Back to 2024 Abstracts
SAVE THE SPLEEN OR FIX IT IN FORMALIN: IS THERE A DIFFERENCE IN PERIOPERATIVE OUTCOME?
Kyle A. Lewellen
*, Thomas K. Maatman, Meghan E. Lark, Eugene P. Ceppa, Michael G. House, Alexandra M. Roch, Nicholas J. Zyromski
Indiana University School of Medicine, Indianapolis, IN
BackgroundSplenectomy carries risk of infectious complications. Splenic preservation (SP) avoids these immunologic consequences but is not common surgical practice. When permissible by clinical status and pathology, SP may be acceptable in select patients. Few series have compared outcomes of SP to splenectomy. We hypothesized that surgical splenic preservation has similar operative outcomes to traditional total splenectomy in a matched cohort.
MethodsPropensity score-matched patients undergoing splenic operation as primary procedure between 2012-2021 were obtained via the National Surgical Quality Improvement Program database. Demographics, comorbidities, operative data, and outcomes were captured. Patients undergoing SP (splenorrhaphy or partial splenectomy) were matched in a 1:3 fashion with total splenectomy patients via propensity score matching (PSM) of preoperative variables. Descriptive statistics were applied, along with univariate and multivariable analyses of preoperative associations with major morbidity and mortality.
P-values<0.05 were considered significant.
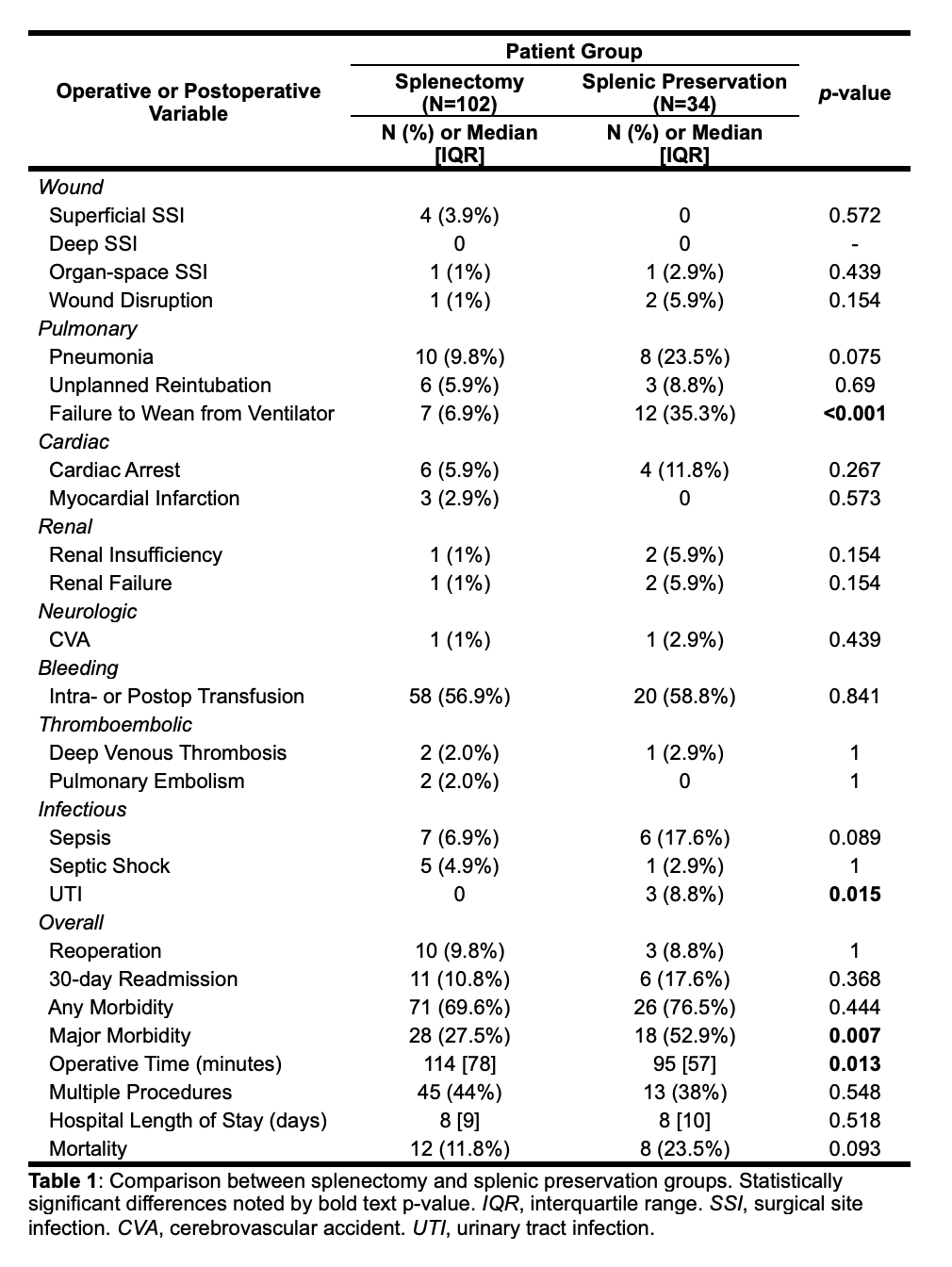
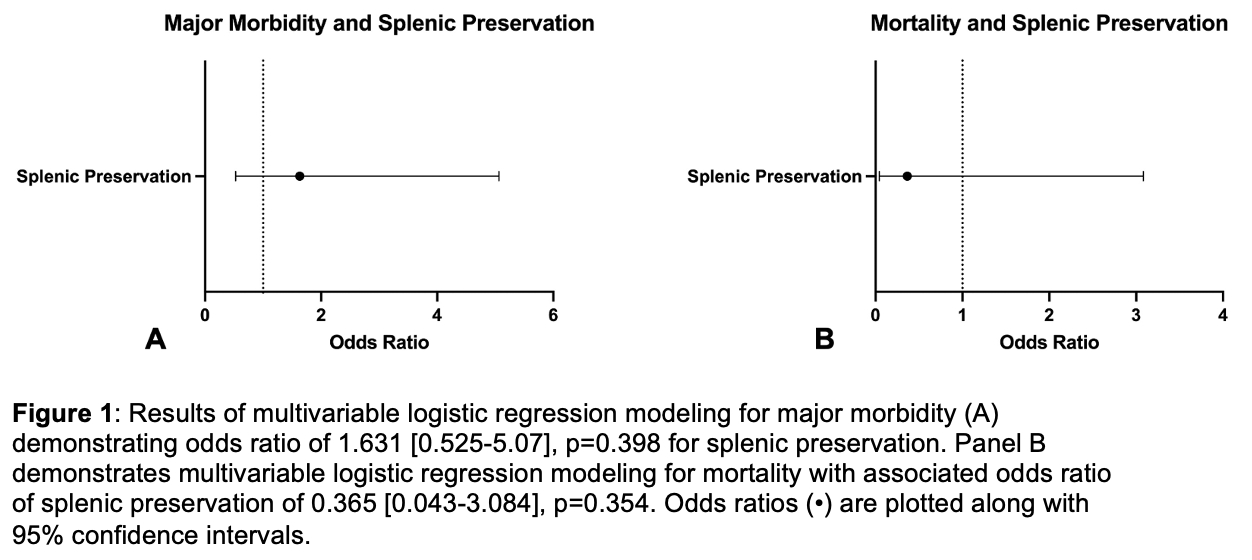
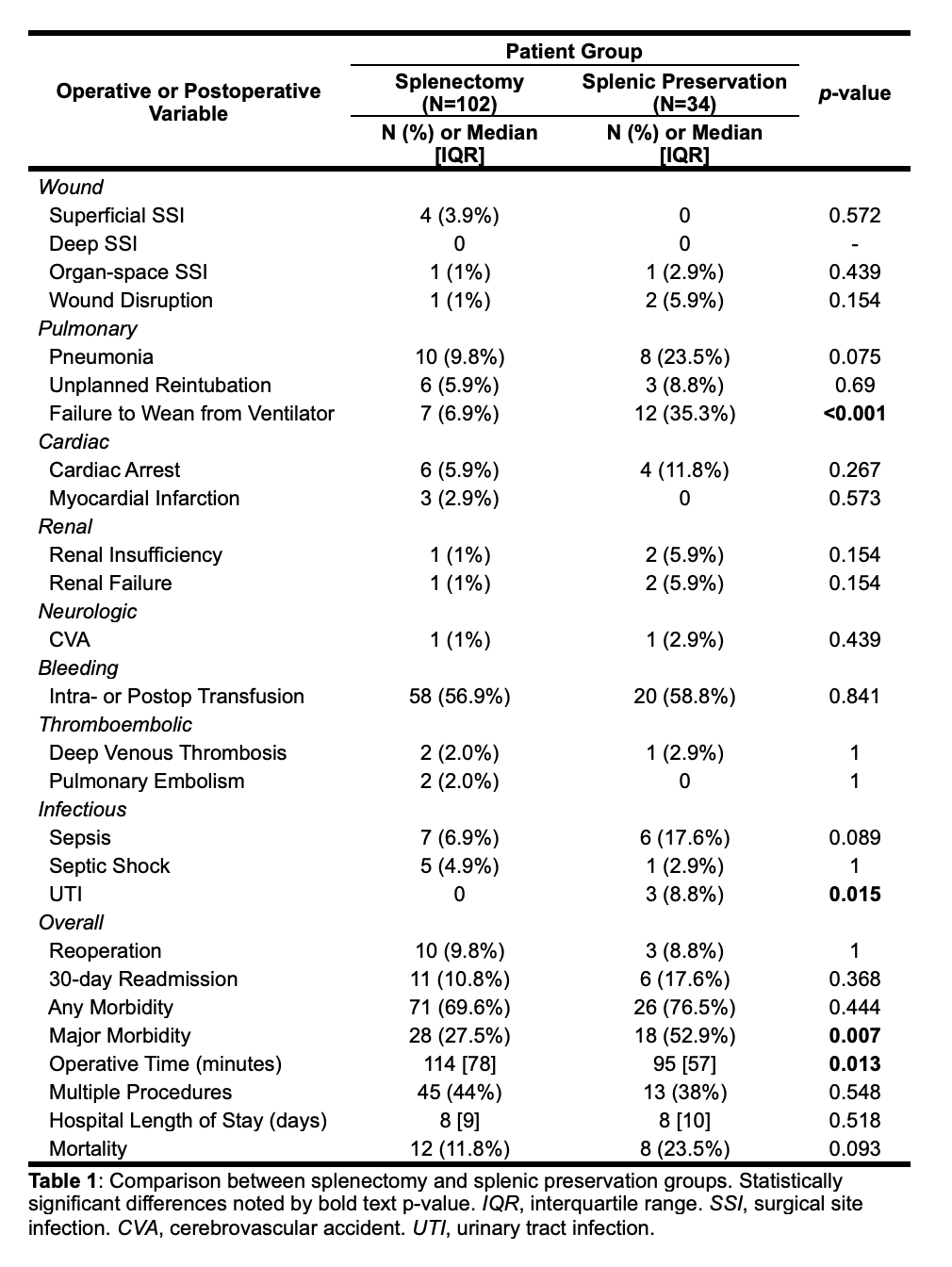
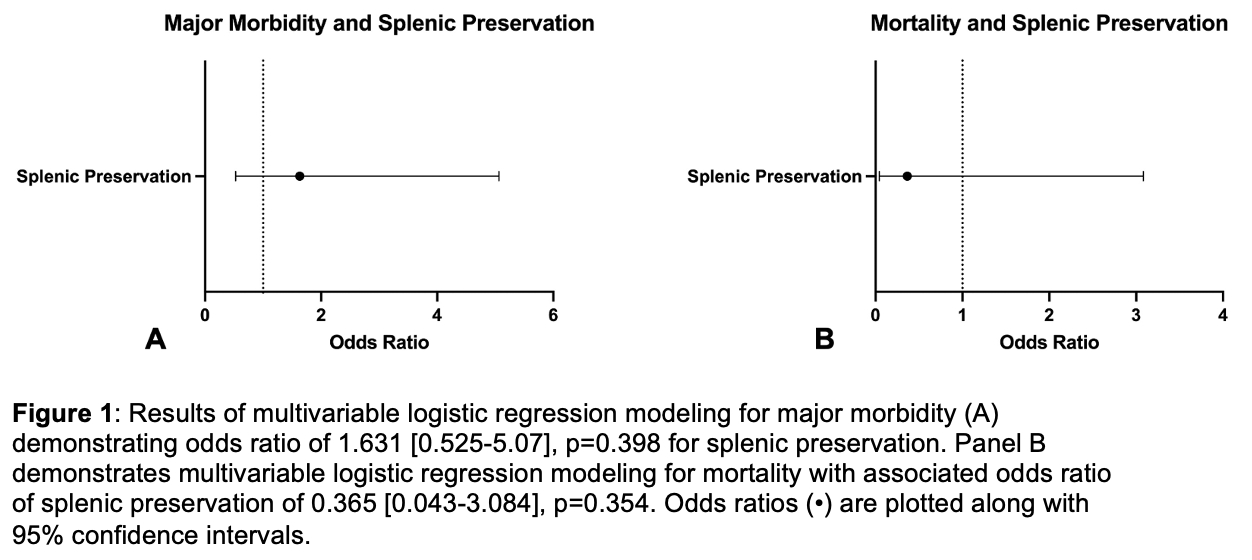
ResultsThe initial query returned 7,410 cases of splenic operations (64 SP). After PSM, 136 cases (102 open total splenectomies, 34 SP) were