Back to 2024 Abstracts
EXCEPTIONAL PATHOLOGIC RESPONSE TO PREOPERATIVE THERAPY IN THE CONTEXT OF MUTATIONAL PROFILING FOR COLORECTAL LIVER METASTASES
Mateo Lendoire de Undurraga
*, Harufumi Maki, Antony Haddad, Timothy E. Newhook, Yun Shin Chun, Ching-Wei D. Tzeng, Jean-Nicolas Vauthey, Hop S. Tran Cao
Surgical Oncology, The University of Texas MD Anderson Cancer Center, Houston, TX
Introduction: Pathologic response after preoperative chemotherapy has been associated with overall survival, and RAS mutational status could stratify patients with minor pathologic response (>50%). However, the significance of pathologic response (PR) after preoperative chemotherapy for colorectal liver metastases (CLM) in the age of mutational profiling with next generation sequencing is uncertain. We assessed degree of PR and evaluated its prognostic significance in the context of tumor mutational status.
Methods: A prospective database was queried for patients with CLM treated with 4-12 cycles of first-line chemotherapy and curative-intent initial hepatectomy during 2003-2021. Building on our prior work, and driven by the hypothesis that PR is not a dichotomous variable, we revised the definition of major PR. Thus, PR was categorized as complete (<1% residual viable tumor [RVT]), major (1%-9% RVT), intermediate (10%-49.9% RVT), or minor (≥50% RVT). The primary endpoint was OS.
