Back to 2024 Abstracts
PARENCHYMAL-SPARING HEPATECTOMY FOR MULTIPLE BILATERAL COLORECTAL LIVER METASTASES: POSITIVE MARGINS ARE NOT ASSOCIATED WITH HIGHER RECURRENCE
Mateo Lendoire de Undurraga
*, Harufumi Maki, Antony Haddad, Anish J. Jain, Hop S. Tran Cao, Yun Shin Chun, Ching-Wei D. Tzeng, Jean-Nicolas Vauthey, Timothy E. Newhook
Surgical Oncology, The University of Texas MD Anderson Cancer Center, Houston, TX
Background: Surgeons may consider parenchymal-sparing (PSH) or one-stage major hepatectomy (MH) for patients with bilateral colorectal liver metastases (CLM). However, outcomes of these two approaches for patients with advanced bilateral disease are underreported. We sought to evaluate outcomes between PSH and MH for patients with multiple, bilateral CLM.
Methods: A prospective database was queried for patients with 5 or more bilateral CLM who underwent R0/R1-intent initial one-stage hepatectomy (1998-2022). Postoperative follow-up imaging (computed tomography and/or magnetic resonance imaging) was reviewed to identify local recurrence (at the resection margin) and other intrahepatic recurrences (any intrahepatic recurrence without local recurrence). Outcomes were compared between patients who underwent PSH versus MH (≥ 3 Couinaud segments). Median follow-up was 49 months.