analyzed after excluding cases which could not be appropriately matched for comorbidities. Median patient age was 59 [IQR 26] years. Few cases (27%) were elective, 40% of patients were American Society of Anesthesiologists Class >3, and 43% underwent multiple procedures at the time of splenic operation. Common indications include splenic injury (26%), hematologic disease (21%), splenic infarct (10%), and splenomegaly (10%). Major morbidity occurred in 34% of patients and mortality rate was 14.7%. Comparison of perioperative outcomes of SP and splenectomy groups are demonstrated in Table 1. On multivariable logistic regression, SP was not associated with major morbidity; odds ratio (OR) 1.631 [95% confidence interval 0.525-5.07]. Elective surgical status was the only preoperative factor significantly associated with decreased odds of major morbidity (OR 0.168 [0.029-0.966], p=0.046). On multivariable logistic regression, SP was not associated with mortality (Figure 1). Patient age (OR 1.154 [1.049-1.269]), preoperative ventilator dependence (54.85 [3.05-986.29]), and preoperative sepsis or septic shock (25.09 [1.95-323.02]) were associated with increased odds of mortality, while independent functional status (0.013 [0.001-0.237]) and preoperative albumin (0.077 [0.012-0.474]) were associated with decreased odds of mortality.
ConclusionThese data demonstrate that in appropriately matched patients, there is no difference in major morbidity or mortality between splenic preservation and splenectomy. When clinical condition of the patient and pathology allow, splenic preservation should be considered to avoid long-term immunologic risks of asplenia.
Back to 2024 Abstracts