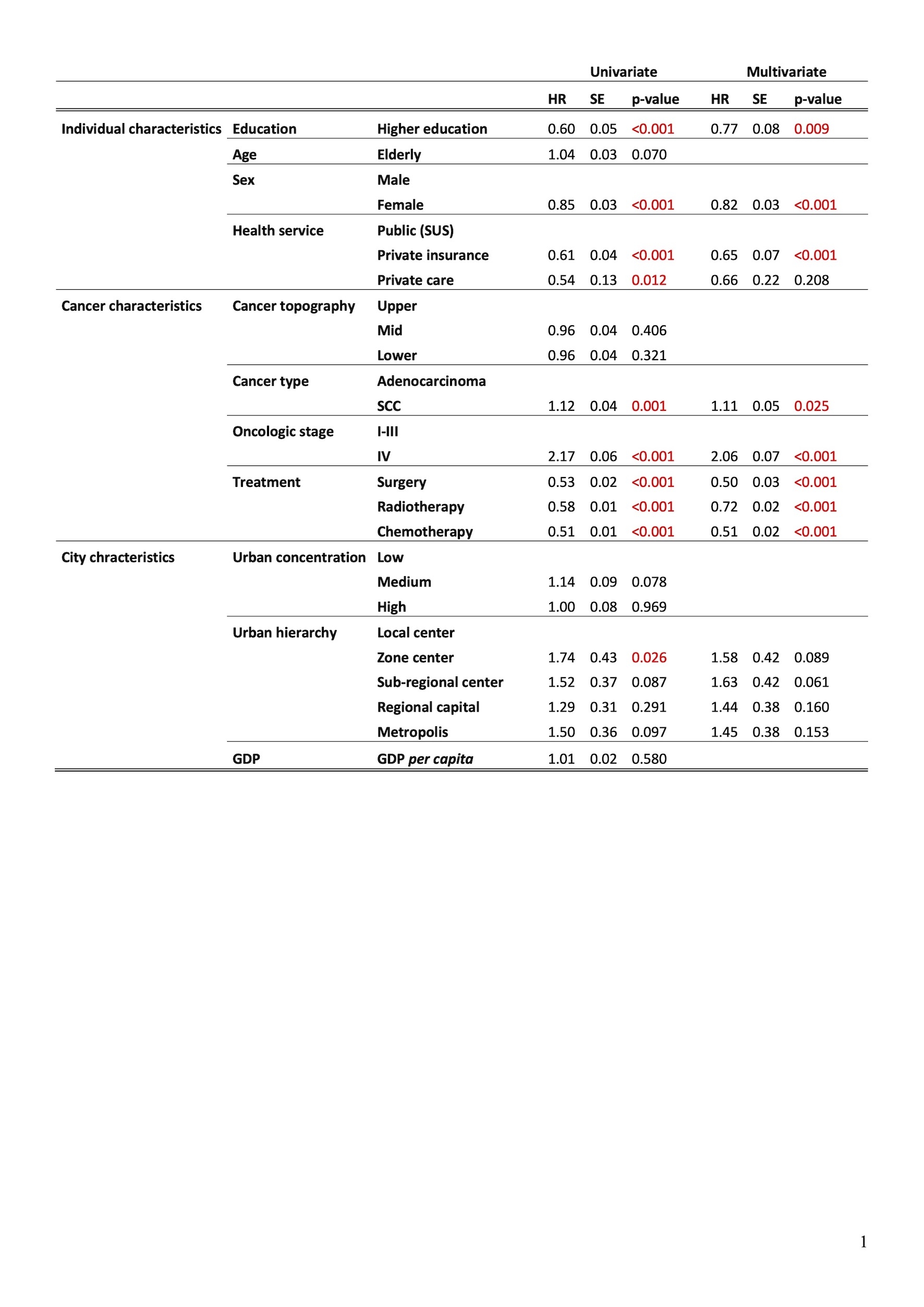
RESULTSAfter applying eligibility criteria, 9280 patients with esophageal cancer (85% SCC; 15% Adenocarcinoma) treated in 42 cities were selected. Only 4% of patients received private health care. In the univariate analysis, higher education (HR=0.6; SE=0.05; p< 0.001), female gender (HR=0.85; SE=0.03; p<0.001) and private health insurance (HR=0.65; SE=0.04; p<0.001) were considered protective factors for OS in esophageal cancer. Furthermore, stage IV, SCC, and treatment with surgery, chemotherapy, or radiotherapy impacted OS (p<0.05). In multivariate analysis, higher education (HR=0.77; SE=0.08; p=0.009), female gender (HR=0.82; SE=0.03; p<0.001), and private insurance (HR=0.65; SE=0.07; p<0.001) were considered protective variables. Cancer type, oncologic stage, and treatment also influenced OS. GDPpc and municipal urban concentration and hierarchy were not associated with OS.