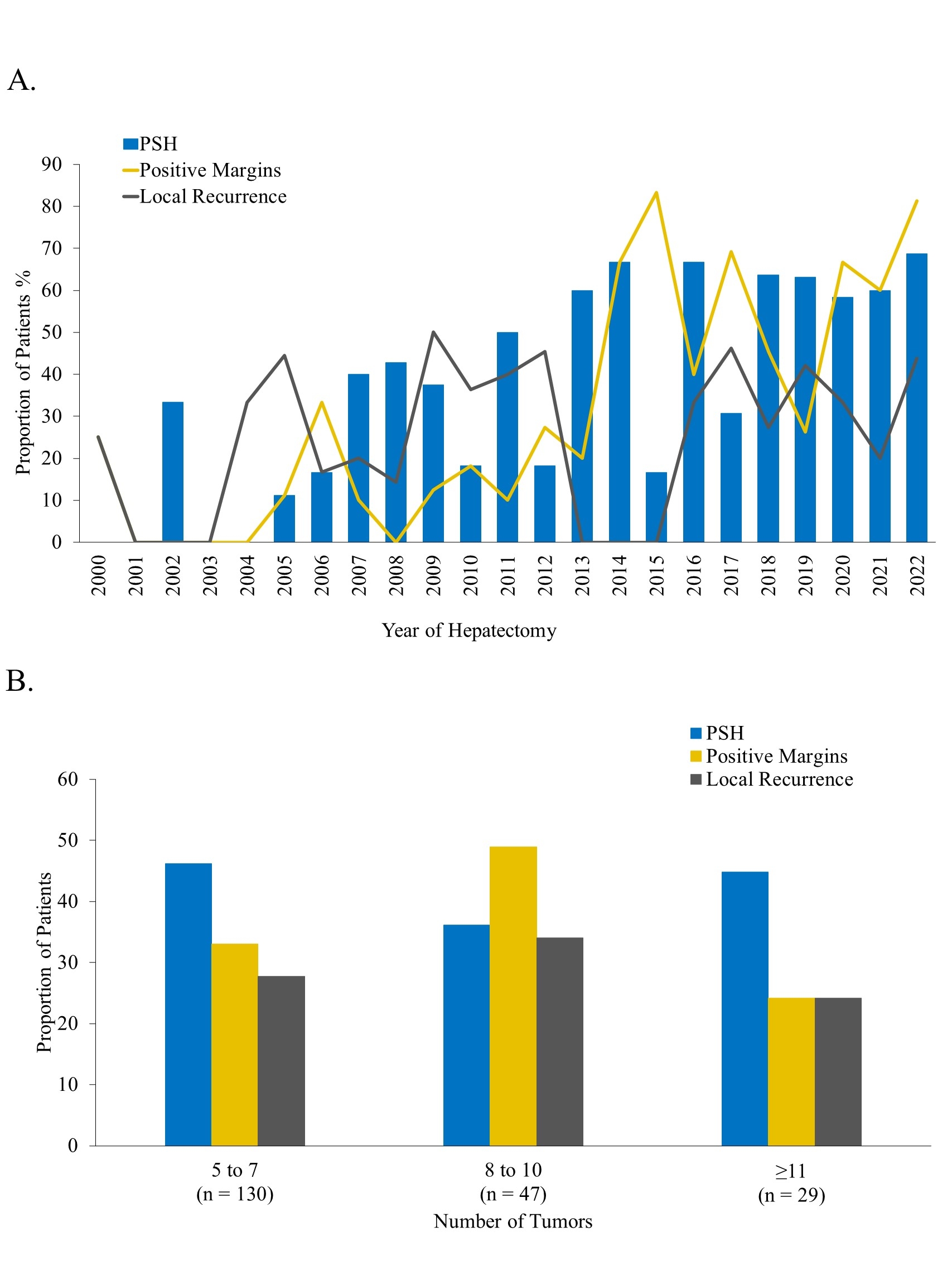
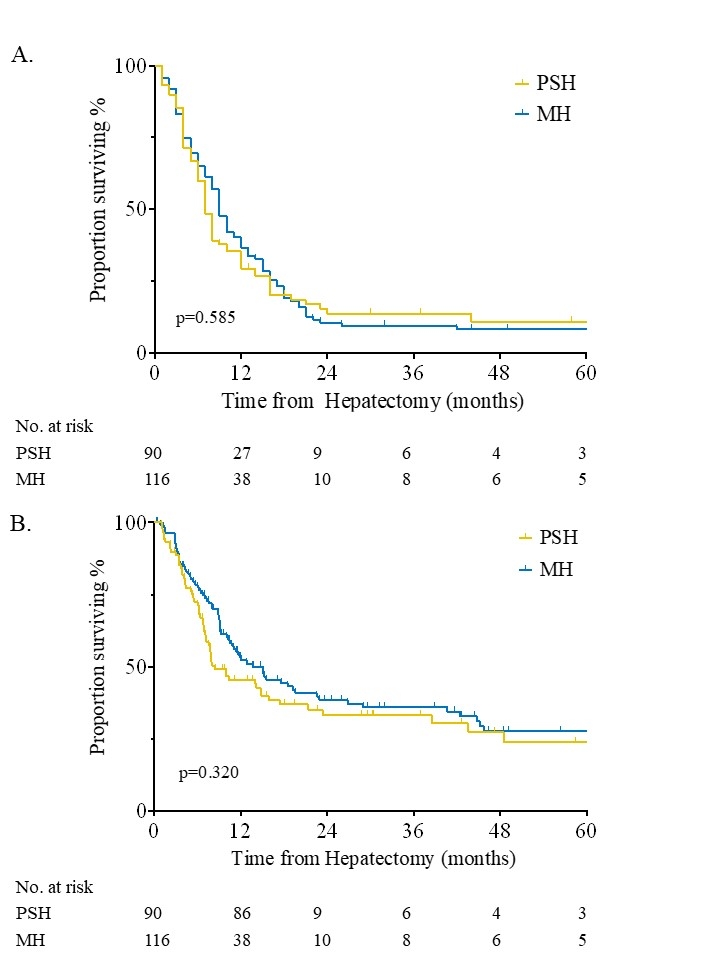
Results: Among 206 patients, median (IQR) number of tumors was 7 (5-9) and maximum tumor size was 3 cm (2-4 cm). 90 (44%) patients underwent PSH and 116 (56%) MH, and PSH had smaller tumors (2 vs. 3.5 cm; p=0.001). No differences were observed in number of tumors (median 7 vs. 7, p=0.392), treatment approach, or mutational profiles between the two groups. Patients who underwent PSH had significantly lower rates of post-hepatectomy liver insufficiency (1% vs. 13%, p=0.030). The use of PSH steadily increased during the study period, and more patients with PSH had margin-positive resection (47% vs. 30%; p=0.02; Fig. 1A). Across the study period, 173 (84%) patients recurred. Median local recurrence-free survival (23 months vs. not reached, p=0.184), recurrence-free survival (RFS, 7 vs. 9 months, p=0.585; Fig. 2A), and hepatic-specific disease-free survival (DFS, 8 vs. 14 months, p=0.320; Fig. 2B) were similar, regardless of the surgical approach. When stratified by tumor number, rates of PSH, margin-positive resection and local recurrence were comparable between PSH and MH (all p>0.100; Fig. 1B). Overall survival was similar between PSH and MH (median 59 vs. 47 months, p=0.072).