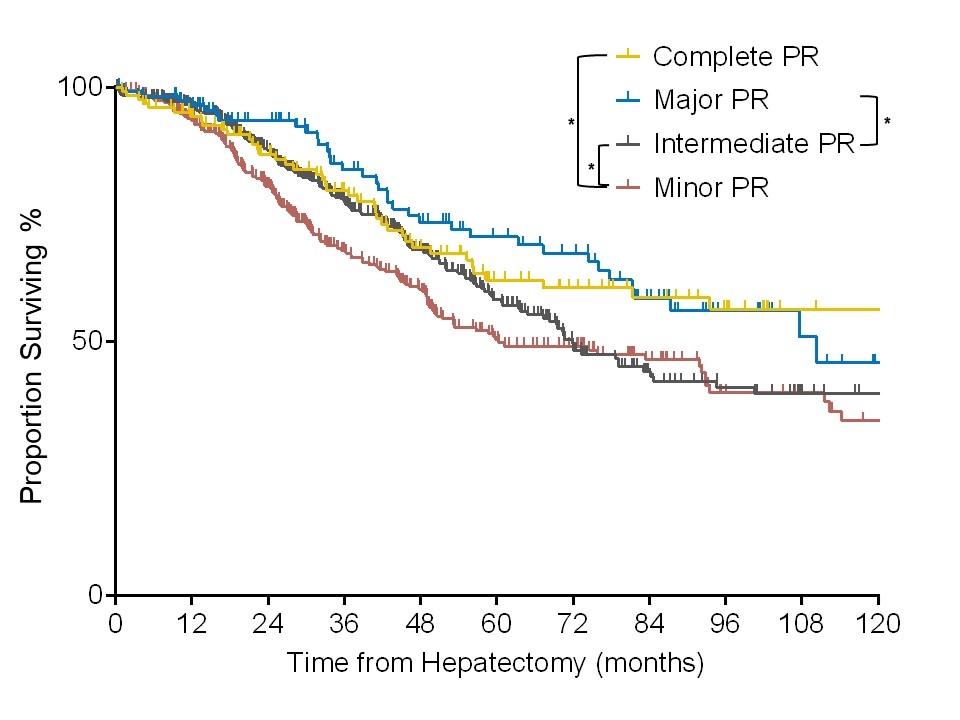
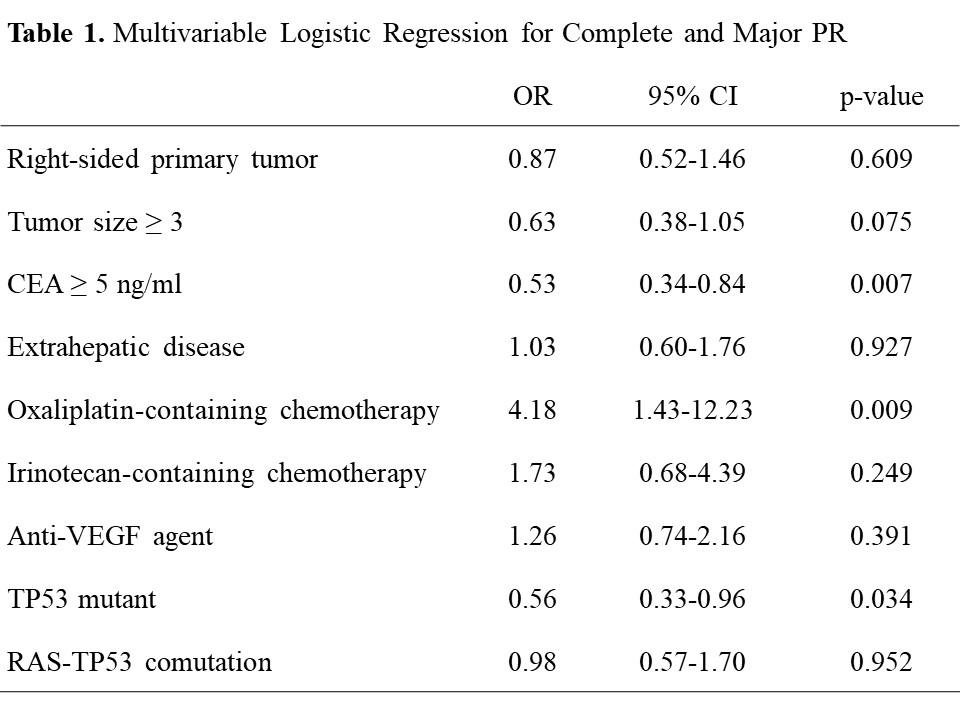
Results: The study included 958 patients with median follow-up of 60 months; 123 patients (12.8%) had complete PR, 112 (11.7%) major PR, 425 (44.4%) intermediate PR, and 298 (31.1%) minor PR. Median age of the cohort was 55 years; median number of chemotherapy cycles was 5. Median OS for major PR (9.2 years) was similar to median OS for complete PR (11.9 years, p=0.64) but significantly better than median OS for intermediate PR (6.0 years, p=0.035) and minor PR (5.0 years, p=0.003) (Figure 1). Nearly 20% of patients achieved complete or major PR regardless of the mutational status. On multivariable analysis, the independent predictors of complete and major PR were a CEA of 5 ng/ml or more, oxaliplatin-containing preoperative chemotherapy, and TP53 mutation (Table 1, all p<0.030).
Conclusion: Exceptional response, encompassing complete and major PR, is associated with markedly improved survival. Oxaliplatin-based preoperative chemotherapy and tumor biology were the most important predictors of such response.
