Back to 2024 Abstracts
EVIDENCE FOR SURVEILLANCE OF HIGH-RISK LOW-GRADE APPENDICEAL MUCINOUS NEOPLASMS FROM A SINGLE LARGE INSTITUTIONAL STUDY.
Kush R. Lohani
*, EeeLN Buckarma, Hardik Sonani, Hee Eun Lee, Robert A. Vierkant, Cornelius A. Thiels, Travis E. Grotz
Mayo Clinic Minnesota, Rochester, MN
IntroductionLow-grade appendiceal mucinous neoplasms (LAMNs) are epithelial appendiceal neoplasms without infiltrative-type invasion and have potential to progress into pseudomyxoma peritonei (PMP). The benefit of surveillance and risk of recurrence in LAMN is not well established. We aim to highlight the presentation pattern, surgical management, and oncologic outcomes.
MethodsRetrospective review of consecutive patients with LAMN from 1992 to 2023 was conducted. All pathology slides were re-reviewed by an experienced pathologist using 2016 Peritoneal Surface Oncology Group International criteria. The study was limited to LAMNs confined to appendix and those with limited locoregional involvement of the right lower quadrant (RLQ). Cumulative incidence was estimated using Kaplan-Meier curves. Associations of recurrence with risk factors were assessed using Cox proportional hazards regression analyses.
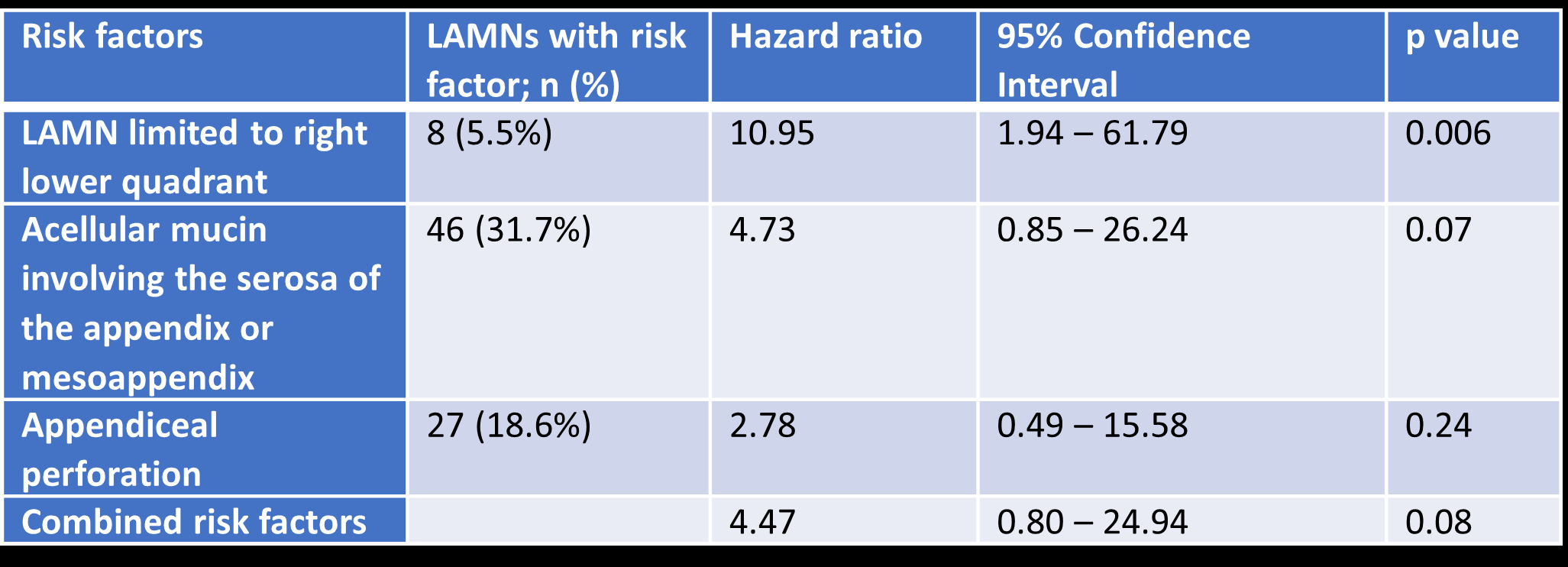
Results145 LAMNs were included in the study (61.3% females, median age=59), of which 91(62.8%) were incidentally found as a mucocele, 39(26.9%) were found at another operation, 13(9%) presented as appendicitis and 2(1.4%) were unspecified. LAMNs most commonly involved the distal tip (n=51, 35.2%) followed by diffuse involvement (n=45, 31%) and least often, the proximal cecal base (n=22, 15.2%). The majority underwent appendectomy (n=103, 71%) followed by right hemicolectomy (n=38, 26.2%), ileocecectomy (n=2, 1.4%) or cecectomy (n=1, 0.7%). 31 LAMNs (21.3%) had concomitant lymphadenectomy but none were involved by LAMN. 11(77.2%) LAMNs were followed in surveillance with abdominal imaging. With a median follow up of 53.5 (IQR=22-119)months, 6/112 (5.4%) LAMNs had recurrence, all of which were within the peritoneum (PMP). Overall, the 5-year and 10-year cumulative incidence of recurrence was 0.05 (95% CI 0.02-0.12) and 0.08 (95% CI 0.03-0.19) respectively. LAMN limited to RLQ was associated with recurrence (
table 1). Acellular mucin involving the serosa and mesoappendix and perforation approached statistical significance. Compared to patients with no risk factors, those with 1 or more risk factors were more than 4 times likely to recur (
table 1). The 5-and 10-year cumulative incidence of recurrence for those without any risk factors was 0.02(95% CI 0-0.08) and 0.06(95% CI 0.01-0.19), respectively. In comparison the 5- and 10-year recurrence cumulative incidence for those with at least one risk factor was 0.12 (95% CI 0.03-0.28) and 0.12 (95% CI 0.03-0.28), respectively.
