Back to 2024 Abstracts
ENABLING LONG TERM FOLLOW UP AFTER VENTRAL HERNIA REPAIR THROUGH CLINICAL REGISTRY AND MEDICARE DATA LINKAGE
Andrew Varone
*1, Xinyan Zheng
2, Jialin Mao
2, Art Sedrakyan
2, Michael Rosen
3, Benjamin Poulose
11Surgery, The Ohio State University Wexner Medical Center, Columbus, OH; 2Weill Cornell Medicine, New York, NY; 3Cleveland Clinic, Cleveland, OH
Introduction: Long term follow up after ventral hernia repair (VHR) remains elusive. We evaluated the feasibility and success of linking the rich clinical information collected in a disease specific registry with the longitudinal information afforded by administrative claims data.
Methods: Abdominal Core Health Quality Collaborative (ACHQC) patients with Medicare coverage or aged ≥65 were linked to Medicare claims data using a step-wise indirect identifier linkage algorithm for patients undergoing VHR between 2014-2019. Medicare patients without fee-for-service entitlement at the time of hernia repair were excluded as this was required for successful long term follow up linkage. The primary outcome measure was the median number of follow up days for assessment of reoperation for recurrence after the initial operation in patients with both ACHQC and Medicare follow up, compared using Wilcoxon's signed rank test for paired data.
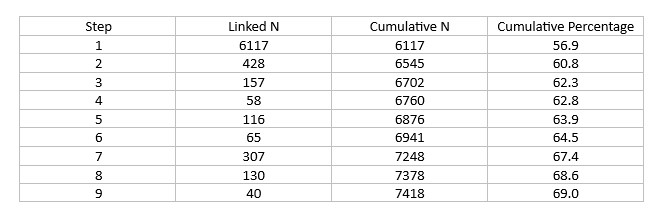
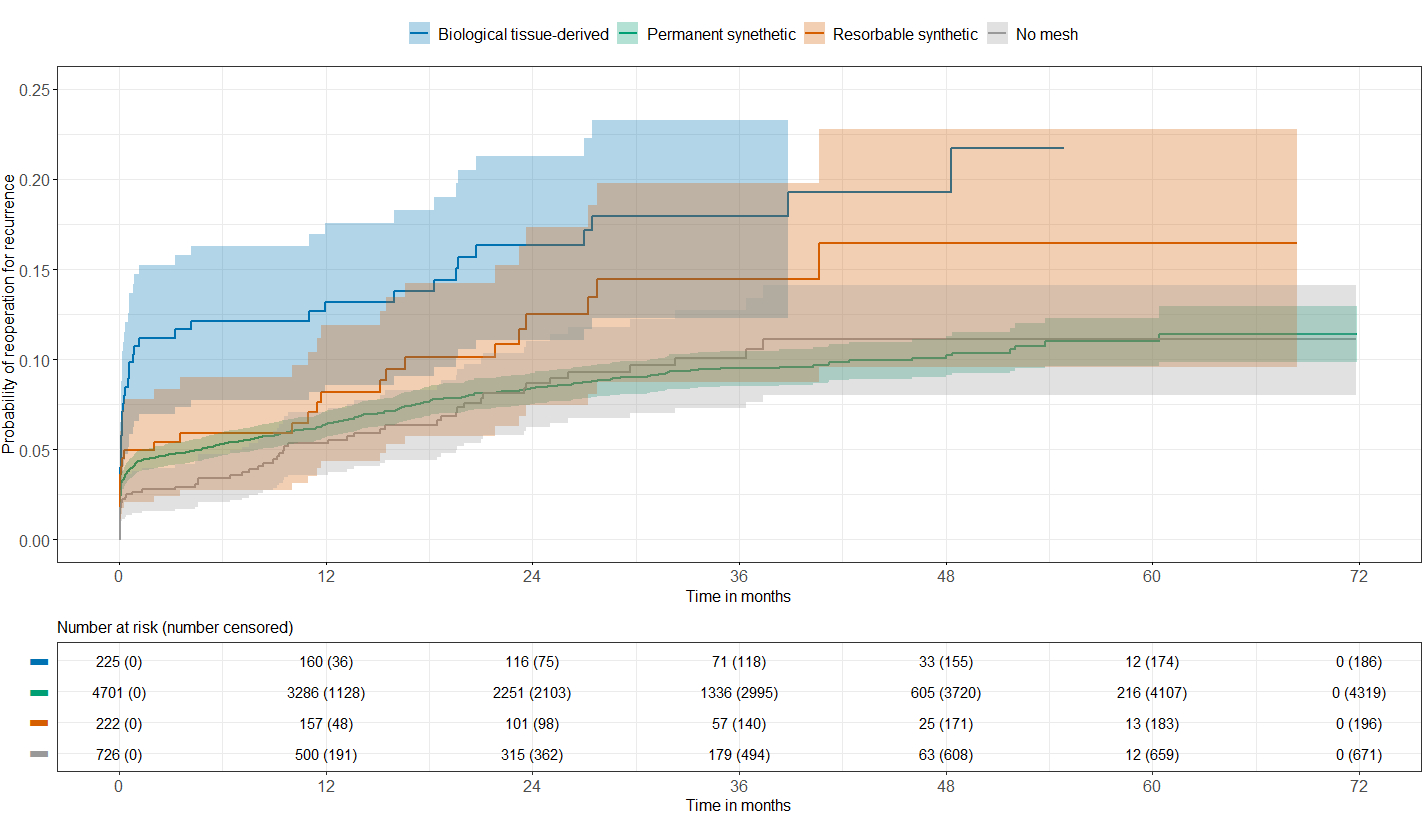
