Back to 2024 Abstracts
THE IMPACT OF PATHOLOGICAL TUMOR RESPONSE FOLLOWING NEOADJUVANT CHEMOTHERAPY AND CHEMORADIOTHERAPY FOR ESOPHAGEAL ADENOCARCINOMA. A RETROSPECTIVE MULTICENTER COHORT STUDY
Giovanni Capovilla
*1, Alessia Scarton
1, Elisa Sciuto
1, Lucia Moletta
1, Elisa Sefora Pierobon
1, Gianpietro Zanchettin
1, Federica Riccio
1, Luca Provenzano
1, Renato Salvador
1, Felix Berlth
2, Evangelos Tagkalos
2, Eren Uzun
2, Carlo Alberto De Pasqual
3, Cecilia Turolo
3, Jacopo Weindelmayer
3, Simone Giacopuzzi
3, Giovanni De Manzoni
3, Peter P. Grimminger
2, Michele Valmasoni
11Department of Surgical, Oncological and Gastroenterological Sciences, University of Padova, Padova, Italy; 2Universitatsmedizin der Johannes Gutenberg-Universitat Mainz Klinik fur Allgemein- Viszeral- und Transplantationschirurgie, Mainz, Rheinland-Pfalz, Germany; 3Azienda Ospedaliera Universitaria Integrata Verona, Verona, Veneto, Italy
BackgroundTwo multimodal strategies are available for the treatment of esophageal cancer: neoadjuvant chemotherapy (nCT) and chemoradiotherapy (nCRT). The higher rate of pathological complete response (pCR) after nCRT is an argument to support this treatment. However, previous studies have failed to demonstrate a survival benefit of nCRT for adenocarcinoma (ADC) and the correlation between pathological tumor response (pTR) and survival is unclear. Primary aim of the study was to verify whether the prognosis of patients with ADC after radical surgery is influenced by the type of neoadjuvant treatment performed. Secondary endpoint was to determine whether the survival benefit associated with a complete tumor regression could be achieved also with a major, albeit subtotal, tumor response.