ConclusionsOverall risk of recurrence for LAMNs after resection is low. Select patients with acellular mucin confined to the RLQ, involving the serosa or mesoappendix, or perforation may be at risk for long-term recurrence. Based on these findings, patients with high-risk LAMNs should be surveilled for at least 10 years and LAMNs without risk factors should be followed up expectantly.
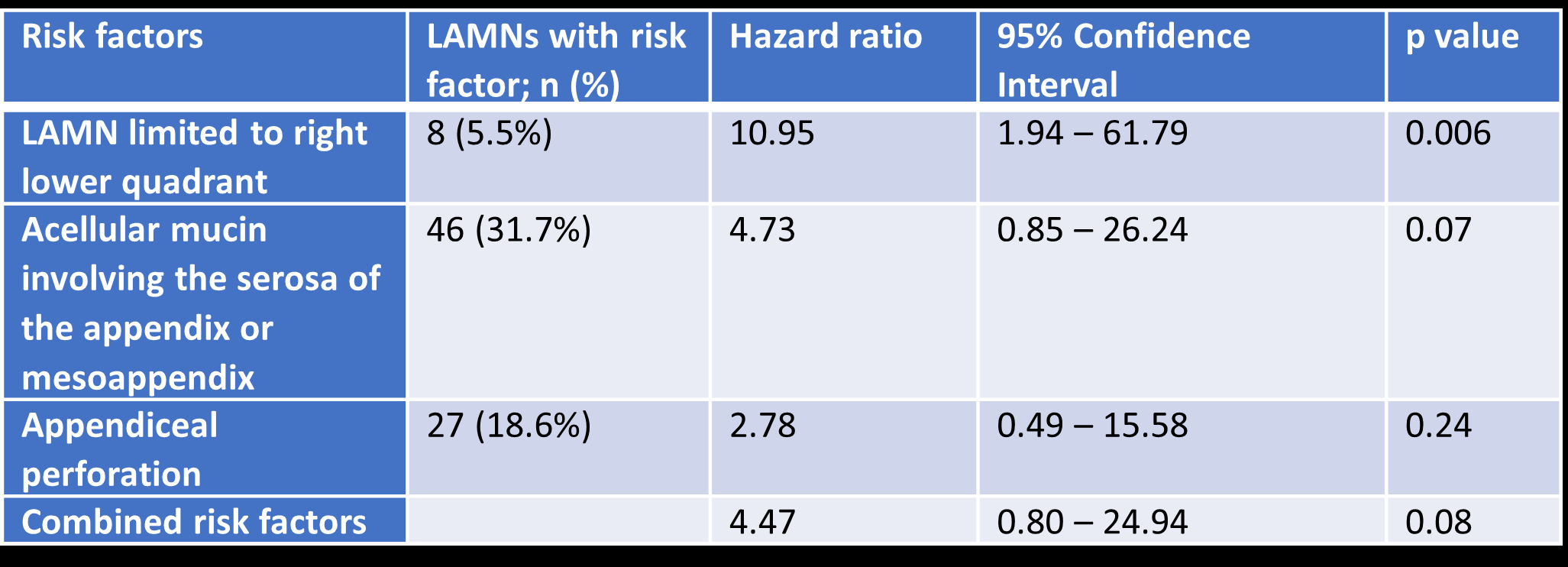 Table 1
Table 1. Clinicopathological risk factors for low-grade appendiceal mucinous neoplasm (LAMN) recurrence.
Back to 2024 Abstracts