Results: A total of 10,757 patients who underwent VHR were identified in the ACHQC with Medicare coverage or aged ≥65; 7,418 (69%) were successfully linked to Medicare claims data (table 1). 1,532 patients who were not enrolled in fee-for-service Medicare were excluded. A final, linked dataset of 5,886 patients was used for the analysis. Patients had a median age of 69 years (interquartile range (IQR) of 65-74 years) 48% women, 91% white with median body mass index of 30kg/m2 (IQR 27-35kg/m2). Most patients underwent incisional (74%) or umbilical (18%) repair in clean (83%) or clean-contaminated (10%) situations. Mean hernia width was 5cm (IQR 3-10cm) with 31% undergoing recurrent repair. The two most common approaches included open (67%) and robotic (16%) with mesh used in 88% of patients. Myofascial release was performed in 39% achieving a fascial closure rate of 91%. Mesh was used in 88%, of these patients had 91% permanent synthetic, 4% biologic, and 4% resorbable synthetic implanted. Of the 5,319 patients with both ACHQC and Medicare follow up, the median number of follow up days increased from 32d (IQR 18-83d) to 778d (IQR 383-1216) after linkage (p<0.001). At 4 years postop, 89.2% of patients had a probability of not requiring a reoperation for recurrence (Figure 1).
Conclusion: Linking of clinical registry data with administrative claims data can dramatically increase long term follow up after VHR with implications for health services research and post market surveillance of hernia mesh. Future work should focus on developing additional claims-based long term outcomes measures.