MethodsThis study included data from 3 high-volume centers. Only patients with ADC who underwent nCT or nCRT and surgery between 2015 and 2022 were included. The correlation between pTR and overall (OS) and disease-free survivals (DFS) after both treatments was evaluated using Kaplan-Meier analysis. pTR was assessed using the Mandard tumor regression grade (TRG). Patients with cT4b or cM+ cancer, R1 or R2 resections and a non-adequate lymphadenectomy (< 12) were excluded. nCT was defined as systemic perioperative regimens including at least 2 drugs. nCRT was defined as preoperative regimens including at least 2 drugs and at least 41.4 Gy of radiation.
ResultsOverall, 563 patients were included, 278 received nCT and 285 nCRT. The incidence of pCR was 11.2% (31/278) in the nCT group and 24.6% (70/285) after nCRT (p < 0.0001).
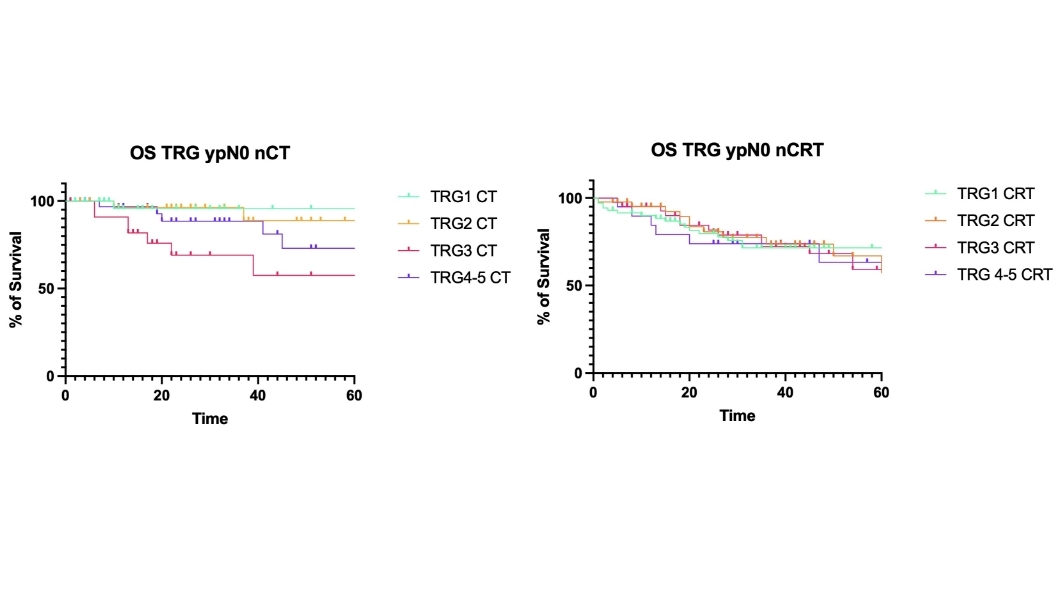
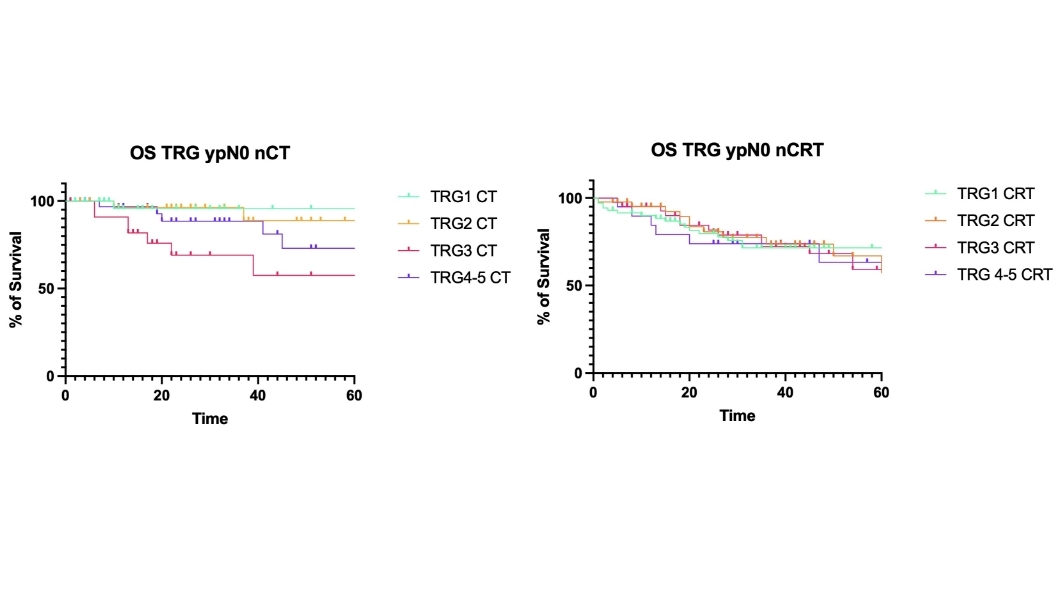
At 5-years the OS rate after nCT for patients ypN0 was 95% for TRG1 patients, 88% for TRG2, 57% for TRG3 and 58% for TRG4-5 (p=0.03). After nCRT it was 71.3 % for TRG1, 57.3 %for TRG2, 59% for TRG3 and 63% for TRG4-5 (p=ns). The OS of patients with pCR was not significantly different after nCT and nCRT (p=0.61) but at 5 years the OS for pCR after nCT was 95% vs 71.3%. after nCRT (figure 1). The 5-years DFS of pCR patients was higher in the nCT group (84% vs. 66.5%, p=0.05).
The incidence of disease recurrence was not significantly different between nCT and nCRT (36.4% vs 44%, p=0.09). However, the proportion of patients showing distant recurrences was significantly higher in che nCRT group (35.4% vs 23.8%, p=0.009).
TRG 1 and 2 showed comparable OS curves both in the nCT group (p=0.76) and in the nCRT group (p=0.82). TRG 1-2 were associated with a significantly improved OS compared to TRG 3-5 after nCT (p=0.004) and nCRT (p=0.0003).
ConclusionTRG showed to be significantly associated with survival in patients treated with nCT, but not with nCRT. Despite a lower rate of pCR, both OS and, especially, DFS of pCR patients were improved after nCT compared to nCRT. The survival outcome was comparable between TRG 1 and TRG 2 patients after nCT and nCRT.
Back to 2024 Abstracts