Back to 2024 Abstracts
ASSOCIATION OF FRAGMENTATION OF CANCER CARE WITH SURVIVAL IN HEPATOCELLULAR CARCINOMA
Hester C. Timmerhuis, Rejoice F. Ngongoni
*, Amy Y. Li, Heather Day, Adam Furst, Katherine Arnow, Brendan Visser
Stanford University School of Medicine, Stanford, CA
IntroductionFragmentation of care (FC) refers to healthcare that is delivered by various providers and/or facilities. This has been linked to inferior outcomes, yet it increases access to specialized cancer care. The primary objective was to investigate the association of FC for hepatocellular carcinoma (HCC) with survival.
MethodsIn this retrospective cohort study, adults diagnosed with HCC from January 2007 to December 2017 were identified using the California Cancer Registry. Facility-related information for each patient visit was linked to the California Healthcare Access and Information database. FC was measured by: (1) the quantity of healthcare facilities a patient visited within two years after diagnosis and (2) the “directionality� of transitions of care between cancer-designated facilities (National Comprehensive Cancer Network [NCCN] or National Cancer Institute [NCI]) and non-designated facilities. Baseline demographic, cancer-specific, and facility-specific data were collected. The association of FC quantity and directionality with survival was determined using multivariable Cox regression analyses with FC expressed as a time-varying covariate.
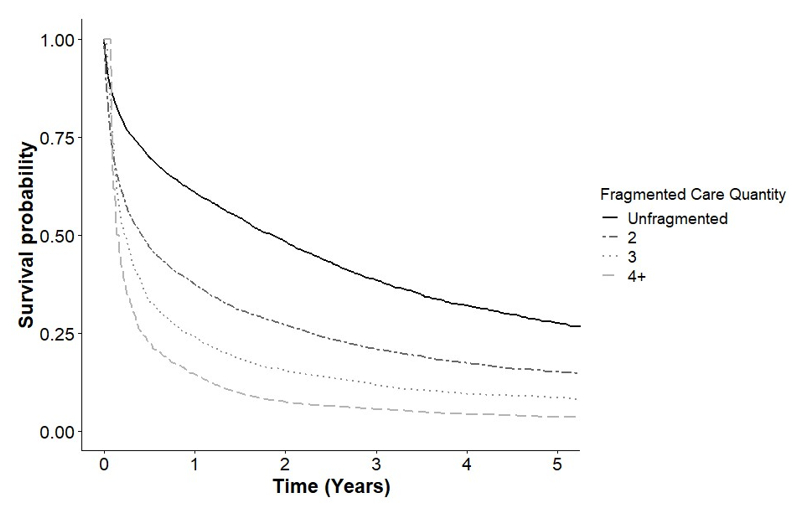
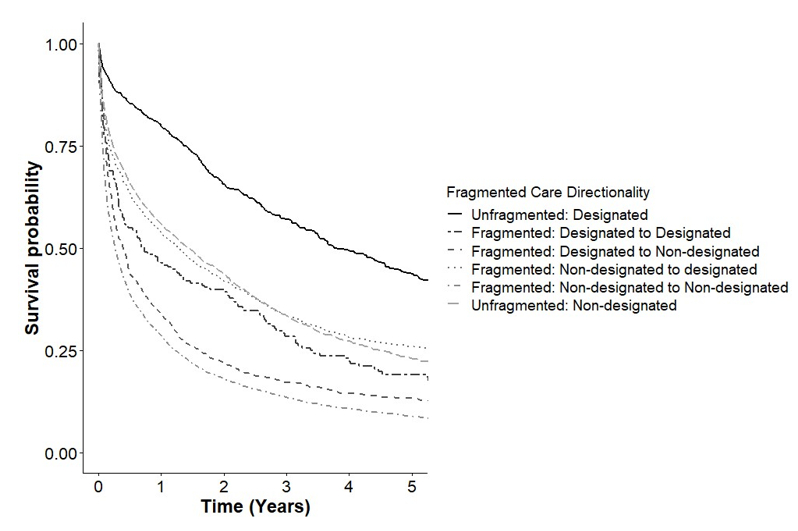
ResultsOf 10,825 eligible patients, 5,047(46.6%) received unfragmented care, 3,679(34.0%) received care at 2 facilities, 1,448(13.4%) received care at 3 facilities, and 651(6.0%) received care at 4 or more facilities. Using Cox regression, increasing FC quantity was associated with higher mortality (2 facilities: HR:1.65, 95% CI:(1.56,1.75), p<0.001; 3 facilities: HR:2.21, 95% CI:(2.02,2.41), p<0.001; 4+ facilities: HR:2.66, 95% CI:(2.35,3.02), p<0.001) (Figure 1). The FC directionality model showed that compared to unfragmented designated care all other care direction types were associated with higher mortality (unfragmented non-designated care: HR:1.47, 95% CI:(1.34,1.61); non-designated to designated care: HR:1.74, 95% CI:(1.55,1.95); designated to designated care: HR:2.27, 95% CI:(1.82,2.84); designated to non-designated care: HR:2.61, 95% CI:(2.32,2.95); undesignated to undesignated care: HR:2.61, 95% CI:(2.37,2.87), all p<0.001), Figure 2). Fragmentation of care was associated with poor outcomes irrespective of the directionality of care transition. Specifically, transition of care from a non-designated to a designated center was associated with poorer outcomes (HR:1.74, p<0.001) than non-fragmented care at an undesignated center (HR:1.47, p<0.001) (Figure 2).