Conclusions: For patients with multiple bilateral CLM undergoing R0/R1-intent hepatectomy, PSH is safer and is associated with increased rates of microscopically-positive margins compared to MH, but no difference in hepatic-specific DFS, RFS, or local RFS.
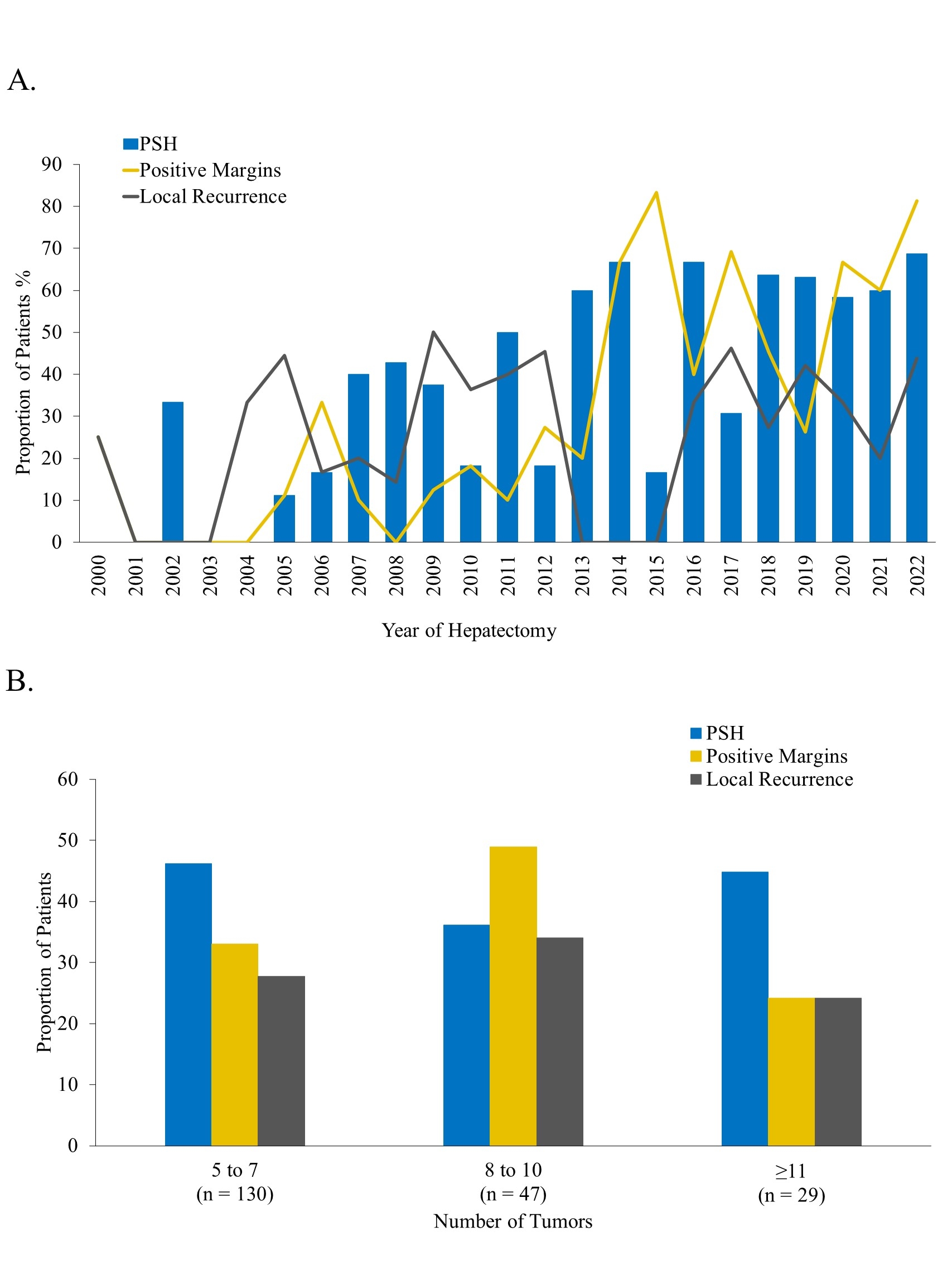 Figure 1.
