Back to 2024 Abstracts
ANALYSIS OF LEARNING CURVE AFTER 500 ROBOTIC HEPATECTOMIES
Sharona Ross, Michelle M. Dugan
*, Maria Christodoulou, Tara M. Pattilachan, Iswanto Sucandy
Digestive Health Institute, AdventHealth Tampa, Tampa, FL
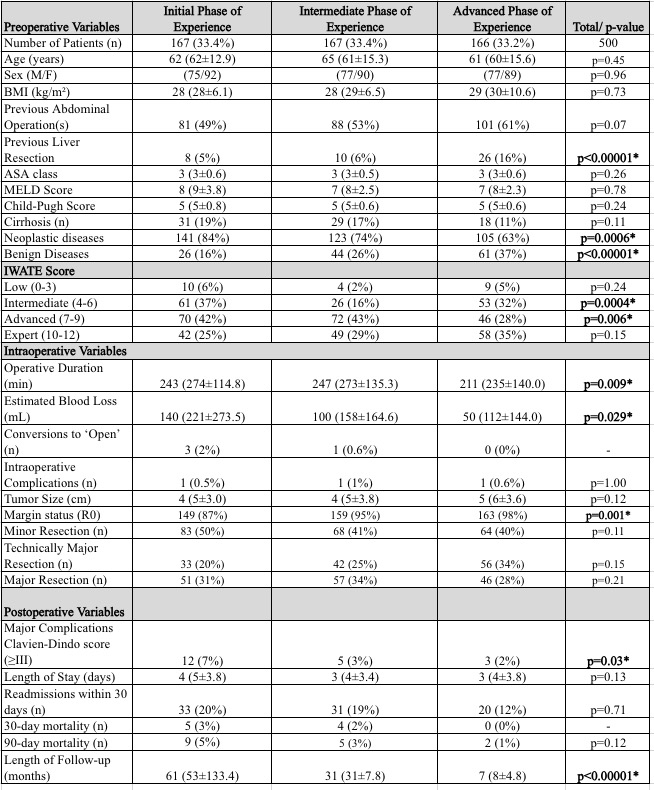
BACKGROUNDRobotic platform is rapidly growing in popularity for complex hepatobiliary resections due to its safety, efficacy, and superior dissection capabilities, when compared to the conventional open approach. To ensure patient safety and comfort level of the operating surgeon, it is critical to understand the learning curve required to achieve technical competency for each type of resections. While learning curve to achieve basic competency in robotic hepatectomy had been reported based on reviews of small (<200 patients) single institutional series, a review based on large cohort is nonexistent. To our knowledge, this is the first study in North America to analyze the robotic learning curve in achieving mastery based on a decade of experience with more than 500 robotic hepatectomies.
