Back to 2024 Abstracts
CONTRIBUTING FACTORS IN THE UTILIZATION OF MINIMALLY INVASIVE TECHNIQUES FOR VENTRAL HERNIA REPAIR: A SYSTEMATIC REVIEW AND META-ANALYSIS
Alexandra C. Skoczek
2, Alexander B. Holland
*1, Brody M. Fogleman
1, Dennis Fernandez
31Edward Via College of Osteopathic Medicine - Carolinas Campus, Spartanburg, SC; 2Edward Via College of Osteopathic Medicine - Auburn Campus, Auburn, AL; 3Crestwood Medical Center, Huntsville, AL
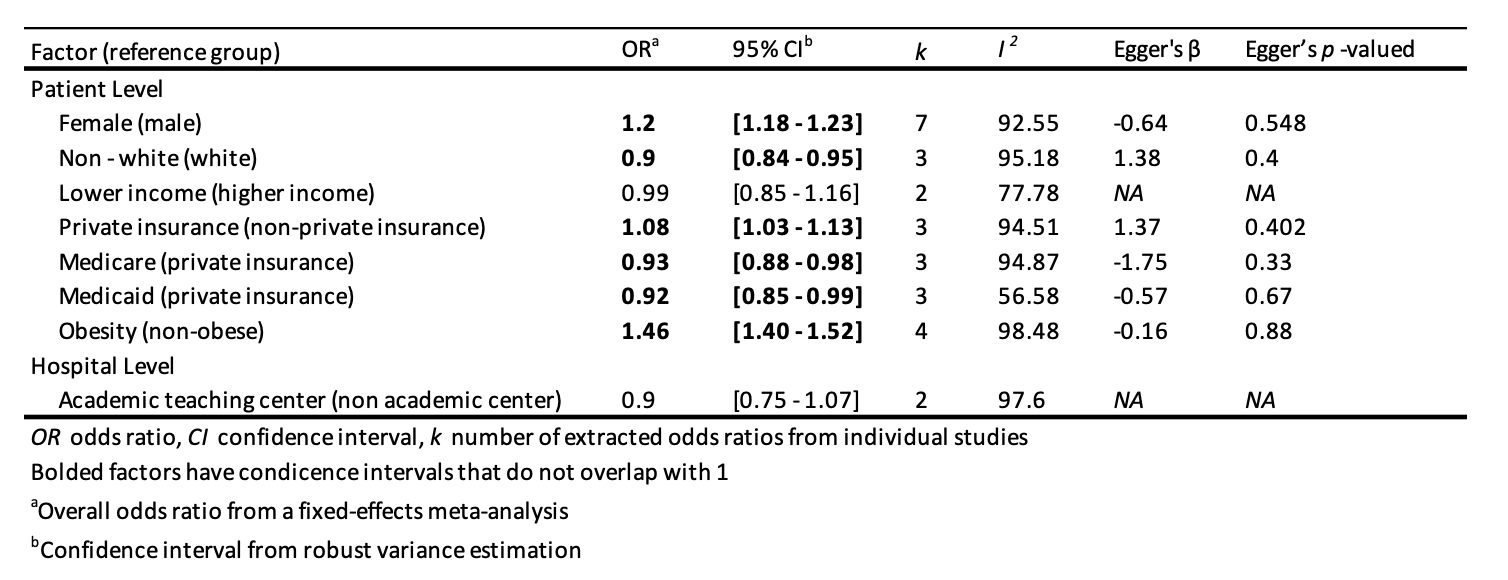
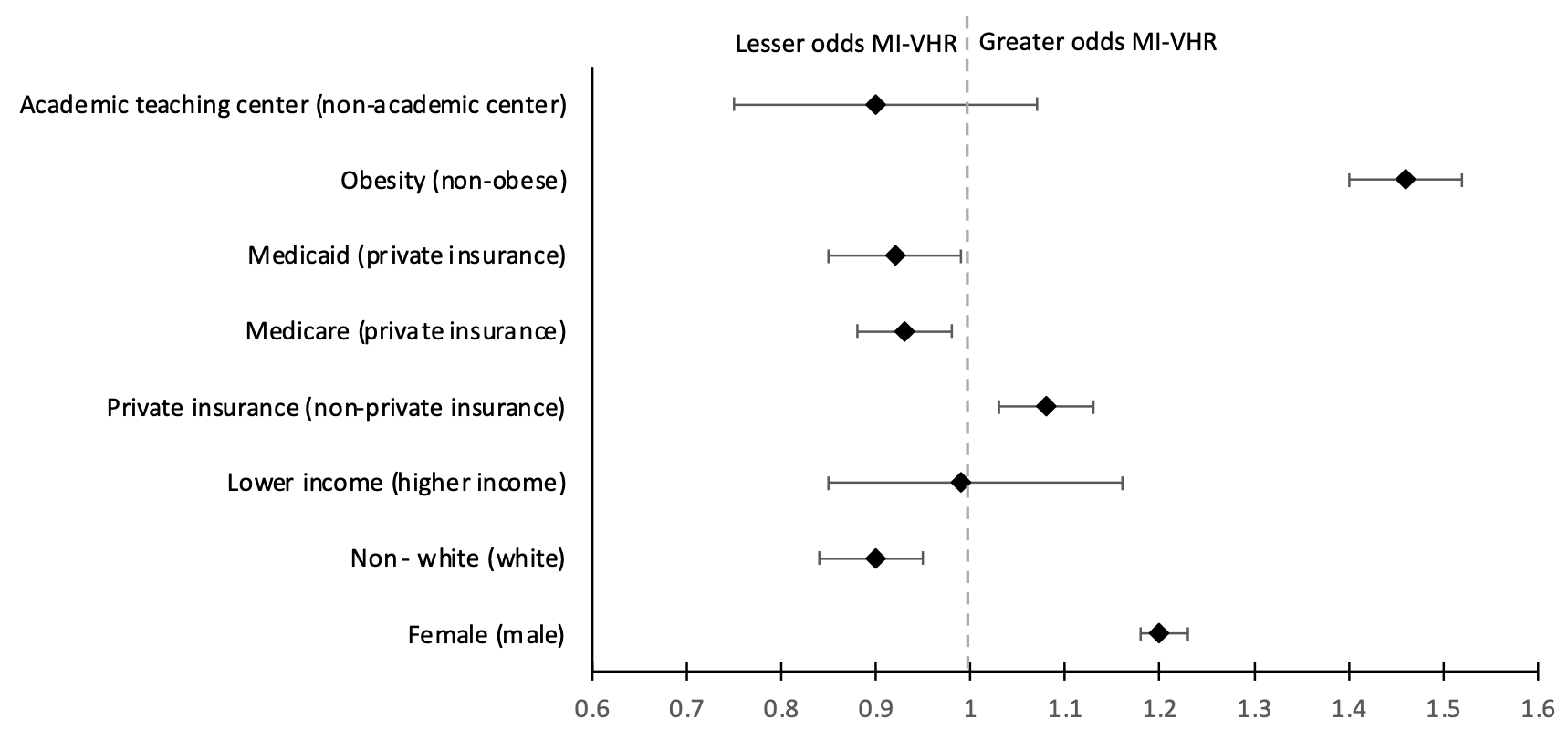
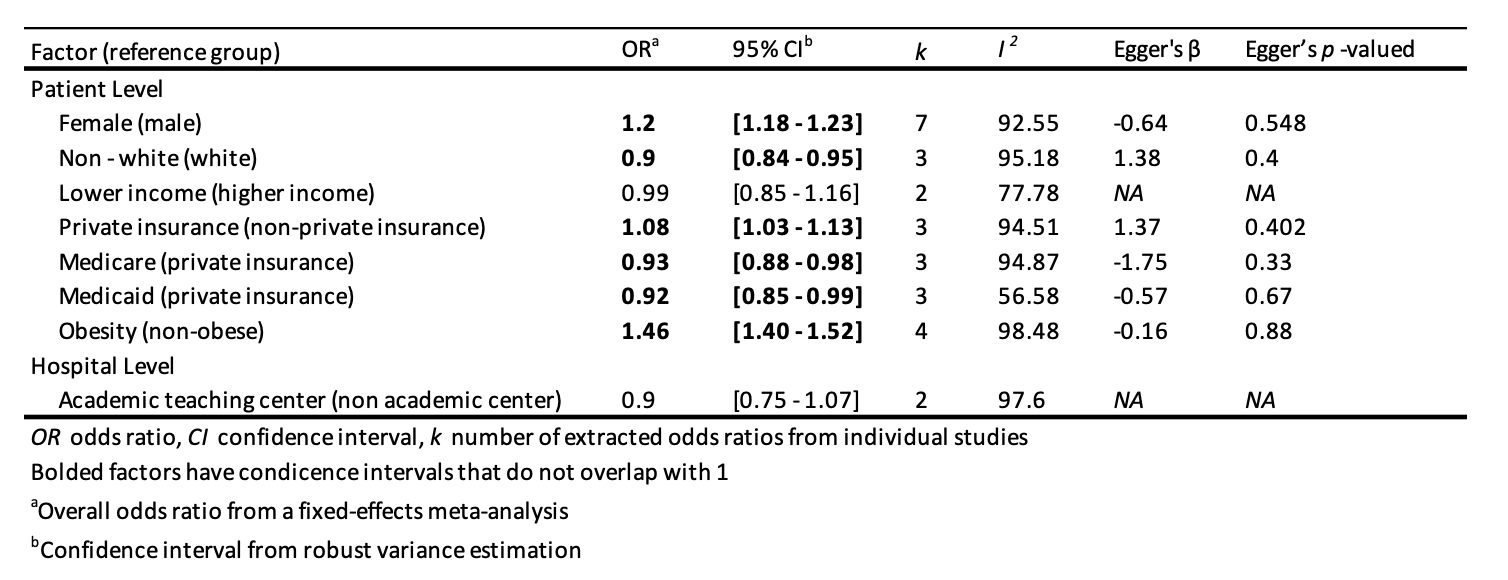
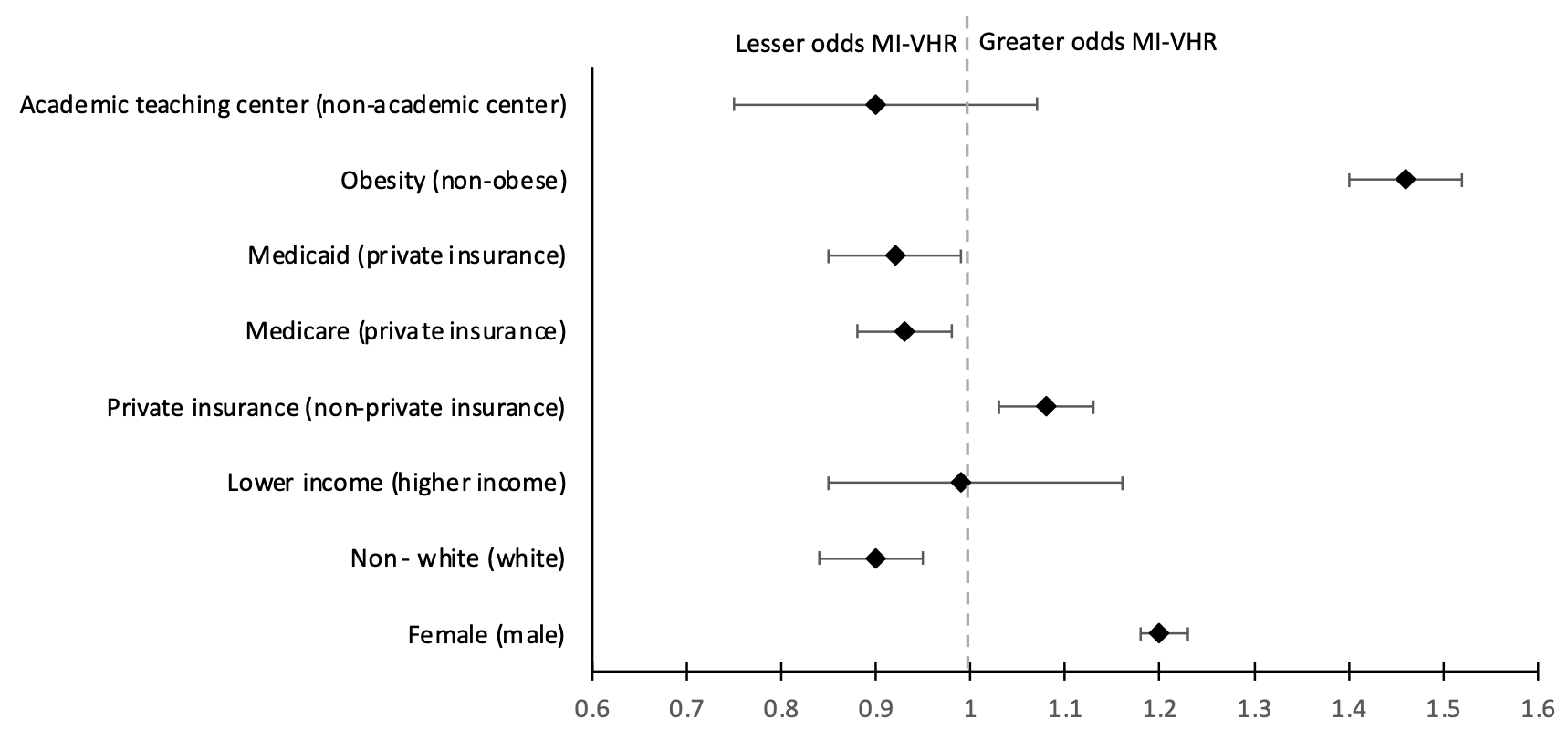
Background Ventral hernias, occurring in 15–20% of patients following gastrointestinal surgery, necessitate over 400,000 repairs annually in the United States. Despite the prevalence, a consensus on the optimal technique for ventral