CONCLUSIONSPopulations at risk, including those with low access to education and access to health, have a worse prognosis for esophageal cancer. Municipal GDPpc, urban concentration, and urban hierarchy have no independent association with OS. The results of the present study are useful for social public policy in esophageal cancer healthcare.
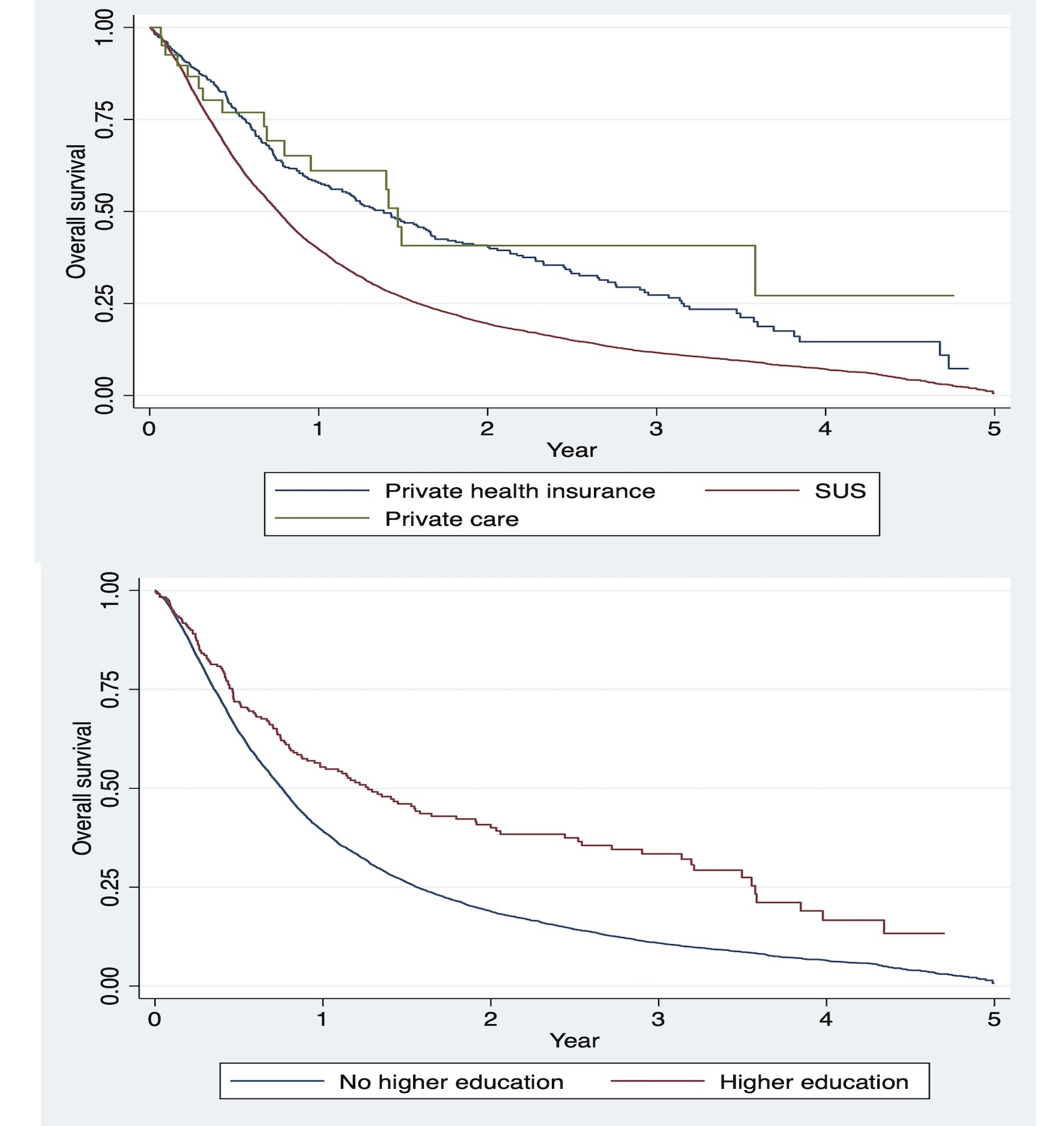
Kaplan–Meier estimator for overall survival according to health care access (upper) and higher education (university education) (bottom). SUS: Brazilian Public Health System (in Portuguese:
Sistema Único de Saúde).