ConclusionFC is associated with mortality in HCC patients and worsens as the number of facilities increases. “Upgrading care� from a non-designated center to an NCCN/NCI center does not appear to overcome the detriment associated with fragmentation of care in outcomes. This requires further investigation because it contradicts the dogma that referral to specialized centers after cancer diagnosis is associated with improved outcomes.
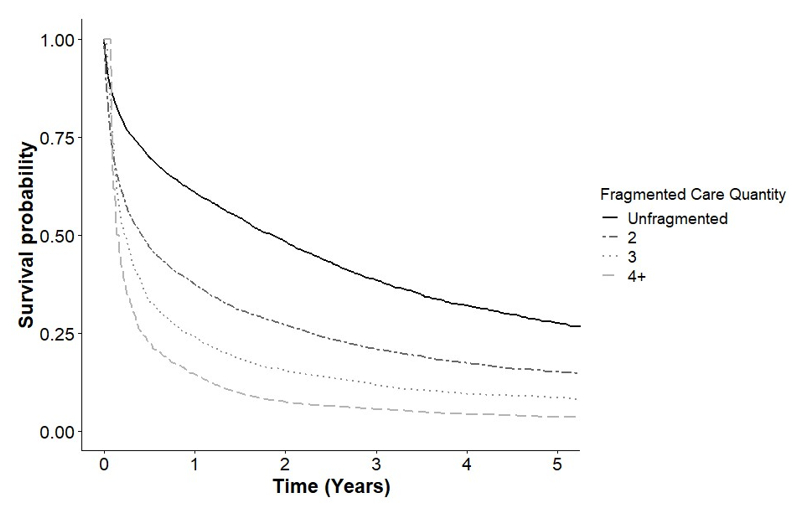
Figure 1. Multivariable time-varying covariate Cox regression of the association of fragmented care quantity (number of facilities visited) with survival in patient hepatocellular carcinoma
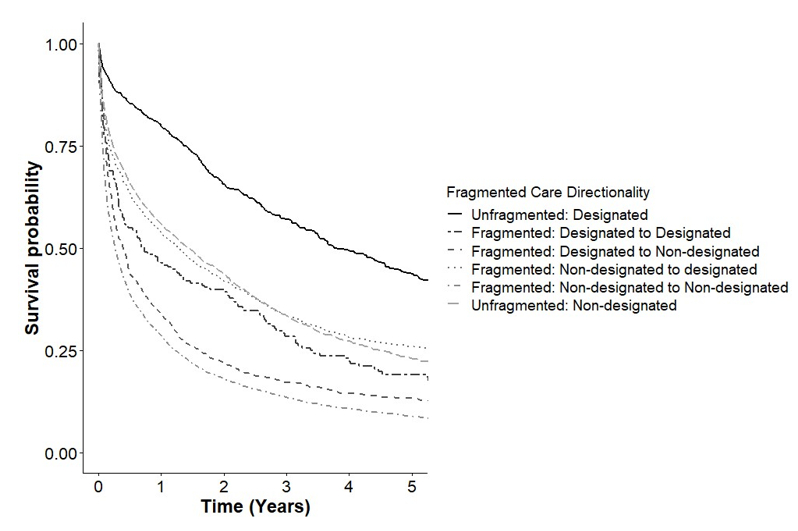
Figure 2. Multivariable time-varying covariate Cox regression of the association of fragmented care directionality (transitioning care between cancer designated and non-cancer designated facilities) and survival in patients with hepatocellular carcinoma
Back to 2024 Abstracts