hernia repair remains elusive. The available approaches include open, laparoscopic, and robotic procedures, each with their merits. Minimally invasive techniques have shown promise in various postoperative outcomes, including lower rates of surgical site infections, hernia recurrence, and postoperative pain. However, the higher operative cost of such procedures, coupled with potential access disparities, presents challenges in determining the most effective approach. Objective This study seeks to identify the factors that influence the utilization of minimally invasive surgical techniques in ventral hernia repair. Methods A systematic review and fixed-effects meta-analysis of published studies comparing the utilization of minimally invasive techniques to open techniques in ventral hernia repair were conducted. Eligible studies were identified through searches in PubMed and EMBASE in November 2023, and the screening of articles was performed using the Rayyan platform. Results The meta-analysis included seven studies, revealing notable trends in patient characteristics influencing the choice of minimally invasive ventral hernia repair. Patients were more likely to undergo minimally invasive ventral hernia repair if they were female (OR = 1.20, 1.18 – 1.23), obese (OR = 1.46, 1.40 – 1.52), and had private insurance (OR = 1.08, 1.03 – 1.13). Patients who were non-white (OR = 0.90, 0.84 – 0.95) or insured with Medicare (OR = 0.93, 0.88 – 0.98) or Medicaid (OR = 0.92, 0.85 – 0.99) were less likely to undergo hernia repair with a minimally invasive technique. Patient characteristics that were shown to have no effect on the selection of a minimally invasive technique included an income below the regional median income (OR = 0.99, 0.85 – 1.16) and having an operation completed at an academic center (OR = 0.90, 0.75 – 1.07). Conclusion The optimal surgical approach in ventral hernia repair is influenced by various factors, including age, comorbidities, obesity, and prior abdominal surgeries. These factors can significantly impact postoperative outcomes, potentially justifying the use of an open approach compared to a minimally invasive one, and vice versa. However, disparities related to gender, race, and insurance status suggest existing inequities in current hernia management and care. Addressing these nonclinical disparities is imperative for ensuring more equitable access to newer, possibly more advantageous operative approaches in ventral hernia repair.
Back to 2024 Abstracts