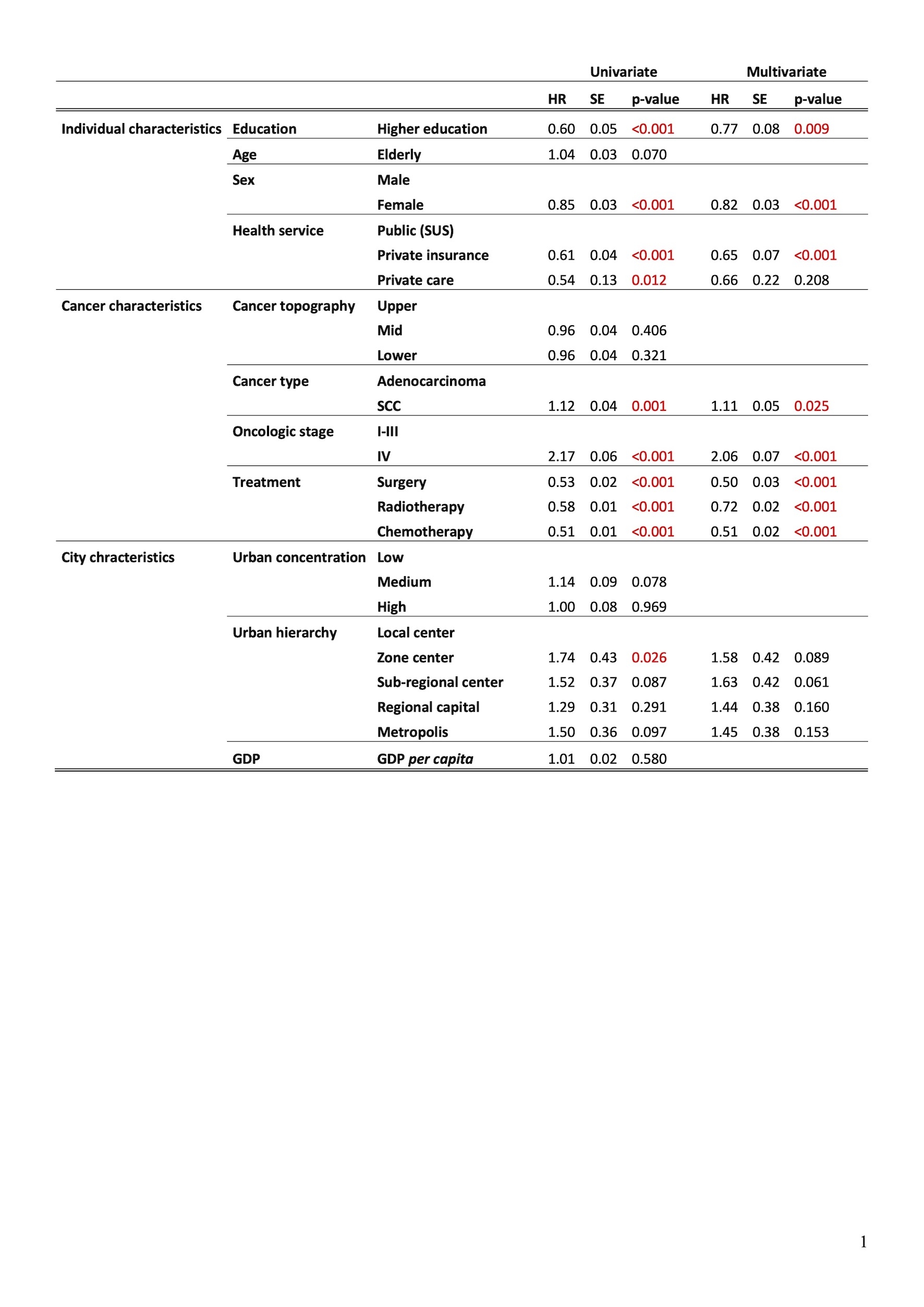
Uni and multivariate Cox regression analysis for overall survival. The red p-value shows significant results (p<0.05). SUS: Brazilian Public Health System (in Portuguese:
Sistema Único de Saúde).
Back to 2024 Abstracts