Figure 1. A. Rates of PSH, R1 resection, and local recurrence over the study period. B. Rates of R1 resection (p=0.165), local recurrence (p=0.517), and PSH (p=0.498) according to the number of CLM. PSH, Parenchymal-Sparing Hepatectomy.
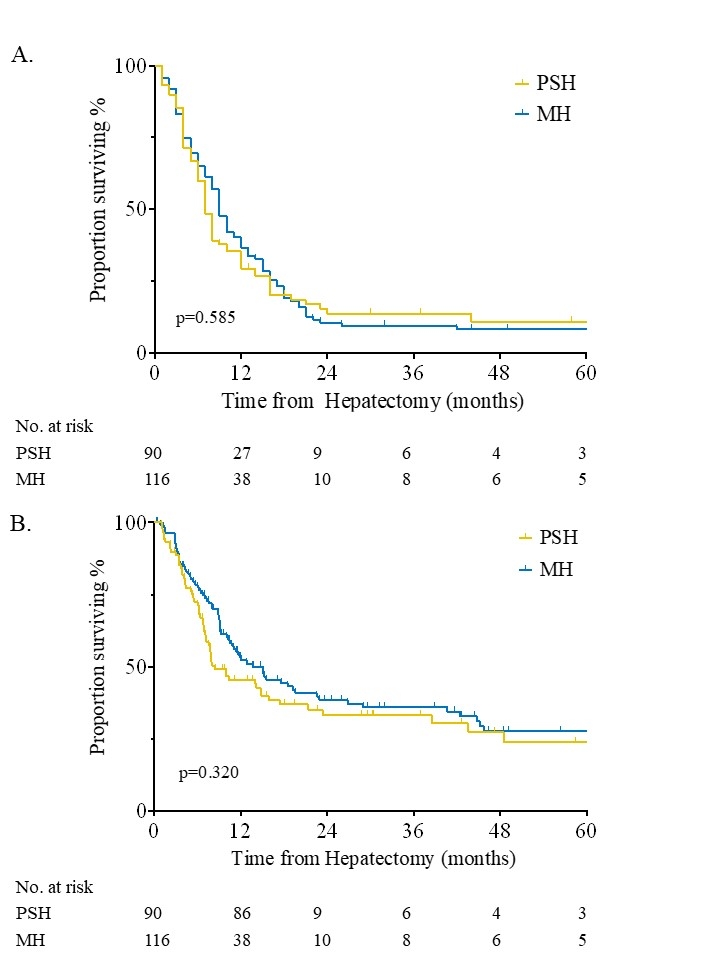 Figure 2.
Figure 2. Kaplan-Meier curves for Recurrence-Free Survival (A) and Hepatic-Specific Disease-Free Survival (B) by surgical approach. PSH, Parenchymal-Sparing Hepatectomy; MH, Major Hepatectomy.
Back to 2024 Abstracts