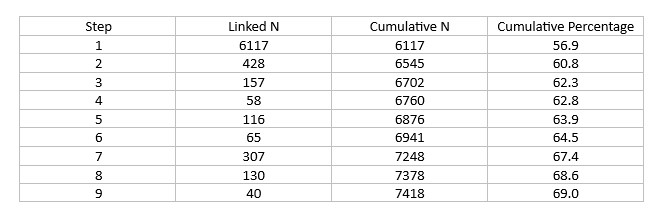
Patients linked by each step of algorithm
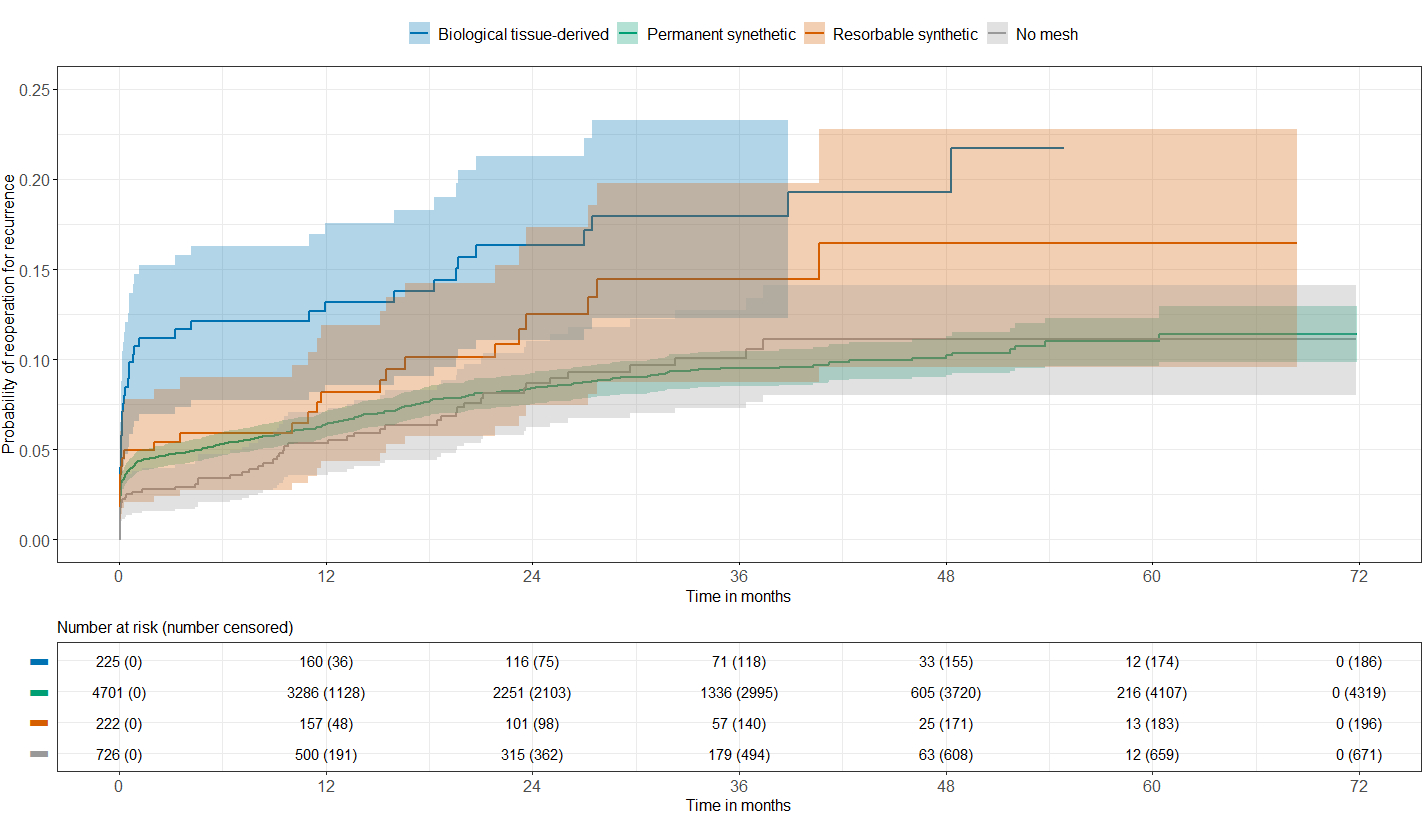
Long term hernia outcomes (p<0.001 log ranked test)
Back to 2024 Abstracts