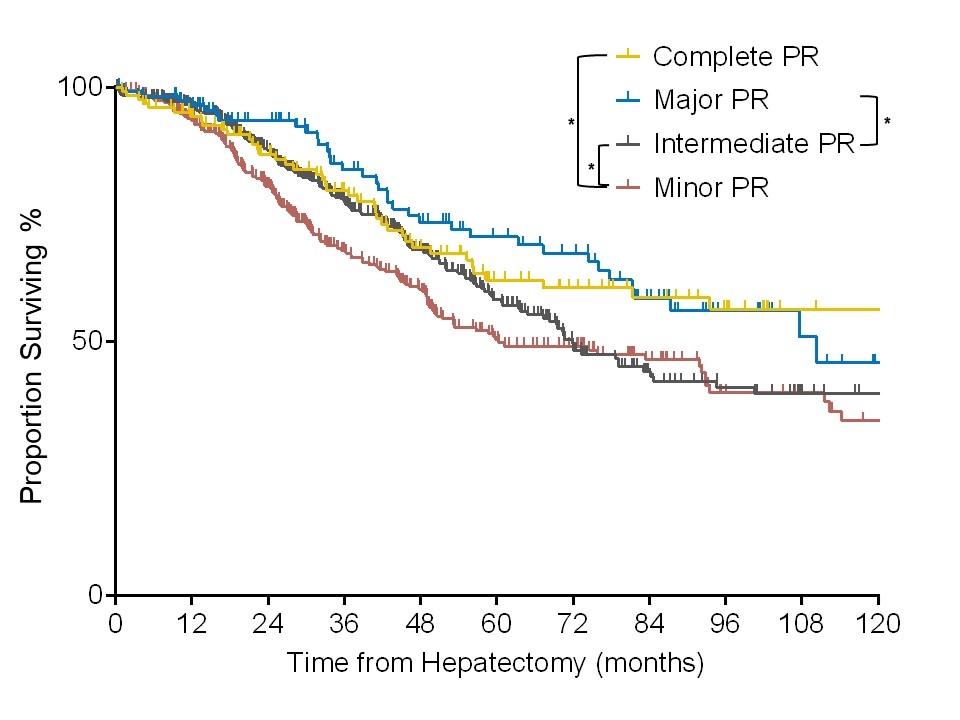 Figure 1.
Figure 1. Kaplan Meier curves for Overall Survival stratified by pathologic response (PR). Complete PR, 0% residual viable tumor (RVT); Major PR, 1-9% RVT; Intermediate PR, 10-49% RVT; Minor PR, 50-100% RVT.
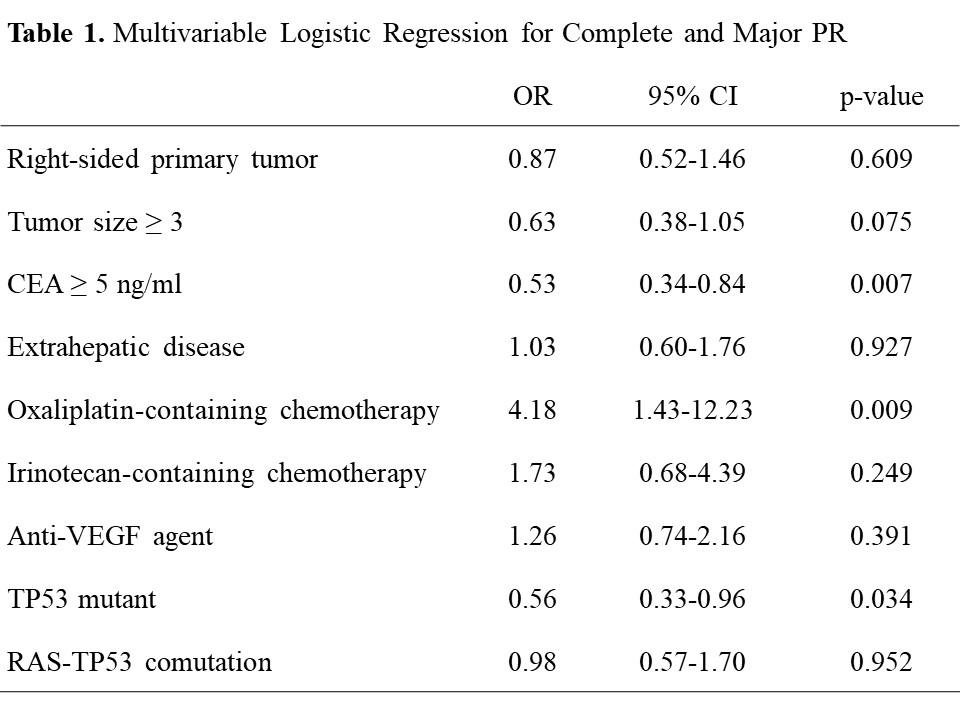 Table 1.
Table 1. Multivariable Logistic Regression for Complete and Major PR.
Back to 2024 Abstracts