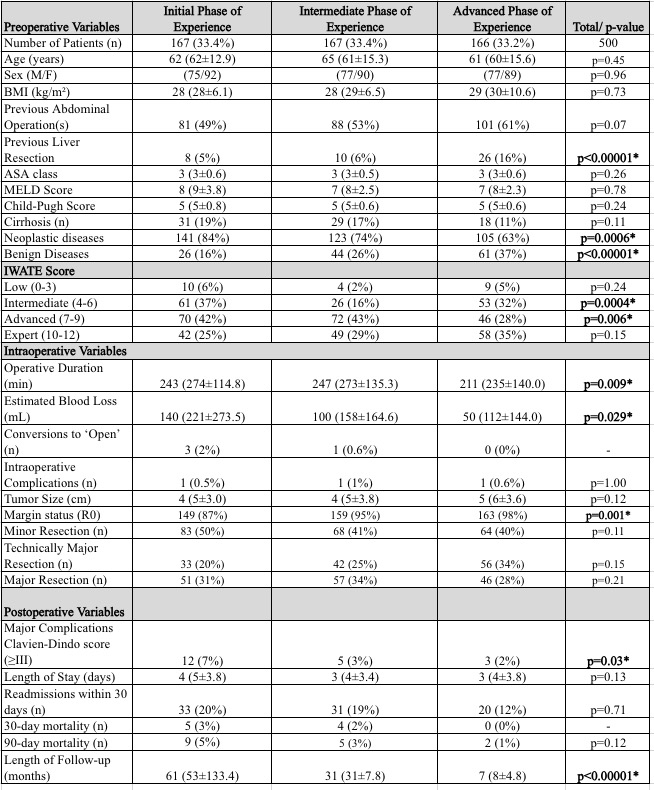
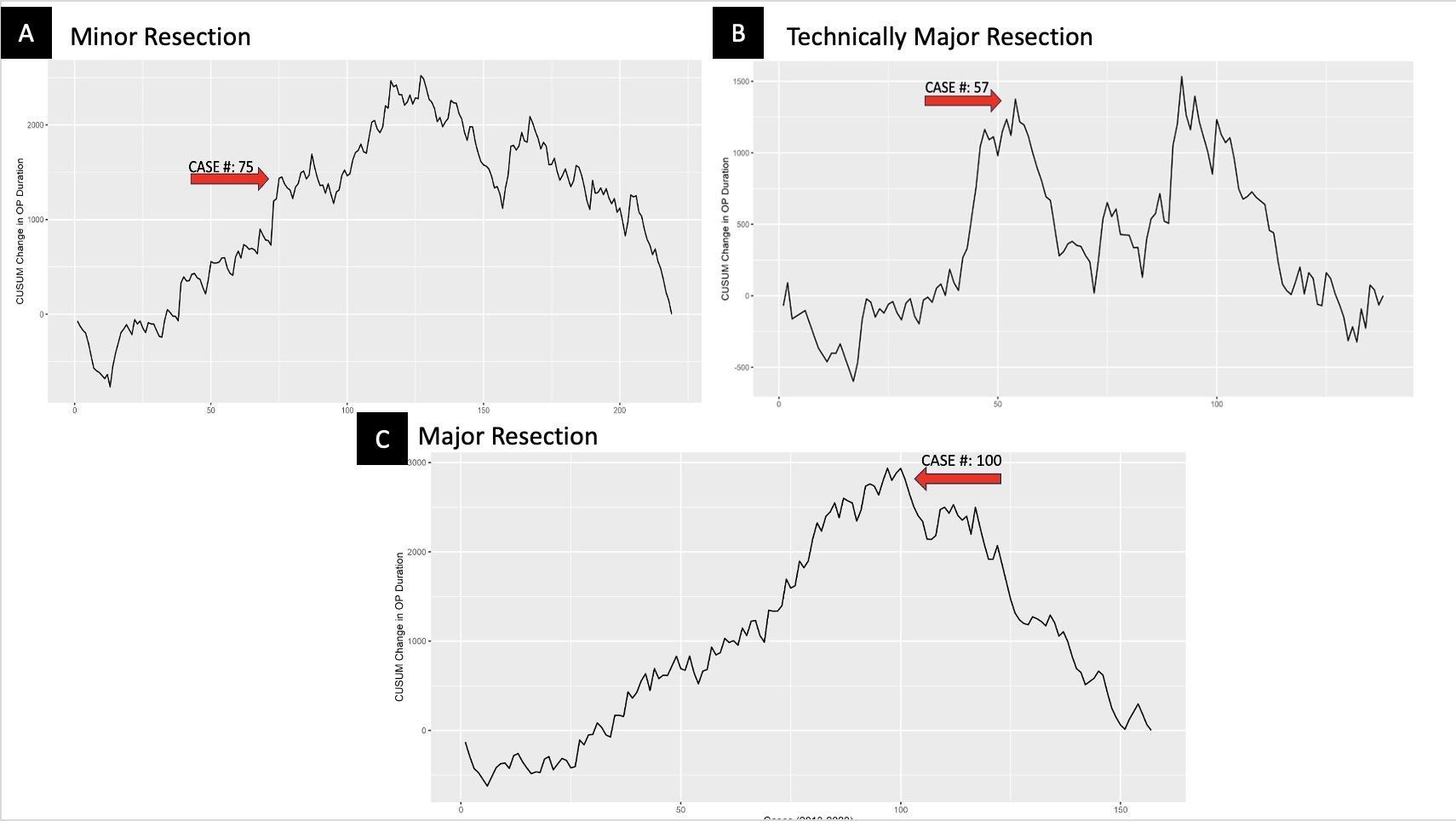
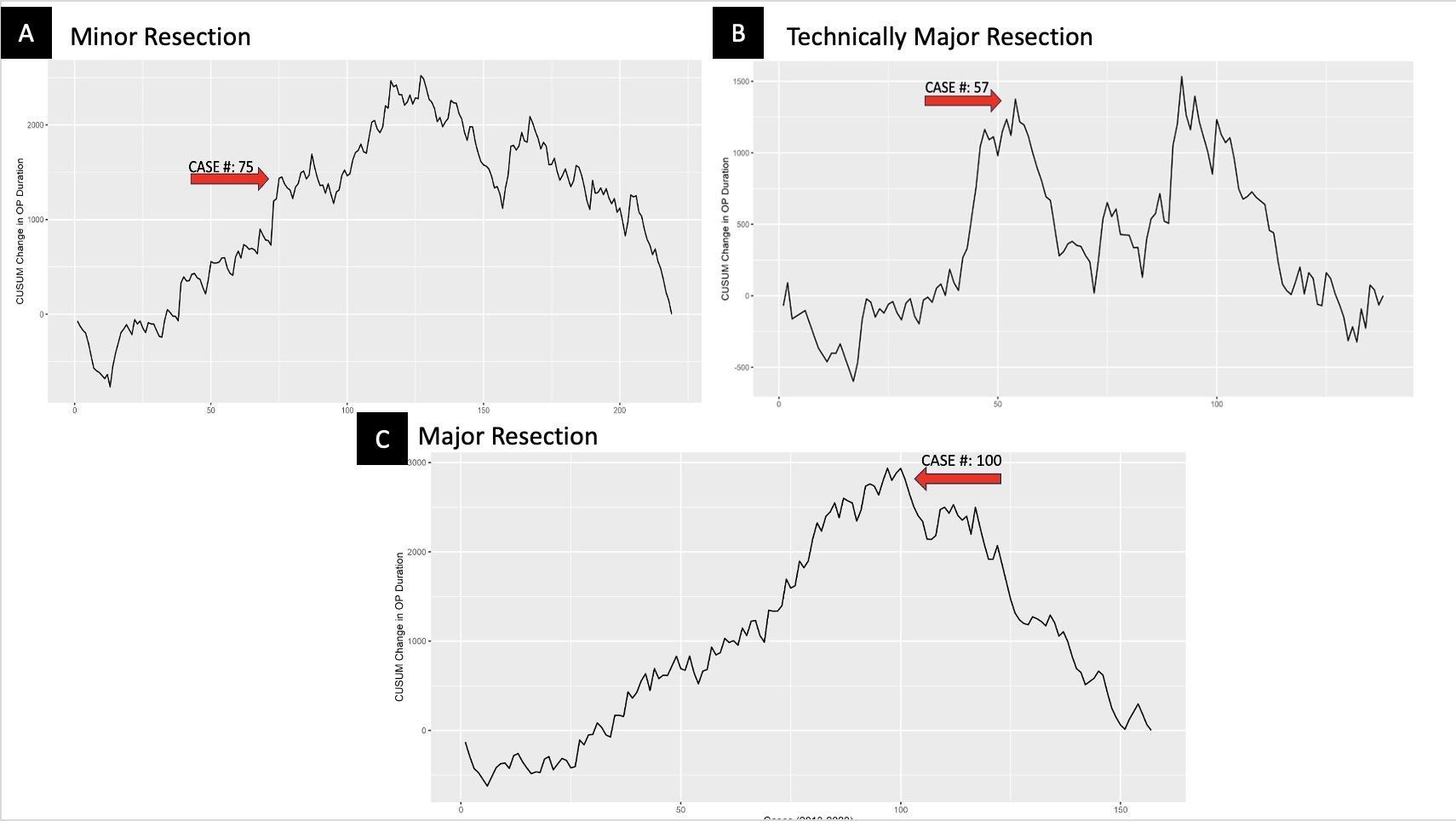
METHODSA prospectively collected database of all patients who underwent robotic hepatectomy at a high-volume institution from 2013 to 2023 were queried. Cumulative Sum Chart (CUSUM) analysis using operative duration was utilized to determine the learning curve for minor, major, and technically major hepatectomy. Technically major resection is defined as resection of segment 7,8, and/or 4A. Data are presented as median (mean ± SD).
RESULTS500 consecutive patients who underwent robotic hepatectomy were included in the study, comprised of 46% men and 54% women, aged 63 (61 ± 14.6) years, with BMI of 28 (29 ± 8.0) kg/m
2, MELD of 7 (8 ± 3.0), Child-Pugh score 5 (5 ± 0.7), 16% with cirrhosis, and 74% with neoplastic liver disease. Operative duration was 235 (260.1 ± 131.9) minutes, EBL was 100 (165 ± 208.1) mL, tumor size was 4 (5 ± 3.5) cm, and R0 margins were achieved in 94%. Major postoperative complications occurred in 4%, hospital stay was 3 (4 ± 3.7) days, 30-day readmission was 17%, 30-day mortality was 2%, and 90-day mortality was 3%. Of the 500 hepatectomies, 215 were minor resections, 154 major resections, and 131 technically major resections. On CUSUM analysis, the learning curve for minor resection was 75 cases, for major resection was 100 cases, and for technically major resection was 57 cases (Figure 1). As we became more mature in our experience, we undertook hepatectomies with shorter operative duration, less blood loss, higher R0 resection margin status, and lower major postoperative complications, as shown in Table 1.
CONCLUSIONSThe needed minimum numbers of robotic hepatectomy undertaken to overcome the learning curves for minor, major, and technically major were quite significant. We believe this study can be used to help guide surgeons in their early robotic hepatectomy experience to ensure patient safety and best oncological long-term outcomes.
Back to 2024 Abstracts